 Want to receive Best Practice Bulletin directly to your inbox?
Sign up here.
Want to receive Best Practice Bulletin directly to your inbox?
Sign up here.
Published: 17 March, 2023
Contents
New multimedia slidecast - Osteoarthritis: a focus on exercise

Three main aspects form the foundation of a management strategy for patients with osteoarthritis: education, exercise and weight loss. Other interventions can then be progressively added as required, such as analgesia with NSAIDs or paracetamol.
Bpacnz has recently published a 20-minute multimedia slidecast, exploring the role of exercise in improving pain or loss of function associated with osteoarthritis. To help navigate this topic, we are joined in this narrated slideshow by physiotherapist Associate Professor Ben Darlow (University of Otago, Wellington) and orthopaedic surgeon Mr John Scanelli (Te Whatu Ora Southern; Senior Clinical Lecturer, Dunedin School of Medicine, University of Otago).
View the slidecast here. Printable key practice points are also available here.
In case you missed it – Endometrial cancer: early detection and referral
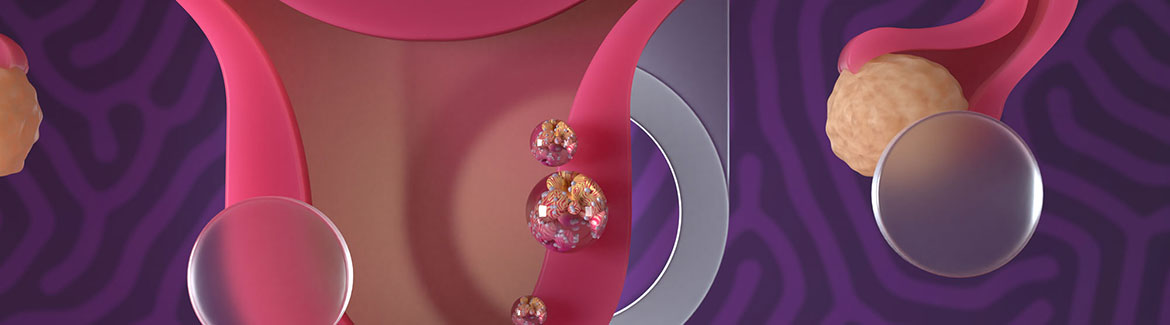
Uterine cancer is the most prevalent gynaecological cancer in New Zealand, with an average of 627 females newly diagnosed each year (from 2015 – 2020). Endometrial cancer accounts for the majority of uterine cancer diagnoses. Excessive exposure to endogenous or exogenous oestrogen unopposed by progesterone is aetiologically linked to most endometrial cancers. Obesity is one of the most significant risk factors, with an estimated six out of ten diagnoses of endometrial cancer attributed to this.
Read the full article here.
 A B-QuiCK summary is
also available here.
A B-QuiCK summary is
also available here.
Potential pertussis outbreak
Te Whatu Ora, Health New Zealand, is asking healthcare professionals to be alert for patients with any symptoms suspicious of pertussis (whooping cough) following concerns of potential community spread. Vaccination (with diphtheria, tetanus and pertussis vaccine, Boostrix) should be strongly encouraged for young children, their caregivers and people who are pregnant. Boostrix is now able to be offered in community pharmacies for eligible people at no cost.
Infants and young children are eligible to received funded Boostrix at ages six weeks, three months and five months. Boosters are available at ages four and eleven years. For people who are pregnant, Boostrix can be administered as a single dose from the second trimester of each pregnancy (funded; recommended from 16 weeks, but at least two weeks before birth). It is also recommended that close family contacts of infants/young children, e.g. parents, grandparents, have a booster dose* to reduce potential spread. A full list of eligibility criteria for funded vaccination can be found here.
*Only funded for parents or primary caregivers of infants admitted to a NICU or Specialist Care Baby Unit for more than three days, who had not been exposed to maternal vaccination at least 14 days prior to birth
This is a timely reminder to opportunistically check whether patients, particularly children, have completed their course of Boostrix and to offer vaccination where appropriate. Some children may have missed out on their scheduled Boostrix vaccine(s) during the last three years due to the COVID-19 pandemic and lockdowns.
COVID-19 antivirals molnupiravir (Lagevrio) and tixagevimab + cilgavimab (Evusheld) no longer recommended by advisory group
Te Whatu Ora, Health New Zealand, has released two position statements from the COVID-19 Therapeutics Technical Advisory Group:
Molnupiravir no longer recommended for treatment of COVID-19
Molnupiravir (Lagevrio) is indicated for the treatment of mild-to-moderate COVID-19 for people at higher risk of severe disease. Nirmatrelvir with ritonavir (Paxlovid) has always been the first-line antiviral for the treatment of COVID-19, with molnupiravir the recommended alternative for patients who are unable to take nirmatrelvir with ritonavir (Paxlovid).
At the beginning of the pandemic, before the emergence of Omicron and other variants, molnupiravir was an effective treatment for COVID-19, reducing both the number of hospitalisations and deaths. But more recent evidence* has not shown clinical benefit in highly vaccinated populations or against Omicron variants. The COVID-19 Therapeutics Technical Advisory Group therefore no longer recommends molnupiravir for the treatment of COVID-19. Nirmatrelvir with ritonavir (Paxlovid) remains the first-line treatment for patients with COVID-19, with remdesivir (Section 29) recommended as the second-line option.
*Based on the PANORAMIC trial, however, it should be noted that there are concerns that the trial population did not consider older people in high-risk groups (who may be unable to take Paxlovid) who may still benefit from molnupiravir: https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(22)02593-4/fulltext
Evusheld no longer recommended for pre-exposure prophylaxis or treatment of COVID-19
Tixagevimab with cilgavimab (Evusheld) has primarily been indicated for the pre-exposure prophylaxis of COVID-19 in people with severe immunocompromise at high risk of COVID-19. However, as new variants of SARS-CoV-2 have emerged, clinical utility of Evusheld has decreased. It is currently predicted to neutralise against < 10% of current circulating SARS-CoV-2 variants in New Zealand. Therefore, the COVID-19 Therapeutics Technical Advisory Group no longer recommend Evusheld for the pre-exposure prophylaxis of SARS-CoV-2 infection.
Potential risk of neurotoxicity with cephalosporins
Several reports have been made to the Centre for Adverse Reactions Monitoring (CARM) of potential neurotoxicity associated with cephalosporins, e.g. cefaclor, cefalexin, ceftriaxone. Neurotoxic adverse effects include seizures, myoclonus, compulsion, confusion, encephalopathy, agitation, hallucination and delirium.
In December, 2022, The Medicines Adverse Reactions Committee (MARC) consulted on this potential risk, and determined that although available data are limited, an association between neurotoxicity and the cephalosporin class of antibiotics could not be discounted. The full report can be read here. This safety issue has been highlighted in the latest edition of Prescriber Update.
Read more
Neurotoxicity (in particular, encephalopathy, myoclonus and/or seizure) has been reported with all five generations of cephalosporins, however, international case reports and case series reviews have found that cefepime (a fourth generation cephalosporin) has been associated with the most reports. Cefepime is not funded for community use in New Zealand; it is available in injectable form only. In New Zealand, the cephalosporin with the most reports to CARM of potential neurotoxicity is cefazolin (IV), followed by cefuroxime and then cefaclor.
The risk of neurotoxicity with cephalosporins appears to be associated with impaired renal function (when doses are not adjusted appropriately), older age, pre-existing central nervous system disorders and high doses of cephalosporins administered by intravenous injection. Patients who are acutely unwell and taking cephalosporins may also be at higher risk of neurotoxicity due to increased blood-brain barrier permeability (and therefore increased penetration of cephalosporins into the central nervous system).
The cephalosporin data sheets will be updated to include reports of neurotoxicity associated with cephalosporins, risk factors and management recommendations.
Identifying neurotoxicity in patents taking cephalosporins can be challenging; consider cephalosporin-induced neurotoxicity in a patient with risk factors and unexplained, new-onset neurological symptoms or signs. If neurotoxicity occurs, the cephalosporin should be withdrawn.
Avoid use of metoclopramide in children and young adults if possible
As reported in the latest issue of Prescriber Update, Medsafe is reminding clinicians that use of metoclopramide in children and young adults (aged 1 – 19 years) is limited to second-line treatment of certain conditions only (see below) due to the risk of dystonia. This comes following several reports to the Centre for Adverse Reactions Monitoring (CARM) of dystonic reactions in children taking metoclopramide.
Read more
Metoclopramide is available in New Zealand in tablet*, oral liquid (Section 29; not funded) and solution for injection forms. For children aged 1 – 19 years (inclusive), metoclopramide is only indicated for use as a second-line treatment for severe intractable vomiting of a known cause, vomiting associated with chemo-or radiotherapy and prior to some surgical procedures or intubation; it is not recommended to be used in people aged < 20 years unless absolutely necessary. See NZFC for further information.
*Tablets unapproved for use in children aged under 15 years
Dystonia, a movement disorder that causes repetitive or twisting body movements due to involuntary muscle contractions, can occur after a single dose of metoclopramide and is more common in children and young adults, in females and with higher doses. To reduce the risk of dystonia, the dosing recommendations must be strictly adhered to.
Trikafta to be funded from 1 April
Pharmac has announced that Trikafta (elexacaftor with tezacaftor and ivacaftor) will be funded from 1 April, 2023, for people aged ≥ 6 years with cystic fibrosis who meet Special Authority eligibility criteria.
Special Authority can be applied for by any relevant practitioner, but funded treatment will only be dispensed from a Te Whatu Ora inpatient hospital pharmacy (of the patient’s choice). Community pharmacies (including both retail and outpatient pharmacies within Te Whatu Ora hospitals) will not be able to dispense Trikafta due to the high cost of the medicine.
N.B. Some patients may have cystic fibrosis caused by rare mutations that are not covered by this access criteria. Prescribers can apply for a Named Patient Pharmaceutical Assessment (NPPA) for these patients. Pharmac will require evidence that Trikafta works for the specific mutation(s) for treatment to be funded. Further information on NPPA applications is available here.
In Brief: monthly fluoxetine dispensing resumed
The seven day dispensing limit for fluoxetine 20 mg capsules has now been removed; monthly dispensing has therefore resumed. As reported in Bulletin 67, the dispensing limit was put in place as the brand change for fluoxetine from Fluox to Arrow-Fluoxetine occurred earlier than expected, causing a supply issue with Arrow-Fluoxetine.
Paper of the Week: "Is there any chance you could be pregnant?"
Most maternity care is carried out by midwives and obstetricians in New Zealand, but general practitioners still have a role in the general medical care of people who are pregnant, including prescribing routine and acute medicines. The problem is that prescribers may not always be aware that the patient is pregnant when they are treating them.
A study published in the British Journal of General Practice has highlighted a breakdown in communication that can have significant long-term consequences for pregnant patients and their child. The aim of this study was to assess general practitioner awareness of pregnancy and its association with prescribing medicines with potential safety risks. It was found that only 48% of patients who were pregnant had confirmation of pregnancy coded in their patient record and subsequently, these patients were 59% more likely to be prescribed a teratogenic medicine that should have been avoided during pregnancy (odds ratio 1.59; confidence interval 1.49 to 1.70).
This study serves as a reminder that, if appropriate, clinicians should always check a patient’s pregnancy status, especially when prescribing higher risk teratogenic medicines, e.g. isotretinoin, antiepileptics and angiotensin-converting enzyme inhibitors.
Read more
- Researchers from the Netherlands used the PHARMO Perinatal Research Network (PPRN) to access the medical and pharmacy records of 96,182 patients and 140,976 pregnancies between 2004 and 2020
- Researchers looked at patient characteristics including medicines use for chronic conditions before pregnancy and healthcare utilisation during pregnancy, e.g. number of visits to the general practitioner, prescriptions dispensed and specialist letters
- General practitioner awareness of pregnancy was defined as either a:
- Pregnancy confirmation (specific code for pregnancy in the patient’s medical record); or
- Pregnancy indicator (any mention of pregnancy in the patient’s medical record, e.g. uncoded text note); or
- Pregnancy contraindication that was actively linked to the patient’s medical record
- The prescribing of hazardous medicines was determined by prescriptions from a general practitioner initiated or continued during the pregnancy period
- A hazardous medicine was defined as having pharmacological or teratogenic effects that should be monitored or (temporarily) avoided
- A highly hazardous medicine was defined as having teratogenic effects that should be (temporarily) avoided
- Medicines that were prescribed for pregnancy-related indications were removed, e.g. progesterone to reduce risk of preterm birth
- Overall, fewer than half of patients (67,496; 48%) who were pregnant during the study period had a confirmation of pregnancy code in their medical records
- The data suggest that general practitioner awareness of pregnancy is increasing over time as use of the pregnancy confirmation code increased from 28% in 2004 to 63% in 2020
- However, 23% of patients who were pregnant in 2020 did not have any mention of their pregnancy in their general practitioner medical records
- Of the patients who had a pregnancy confirmation in their record, most (52,640; 78%) were recorded during the first trimester
- Hazardous medicines were prescribed to 22% (31,523) of patients who were pregnant during the study. Only 29% of these patients (9,265 of 31,523) had a pregnancy confirmation in their medical record at the time the hazardous medicine(s) was prescribed (45% for any pregnancy indicator [14,212 of 31,523]).
- Patients who were pregnant but did not have a pregnancy confirmation in their medical records were 59% more likely to be prescribed a highly hazardous medicine (odds ratio 1.59; confidence interval 1.49 to 1.70) compared to those with a recorded confirmation of pregnancy
- Of the 3% of patients (4,489) who were pregnant and received highly hazardous medicines, a pregnancy confirmation was recorded in 13% (5,585 of 4,489), and any pregnancy indicator was recorded in 26% (1,171 of 4,489) of patient records
- Isotretinoin and methotrexate were 30 times and ten times more likely to be prescribed for a patient who was pregnant if there was no pregnancy confirmation in their medical records compared to if a general practitioner was aware of the pregnancy
- Doxycycline, misoprostol and norethisterone were the most commonly prescribed highly hazardous medicines to patients who were pregnant during this study
- The authors of the study acknowledged that use of dispensing records is only an estimate of hazardous medicine exposure as there was no way to measure the patient’s adherence and the use of hazardous medicines may be overestimated. Underestimated medicine exposure may also be likely as over-the-counter and specialist-prescribed medicines were not included in this study.
- Three implications of this study were suggested:
- The importance of maintaining clear, accurate and up to date medical records
- Electronic medical record systems need to be simple to use and standardised across the entire healthcare system
- Increased public awareness of hazardous medicines in pregnancy and ensuring pregnant patients are fully informed of the risks when taking medicines during pregnancy
Houben E, Swart KM, Steegers EA, et al. GPs’ awareness of pregnancy: trends and association with hazardous medication use. Br J Gen Pract 2023;BJGP.2022.0193. doi:10.3399/BJGP.2022.0193
For further information on considerations regarding medicine safety in pregnancy, see the New Zealand Formulary pregnancy information: https://www.nzf.org.nz/nzf_70762
Patient information leaflets from the United Kingdom Teratology Information Service are available at: https://www.medicinesinpregnancy.org/
 This Bulletin is supported by the South Link Education Trust
This Bulletin is supported by the South Link Education Trust
If you have any information you would like us to add to our next bulletin, please email:
editor@bpac.org.nz
© This resource is the subject of copyright which is owned by bpacnz. You may access it, but you may not reproduce it or any part of it except in the limited situations described in the terms of use on our website.
