 Want to receive Best Practice Bulletin directly to your inbox?
Sign up here.
Want to receive Best Practice Bulletin directly to your inbox?
Sign up here.
Published: 8th August, 2025
Contents
New from bpacnz: Clinical Audit - Recovery at Work

“Fit for selected work” should generally be the first consideration for most injured patients who are not “Fully fit” for work when issuing a medical certificate. This is based on the idea that, like over-prescribing a medicine, prescribing a patient too much time off work can detrimentally affect their health and vocational and social outcomes, without providing any added benefit to recovery.
This audit helps healthcare professionals to consider their decision-making about work-related medical certificates in the past 12 months, to assess whether the designation, and the overall proportion of “Fully unfit” medical certificates issued was appropriate.
 A “working audit” option is also provided, where data are collected over time when an eligible patient presents following an accident resulting in injury. This format may be better suited to locums or urgent care clinicians, or other healthcare professionals who prefer a different approach to identifying eligible patients.
A “working audit” option is also provided, where data are collected over time when an eligible patient presents following an accident resulting in injury. This format may be better suited to locums or urgent care clinicians, or other healthcare professionals who prefer a different approach to identifying eligible patients.
View the audit here.
Read the comprehensive Recovery at Work guide, here. A B-QuiCK summary, case study quiz and peer group discussion are also available.
 Coming soon – Navigating the Recovery at Work process: the podcast
Coming soon – Navigating the Recovery at Work process: the podcast
During the development of ACC Recovery at Work resources, we realised that we still had questions, and after we started publishing, it was evident that our primary care audience had questions too.
We recently hosted a panel discussion with representatives from ACC to clarify and expand on some aspects of the Recovery at Work programme. To prepare for this discussion, a group of primary care specialists - general practitioners, urgent care clinicians and nurse practitioners - were invited to participate in a written interview, and we asked them about their experiences with the Recovery at Work programme. The common threads from their responses were then used to inform and direct the panel discussion. Our podcast is now in final production and due to be published soon.
Click here for a sneak peek…
“It's really important that the [primary care] sector knows that you have strategic importance to ACC, you're the main entry point into this scheme. Primary care providers sign off the majority of the work certificates and those are really quite key interactions for ACC. They can either put the handbrake on recovery or they can support an early reintegration into the workplace.”
“[Vocational] providers are telling us that they're willing and able and really want to engage with you. They've identified that the inability to connect with the GP is actually a pretty significant barrier for getting people back to work. In my time as a provider it was absolute gold dust to have those open communication channels with GPs, especially for those curlier situations.”
“As an organisation our current focus is to work with the health sector and commission for services and find new ways of being able to work better together with you as a primary care sector, and for us to improve these recovery outcomes. We need to do this not only to ensure that we're not causing any harm to patients, but also ensuring that there's sustainability for you and for us.”
In case you missed it: Gout case study quiz
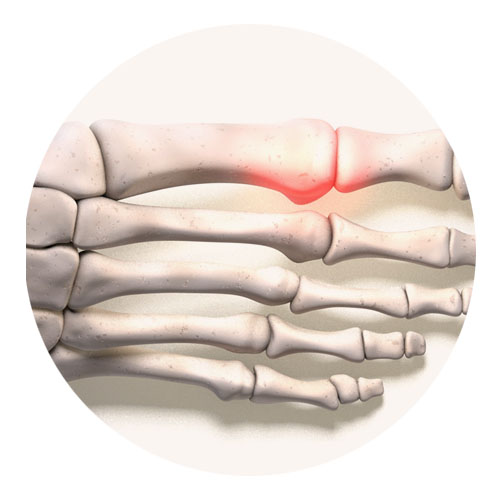
bpacnz recently published an interactive case study quiz on gout, following the story of Malo Fuimaono, a 47-year-old male who presents with severe pain in his right big toe. What can you do to help Malo? Do you feel confident that you can set Malo on a positive path towards long-term symptom control? Will you make the right call on the “extra for experts” scenario? Test your knowledge with the case study quiz here* and earn CPD points.
* You will need to log-in to “My bpac” or create a free account
Read the full article on gout, here. A B-QuiCK summary, clinical audit and peer group discussion are also available.
Medicine news: ferrous sulfate, fexofenadine, oxycodone, Ultraproct, Mirena, Jaydess, inhalers
The following news relating to medicine supply has recently been announced. These items are selected based on their relevance to primary care and where issues for patients are anticipated, e.g. no alternative medicine available or changing to the alternative presents issues. Information about medicine supply is available in the New Zealand Formulary at the top of the individual monograph for any affected medicine and summarised here.
Pharmac has announced a supply issue affecting ferrous sulfate 325 mg modified-release tablets (Ferrograd). This medicine is expected to go out of stock in early September and no alternative brand is available. No new patients can be prescribed ferrous sulfate tablets from 1st September, 2025, and this formulation will be delisted from the Pharmaceutical Schedule on 1st March, 2026. This supply issue has occurred due to a change in manufacturer and price.
Ferrous fumarate 200 mg (Ferro-tab) is an alternative iron tablet that can be prescribed. As it is an immediate-release formulation, some patients may require dosing up to three times daily, as opposed to once daily with modified-release ferrous sulfate (see NZF for dosing instructions). However, ferrous fumarate may be better tolerated by some patients.
Pharmac is offering prescribers and patients an opportunity to provide feedback on the impact that the delisting of ferrous sulfate will have, and whether any additional support is required. Feedback can be emailed to: consult@pharmac.govt.nz by 5 pm, Thursday, 14th August.
Supply issue affecting fexofenadine 120 mg tablets
There is a supply issue affecting stock of fexofenadine 120 mg tablets (Fexaclear) due to a change in packaging. Re-supply of fexofenadine with the new packaging is expected from September, 2025. Alternative funded products are available, e.g. fexofenadine 180 mg tablets and cetirizine 10 mg tablets,* however, a new prescription will be required. Fexofenadine 60 mg tablets are also a suitable alternative and a new prescription may not be needed, but these are only partly funded. Fexofenadine 120 mg and 180 tablets have been fully funded since February, 2025 (as reported in Bulletin 108).
* Loratadine 10 mg tablets are also a suitable alternative, but are currently affected by a supply issue (as reported in Bulletin 121)
There is an ongoing supply issue affecting stock of 5 mg, 10 mg and 20 mg oxycodone immediate-release tablets (as last reported in Bulletin 125). The supplier is currently out of stock of 5 mg tablets, while stock of 10 mg and 20 mg tablets is low. Re-supply of all strengths has now been delayed until September (re-supply was previously expected in August); supply of 10 mg and 20 mg tablets may run out before new stock arrives. Oxycodone 1 mg/mL oral liquid is available (a new prescription will be required), but clinicians are advised to consider prescribing an alternative analgesic.
Pharmac has also announced that 40 mg oxycodone controlled-release tablets (Oxycodone Sandoz) are out of stock with the supplier. Clinicians are advised to prescribe lower strength tablets to make up the equivalent dose, however, stock of the 20 mg oxycodone controlled-release tablets is reportedly low. Re-supply of the 20 mg and 40 mg tablets is expected by mid-August.
Ultraproct supply update
Pharmac announced in April that stock of Ultraproct (fluocortolone caproate with fluocortolone pivalate and cinchocaine) suppositories and ointment would be affected by a supply issue due to manufacturing delays (as reported in Bulletin 121). Ultraproct suppositories are currently out of stock, and stock of the ointment is now expected to be exhausted by mid-August (previously it was expected to be out of stock from September). The supply issue is likely to continue until the end of 2025. An alternative funded product, Proctosedyl (hydrocortisone with cinchocaine), is available in both formulations, however, a new prescription will be required as the active ingredient is different.
A patient information handout about supply issues in general is available, here.
Schedule reminders: Mirena and Jaydess available on PSO, improved access to budesonisde with eformoterol inhalers
As of 1st August:
- The intrauterine systems, Mirena and Jaydess, are now available on PSO (see Bulletin 127 for more details). Up to 25 Mirena devices and up to ten Jaydess devices can be ordered. The number of Jadelle subdermal implants has also increased from three to 20 packs (each pack contains two rods for implant).
- Patients can now collect up to three months’ supply of selected budesonide with eformoterol inhalers, used in AIR/SMART therapy, at once. These inhalers are also available on PSO in limited quantities. See Bulletin 127 for further details, including information on the strengths of inhaler this change applies to.
Widened access to meningococcal B vaccine for children aged under five years
Pharmac has announced that from 1st September, 2025, access to the meningococcal B vaccine (Bexsero) will be widened to include all children aged under five years. Currently, meningococcal B vaccination is funded for children up to age 12 months as part of the childhood immunisation programme; it is scheduled to be given as three doses, usually at ages three, five and 12 months. The timing of administration remains the same. A catch-up meningococcal B vaccination programme has also been available for children aged 13 – 59 months since March, 2023 (as reported in Bulletin 65), but ends on 31st August, 2025. This change will replace the current catch-up programme, and means that all children aged under five years will be able to complete the full meningococcal B vaccination course if it was not done within the first 12 months of life.
Eligibility criteria for funded meningococcal B vaccination for older children and adults at high risk remain the same; click here for funding criteria.
Dengue cases on the rise
Te Whatu Ora, Health New Zealand, is raising awareness of dengue following a recent surge in cases involving people who have recently returned to New Zealand from overseas, particularly Pacific countries. In all cases, the infection was acquired in another country; there are no mosquitoes in New Zealand that are able to transmit the dengue virus, and it cannot be transmitted from person to person.
Read more about dengue symptoms
Most people infected with the dengue virus are asymptomatic or have mild symptoms that last for up to seven days. However, in some cases significant illness can occur, known as severe dengue, which can cause dengue haemorrhagic fever. Severe dengue typically develops within five days of mild symptoms first appearing and is more common in people who have previously been infected with the dengue virus. These patients require acute secondary care referral.
Initial symptoms and signs of dengue may include: |
Signs of severe dengue include: |
- Nausea and vomiting
- Sudden onset of high fever
- Headaches
- Fatigue
- Retro-orbital pain
- Myalgia or arthralgia
- Fine rash on the extremities (may be pruritic)
|
- Persistent vomiting
- Severe abdominal pain
- Mucosal bleeding
- Hepatomegaly
- Fluid accumulation
|
In a recent communication to the sector, the National Public Health Service is asking healthcare professionals to consider the possibility of dengue in patients who present with relevant symptoms and a history of recent overseas travel (within three weeks), and to notify the local Medical Officer of Health on suspicion of dengue. Relevant laboratory tests include full blood count and dengue serology. Clinicians should also ensure that patients with upcoming international travel to areas where dengue is widespread, e.g. Pacific islands, are aware to take precautions to avoid being bitten by mosquitoes.
Monitoring Communication update: Anti-CD20 monoclonal antibodies and pyoderma gangrenosum
In January, 2025, Medsafe asked clinicians to report any possible cases of pyoderma gangrenosum, a rare inflammatory skin condition, in patients administered anti-CD20 monoclonal antibodies, e.g. rituximab, ocrelizumab, obinutuzumab (as reported in Bulletin 115). The reporting period has now ended, and the Centre for Adverse Reactions Monitoring (CARM) did not receive any case reports (16th January – 16th July, 2025). On balance, Medsafe advises that the benefit/risk ratio for anti-CD20 monoclonal antibodies remains positive at this stage.
Upcoming changes to the Community Referred Radiology programme
It has been reported that Te Whatu Ora, Health New Zealand, is implementing mandatory national criteria for Community Referred Radiology from 1st September, 2025. This is a phased rollout that will replace regional frameworks and is intended to standardise access to imaging across New Zealand and improve equity of care. As part of this, the scope of referrers is reportedly being widened.
This will mean that general practitioners, urgent care doctors and nurse practitioners will be able to refer patients directly for certain types of imaging (including CT), without the patient needing hospital specialist assessment or emergency department referral. Specific referral criteria and timeframes for prioritisation have been developed and are available here. This includes the clinical criteria required for requesting diagnostic X-rays, ultrasound and CT imaging in both adults and children. N.B. Imaging that is covered under other funding streams, e.g. ACC, primary maternity services, is excluded. Any imaging required as part of a screening or surveillance programme is also not included.
A webinar on navigating the new radiology programme is being held by the Goodfellow Unit on Tuesday, 30th September, from 7:30 – 8:45 pm. Find out more here.
NZF updates for August
Significant changes to the NZF in the August, 2025, release include:
- Hydrocortisone butyrate (Locoid) has been reclassified from a potent to moderate potency topical corticosteroid
- A new section on teratogenic medicines and pregnancy prevention has been added to the therapeutic notes for contraceptives
- Updates to the following sections in the hypertension therapeutic notes: drug treatment of hypertension, hypertension in older people, hypertension in diabetes, hypertension in renal disease and hypertensive crisis
- All sections in the anti-seizure medicine (ASM) therapeutic notes have been updated; a new table has also been added on anti-seizure medicine choice based on seizure-type
- A new monograph has been added for lemborexant (Section 29, not funded), indicated for insomnia characterised by difficulties with sleep onset and/or sleep maintenance
- Cautions, pre-treatment screening, monitoring, adverse effects and patient advice have been updated in the carbamazepine monograph
- Hyperthermia has been added as a serious adverse effect to the hyoscine hydrobromide. Patient advice has also been added.
- Indications and dose regimens have been updated in the following monographs to align with revised New Zealand acute rheumatic fever and rheumatic heart disease guidelines: amoxicillin, phenoxymethylpenicillin, erythromycin, roxithromycin, clindamycin, amoxicillin + clavulanic acid and rifampicin
- History of nitrofurantoin-induced hepatotoxicity or pulmonary toxicity has been added as a contraindication to nitrofurantoin. Cautions (hepatic dysfunction – may mask signs and symptoms of nitrofurantoin-induced hepatotoxicity has been added as a caution), monitoring, hepatic impairment, adverse effects and patient advice have also been updated.
You can read about all the changes in the August release, here. Also read about any significant changes to the NZF for Children (NZFC), here.
 Practice Focus: Understanding diagnostic overshadowing
Practice Focus: Understanding diagnostic overshadowing
A new resource for primary care clinicians on understanding diagnostic overshadowing has been developed by Te Pou and the Tupuānuku and Te Pu Korokoro researchers at the University of Otago. Diagnostic overshadowing describes the situation in which a person’s symptoms are misattributed to their pre-existing mental health or substance use condition diagnosis, rather than exploring the possibility of a co-occurring physical health condition. This can result in delayed diagnosis and treatment for physical health conditions. The purpose of the resource, which is in the format of a short slidedeck, is to highlight this clinical phenomenon and to provide strategies for overcoming it.
Read more
The resource, Improving primary care for people with mental health or substance use conditions, highlights strategies for clinicians to recognise overshadowing to ensure that people with mental health or substance use conditions receive the same level of care as those who do not. For example, ensuring that new symptoms in people with a history of mental health conditions or substance use are fully assessed without any pre-determined diagnosis or attribution for the symptoms. Support and advice on how to understand and manage symptoms should be provided to the patient even if no clear cause is found. Also consider reflecting on your own thinking, including assumptions about mental health or substance use conditions, and auditing your practice, e.g. compare screening, referrals and treatment rates between patients with a mental health or substance use condition and those without.
View the full resource here. A short (three minute) patient-focused video on understanding overshadowing is also available here (this resource may also be useful for healthcare professionals).
Medical Council survey on Good Medical Practice statement
The Medical Council of New Zealand is in the process of reviewing its official statement on Good Medical Practice, and has released a survey seeking feedback on how the statement is currently used, which aspects are most useful and areas that could be improved. The findings from the survey are expected to help inform the revised draft, which will then go out for consultation. The survey closes on Friday, 15th August. Complete the survey here.

See you in Christchurch?
If you are going to Christchurch next week for the GP CME conference, you are warmly welcomed to come meet some of the bpacnz Publications Team at the South Link Education Trust stand. We would love to talk to you about our educational resources, as well as other exciting opportunities and products in development by the wider South Link Health and BPAC Clinical Solutions teams.
 Paper of the Week: Optimising LDL-C post-ACS – is there room for improvement?
Paper of the Week: Optimising LDL-C post-ACS – is there room for improvement?
The benefits of lowering LDL-C in people with increased cardiovascular disease risk are widely accepted. The 2025 National Heart Foundation of Australia & Cardiac Society of Australia and New Zealand guideline for diagnosing and managing acute coronary syndromes (ACS) recommends that people with a history of ACS aim for a LDL-C level < 1.4 mmol/L and a reduction of ≥ 50% from baseline. This aligns with other international cardiovascular guidelines. Almost all patients will require pharmacological intervention to achieve this LDL-C level and high-intensity statin treatment, which lowers LDL-C by an average of ≥ 50% from baseline, is widely recommended for this purpose.
A study published in the New Zealand Medical Journal assessed the relationship between statin intensity, treatment adherence and LDL-C levels in patients discharged from hospital following their first ACS. More than three-quarters of patients were discharged on high-intensity statin treatment. However, 21% of patients did not have repeat lipid measurements at any point in the year post-discharge and of those with repeat lipid tests, only one in four achieved the current recommended LDL-C target. Of the patients that did not achieve a LDL-C level < 1.4 mmol/L, three-quarters did not receive any statin dose adjustments during the 12 months post-ACS.
While these findings imply there is a need for more active management of patients post-ACS in the short-term to reduce the risk of future cardiovascular events, published commentary from Gray, 2025, questions the usefulness of serial monitoring of LDL-C levels.
What are your thoughts on intensifying statin treatment and measuring LDL-C in patients post-ACS? Would you make dose adjustments or switch lipid-lowering medicines without first checking LDL-C levels? How often do your patients achieve the guideline recommended LDL-C targets? In your experience, does tolerance often limit the ability to achieve targets?
Read more
- The study involved analysis of the records of 13,202 patients hospitalised with their first ACS in the Northern region of New Zealand between 2014 – 2019. Most patients had a LDL-C level ≥ 1.8 mmol/L at hospital admission (median 2.6 mmol/L, interquartile range 1.8 – 3.4 mmol/L).
- 70% of the patients were male
- Mean age was 65 years
- The proportion of patients by ethnicity was: European/Other (64%), Māori (11%), Pacific peoples (10%) and Indian/Other Asian (15%)
- 78.7% of patients had at least one follow-up LDL-C level measured between 30 days and one year after being discharged from hospital; 42.4% had at least two tests
- Studies have shown that follow-up lipid assessment after ACS increases the likelihood of statin up-titration and the patient achieving the LDL-C target level. International guidelines recommend measuring LDL-C levels 4 – 12 weeks following statin initiation and again within 6 – 12 months.
- Approximately 8,000 patients (76.1%) did not achieve the LDL-C target level (< 1.4 mmol/L) within 12 months post-ACS
- Three-quarters of these patients did not receive any statin dose adjustments during that period
- Lower LDL-C levels were more likely in patients with better adherence
- Evaluated using a medication possession ratio (MPR), based on the quantity of medicines dispensed divided by the number of days since hospital discharge; MPR ≥ 1.0 is optimal adherence, MPR ≥ 0.8 is satisfactory, MPR = 0 is no adherence
- Those with a MPR = 1.0 had an average LDL-C of 1.73 mmol/L, compared to 1.91 mmol/L for patients with a MPR 0.8 – 1.0 and 2.39 mmol/L for a MPR < 0.8
- Patients with better medicines adherence may also be more likely to implement and maintain lifestyle changes which may also contribute to the observed effect on LDL-C levels, i.e. the “healthy adherer” effect
- Notably, only 29% of patients who received high-intensity statin treatment and had optimal adherence (MPR ≥ 1.0) achieved the LDL-C target level. This suggests that high-intensity statin treatment alone is not sufficient to achieve LDL-C target levels in a large subset of the general population and further interventions, e.g. PCSK9 inhibitors (not available in New Zealand), are likely to be required to achieve guideline recommended targets.
- Newer guidelines are recommending even lower LDL-C targets for patients with recurrent cardiovascular events, e.g. < 1.1 mmol/L (European Society of Cardiology), however, the authors of the study acknowledge this may be difficult to achieve for some individuals with the current medicines available, such as those with higher baseline LDL-C levels, and ultimately may be demotivating
- Rosuvastatin, a high-intensity statin, was not funded in New Zealand during the study period. Ezetimibe was funded with Special Authority approval.
- Ezetimibe (in combination with a statin) was prescribed to 2.4% of patients discharged from hospital (and who underwent follow-up LDL-C measurement). This increased to 5.6% by one year after discharge in the LDL-C measurement group.
- Rosuvastatin was funded with Special Authority approval in 2021 and funding restrictions on ezetimibe were removed in 2023, now giving primary care prescribers more options to help patients achieve lower LDL-C levels
- Lipid management is not limited to pharmacological intervention. Lifestyle changes, e.g. limiting intake of dietary saturated fat, regular exercise, and referral for cardiac rehabilitation are critical to reduce the risk of future cardiovascular events.
- Study limitations include the assumption that the dispensed medicines were taken correctly by the patient and that the exclusion of patients with more than one episode of ACS may mean these findings are not generalisable to all patient populations who likely benefit from LDL-C reduction
A response to this study from Associate Professor Ben Gray, Primary Healthcare and General Practice, was subsequently published in the New Zealand Medical Journal. Associate Professor Gray agrees that initiating the highest tolerated statin dose is valuable post-ACS but disputes the value of serial LDL-C measurements for titrating doses or adding ezetimibe because biological variation in individual LDL-C test results is not accounted for. The key points made to support this argument are:
- The reference change value, i.e. the percentage change required for two serial measurements to be considered different, is within 21 – 30% for LDL-C measurements
- The initiation of 10 – 20 mg statin dose will reduce LDL-C by 30 – 35%, however, increasing the statin dose to 40 – 80 mg will likely only result in ~10% reduction in LDL-C. This subsequent LDL-C reduction is below the reference change value, making it potentially misleading.
- Serial LDL-C monitoring, is therefore only useful for measuring adherence to statin treatment, but this is often better assessed through discussion with the patient
Professor Andrew Kerr, Cardiologist and an author of the study, agrees with the points made above, but reiterates that “serial LDL estimations can be an important tool as part of the shared decision-making process: both to identify patients not consistently meeting treatment targets for review regarding whether medication can be further intensified, and for review of adherence to lifestyle and medications”.
He J, Lee M, Kerr A. Low-density lipoprotein cholesterol management after acute coronary syndrome in Aotearoa New Zealand: opportunities for improvement (ANZACS-QI 81). NZMJ 2025;138:60–74. doi:10.26635/6965.6818.
Gray B, Kerr A. Measuring low-density lipoprotein cholesterol and Response to: ‘Measuring low-density lipoprotein cholesterol’. NZMJ 2025;138:71–4. doi:10.26635/6965.7120.
For further information on managing lipid levels and other cardiovascular risk factors following ACS in primary care, see: https://bpac.org.nz/2025/acs.aspx
For further information on prescribing statins in primary care, see: https://bpac.org.nz/2021/statins.aspx and https://bpac.org.nz/2022/rosuvastatin.aspx
 This Bulletin is supported by the South Link Education Trust
This Bulletin is supported by the South Link Education Trust
If you have any information you would like us to add to our next bulletin, please email:
editor@bpac.org.nz
© This resource is the subject of copyright which is owned by bpacnz. You may access it, but you may not reproduce it or any part of it except in the limited situations described in the terms of use on our website.
