 Want to receive Best Practice Bulletin directly to your inbox?
Sign up here.
Want to receive Best Practice Bulletin directly to your inbox?
Sign up here.
Published: 6th September, 2024
Contents
New from bpacnz
Peer group discussion: Managing winter ills in primary care
The winter flu season is a particularly busy time of year in primary care. Increasing circulation of respiratory syncytial virus (RSV), influenza type A, common colds and COVID-19 in the community inevitably results in high numbers of patients presenting with “cold and flu” symptoms. Appropriate management is clear in most cases, e.g. manage symptomatically, recovery at home or urgent hospital referral for very unwell patients. However, the challenge in primary care is identifying patients whose symptoms and signs, or other clinical characteristics, put them at greater risk of deterioration and adverse outcomes, e.g. pneumonia. These patients often require close monitoring, safety netting and a low threshold for hospital referral.
Click here to view the peer group discussion; this can be used for clinical peer groups, student study groups or personal reflection.
Clinical audit: Monitoring renal function in patients with diabetes

Diabetic kidney disease is the leading cause of end-stage renal disease in New Zealand. Māori and Pacific peoples with diabetic kidney disease often have more severe disease and poorer outcomes than other patient groups. Patients with diabetes should have their renal function tested at least once per year as part of their annual diabetes review. This audit assesses the frequency and extent of renal monitoring for patients with type 1 and type 2 diabetes in your practice. As an optional extra, patient ethnicity can be analysed to determine if there are disparities in renal monitoring.
Click here to view the audit
Isotretinoin consent form
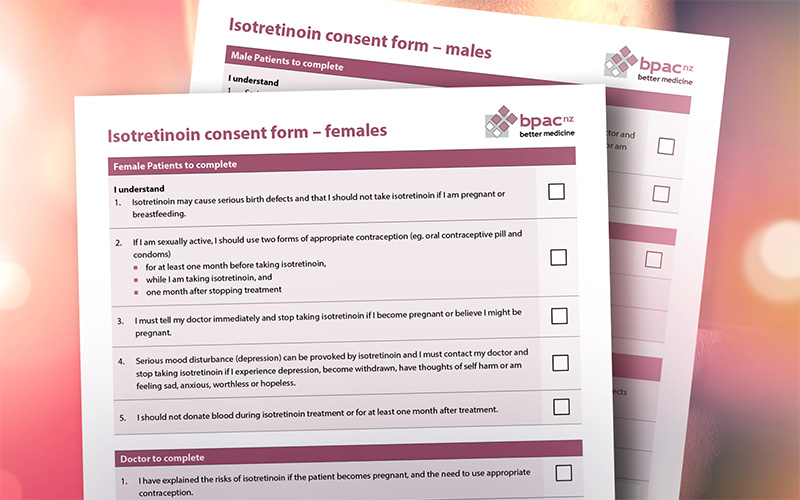
The BPAC Clinical Solutions decision support module on acne management is no longer available (as reported in Bulletin 104). An editable version of the isotretinoin consent form that was included in the module is now located with the bpacnz resource on acne and is available to download, save and print.
Click here to view the consent form
Continuous glucose monitors to be funded for type 1 diabetes
Continuous glucose monitors (CGMs) will be funded from 1st October, 2024, for people with type 1 diabetes and other specific forms of diabetes e.g. type 3c, if they meet criteria for Special Authority approval. Pharmac is also widening access to insulin pumps and consumables for these patient groups. Five new funded CGMs will be available. These are either standalone devices or interoperable devices that are used in conjunction with one of the two funded brands of insulin pumps. Initial Special Authority applications (valid for one year) and ongoing renewals (valid for two years) for CGMs and insulin pumps can be made by any relevant practitioner, however, patients prescribed an interoperable CGM as part of an automated insulin delivery system still require evaluation by a diabetes multidisciplinary team to establish whether an insulin pump is appropriate before starting treatment.
The MiniMed 770G insulin pump that is currently funded for people who meet Special Authority criteria will be delisted from the Pharmaceutical Schedule on 1st January, 2025. The consumables associated with this pump will be delisted on 1st October, 2026. The staggered delisting is intended to allow time for people to switch to one of the funded brands of insulin pumps. People who cannot switch to one of the new funded brands of insulin pumps for clinical or other reasons can apply for continued funding via the Exceptional Circumstances pathway.
Pharmac acknowledges that pharmacists will need to provide comprehensive information when dispensing CGMs to a patient for the first time; a brand switch fee is available from 1st October, 2024, to 1st January, 2025.
For further information from Pharmac about funding of CGMs and insulin pumps, click here. Training and educational resources for healthcare professionals are currently being developed.
Medicine supply news: Methylphenidate, capsaicin cream
The following issues relating to medicine supply, of particular interest to primary care, have recently been announced. These items are selected based on their relevance to primary care and where issues for patients are anticipated, e.g. there is no alternative medicine available or changing to the alternative presents issues. Information about medicine supply is available in the New Zealand Formulary at the top of the individual monograph for any affected medicine and summarised here.
Methylphenidate supply status
Pharmac has provided updated information regarding ongoing supply issues affecting both Concerta and Teva brands of extended-release methylphenidate. The stock situation for methylphenidate is frequently changing (information on availability now differs from what was reported in Bulletin 106); check the Pharmac website and the methylphenidate monograph on NZF for up-to-date information or contact your local pharmacy prior to issuing a prescription for a patient. Patients (or their parent/caregiver) can also be recommended to contact their usual pharmacy to see which formulations are available
A reminder that Pharmac is advising prescribers to not start new patients on extended-release methylphenidate where possible. Information on the legal requirements when prescribing methylphenidate is available here. Brands are not interchangeable unless the patient has Special Authority approval for both Teva and Concerta.
Capsaicin cream recall
There is a product recall of 0.075% Rugby Capsaicin Topical Cream (Section 29), which has been listed as an alternative brand of capsaicin cream since 2022, due to ongoing supply issues. The manufacturer is recalling one batch of 0.075% Rugby Capsaicin Topical Cream due to potential problems with the product appearance: batch number: 24-01307, expiry: 01/2026. Ask patients who you have prescribed capsaicin to, to check at home to see if they have received the affected product. Pharmacies should assess stock for the affected batch and ask patients picking up a new prescription to check whether they have the product at home. It is not anticipated that this recall will result in supply issues, as the new brand Zo-Rub*, 0.075% Capsaicin Topical Cream is now available. The 0.025% Capsaicin Topical Cream is unaffected.
* Zo-Rub is replacing the Zostrix brand of capsaicin cream, as reported in Bulletin 105.
Mpox update from the National Public Health Service
The National Public Health Service has published an update on mpox. This update comes after the World Health Organization declared mpox as a Public Health Emergency of International Concern (PHEIC) in August; see Bulletin 106 for details.
There are two subtypes (clades) of mpox virus: clade I (Ia and Ib) and clade II. Clade II mpox virus has been the cause of the ongoing mpox outbreak and predominantly affects men who have sex with men. Clade I is more likely to cause severe infection and can be transmitted via both sexual and non-sexual contact; there is greater public health risk associated with this subtype. An outbreak of mpox clade Ib in parts of Africa enacted the PHEIC. ESR has assessed the overall public health risk of clade I mpox in New Zealand as low, and low-moderate for clade II mpox.
The Ministry of Health, Manatū Hauora, and Health New Zealand, Te Whatu Ora, are considering how to implement recommendations for mpox made by the World Health Organization. Guidance in New Zealand is currently based on the clade II mpox virus. Updates to clinical guidance and public health advice will be made as required; at this stage, strengthened testing and referral pathways are being planned.
The situation with clade I mpox and implications for New Zealand is being monitored closely; the National Public Health Service states that New Zealand is prepared in the case of an outbreak of mpox.
Further information on mpox is available from Health New Zealand, Te Whatu Ora (currently under review).
NZF special report: Nitrofurantoin safety reminders
In a new feature for Best Practice Bulletin, the team at NZF highlights a prescribing-related practice point.
Nitrofurantoin is commonly used for the treatment of urinary tract infection (UTI) and may also be used in some cases for prophylaxis of recurrent UTI. Duration of treatment for prophylactic doses may be up to six months, and in some instances longer if treatment is reviewed and the benefits outweigh the risk.
Always check you are prescribing and dispensing the correct product and dose: immediate-release and modified-release preparations are available and funded.
- Standard dosing of modified-release capsules is twice daily for a UTI, while the immediate-release tablets are typically prescribed four times daily
- Prescribers should ensure the correct brand is noted on the prescription so that it is clear whether they intend to prescribe the modified-release (Macrobid) or immediate-release (Nifuran) preparation, and pharmacists should query any non-standard dosing to ensure it is intentional
Serious pulmonary reactions such as pulmonary fibrosis (may be irreversible) and interstitial pneumonitis can occur with short-term or long-term use:
- Be alert for symptoms and signs of pulmonary toxicity in patients taking nitrofurantoin
- Ensure patients are aware of what to watch for including new or worsening symptoms of cough or shortness of breath, and that they must report these
- Monitor lung function in patients taking nitrofurantoin long term
- Stop treatment at the first sign of pulmonary toxicity
For further information, refer to the Nitrofurantoin monograph in the NZF. N.B. These prescribing-related practice points are also published in the NZF monthly release email.
A 2020 Prescriber Update article on nitrofurantoin safety is available here
A recent Health and Disability Commission decision concerning a patient death from pulmonary fibrosis highlights the risks of long-term nitrofurantoin treatment. Click here to read the full decision.
NZF updates for September
Significant changes to the NZF in the September, 2024, release include:
- Guidance for switching patients to alternative insulin products from the NZ Society for the Study of Diabetes (NZSSD) has been added to the biphasic isophane insulin monograph in preparation for the discontinuation of Penmix 30, Mixtard 30, and Penmix 50 (also reported in Bulletin 105)
- The recommended duration for first-line triple treatment regimen for Helicobacter pylori infection has increased to 14 days. For further information on the testing and treatment of H. pylori, see: bpac.org.nz/2022/h-pylori.aspx.
- Updates to the therapeutic notes for beta-adrenergic blocking drugs to include information about the use of beta blockers for portal hypertension (unapproved indication). The therapeutic notes for urinary incontinence in women have also been updated with information on antimuscarinic adverse effects and anticholinergic burden in older people.
- Dosing regimens have been updated for metoprolol succinate (arrhythmias) and nadolol and propranolol (prophylaxis of variceal bleeding in portal hypertension [unapproved indication])
- New monograph added for lanreotide, indicated for the management of acromegaly and neuroendocrine tumours
- A range of new patient information leaflets added
You can read about all the changes in the September release here. Also read about significant changes to the NZF for Children (NZFC), here.
Latest edition of Prescriber Update released
The September edition of Prescriber Update has been published. Particular items of interest for primary care include:
Reminder: ACE inhibitors and ARBs are contraindicated during pregnancy
Medsafe is reminding clinicians that use of ACE inhibitors and ARBs is contraindicated during pregnancy as there is an increased risk of fetal and neonatal abnormalities. Therefore, any females planning or considering pregnancy should ideally use an alternative medicine, or switch from an ACE inhibitor/ARB to another option, e.g. labetalol, nifedipine, methyldopa, once the pregnancy is confirmed.
For further information on the management of hypertension, see: bpac.org.nz/2023/hypertension.aspx
Medicine-induced tendinopathy
Many medicines are associated with tendinopathy, particularly fluoroquinolones (usually within 48 hours), corticosteroids (usually ≥ 3 months), statins (usually 8 – 10 months) and aromatase inhibitors used in cancer treatment (usually within two weeks to 19 months). The Achilles tendon is most commonly affected. Risk factors for medicine-induced tendinopathy include advanced age, obesity and physical exertion and certain co-morbid conditions, e.g. connective tissue disorders, renal failure. Discontinue treatment if tendonitis is suspected, e.g. pain, swelling, inflammation, and prescribe an alternative medicine if possible. Between January, 2014, and June, 2024, there were 103 cases of tendon disorders associated with medicine use reported to Medsafe and CARM; ciprofloxacin, norfloxacin, zoledronic acid and prednisone were the most commonly associated medicines. Read the full article here.
Medicines and food interactions
Specific foods interact with certain medicines and alter the pharmacokinetic and pharmacodynamic properties. For example, vitamin K rich foods such as broccoli can interact with warfarin, fruits such as grapefruit can interact with statins and calcium channel blockers. Potential food-medicine interactions should be considered when first prescribing a medicine to a patient, and during subsequent medicine reviews. The NZF interactions checker (click on Interactions Tab and enter medicines/substances in the search bar) can be used to check the interaction between medicines and some foods, e.g. grapefruit, garlic, cranberry, fish oil. Read the full article here.
Medicines that may cause or exacerbate myasthenia gravis
Myasthenia gravis can be caused or exacerbated by certain medicines including immune checkpoint inhibitors, aminoglycosides, antimuscarinics, benzodiazepines and statins (recently identified adverse effect; Medsafe has requested the data sheets of all statins be updated to include this association). CARM has received three reports of myasthenia gravis where pembrolizumab was the suspect medicine, and two for atorvastatin (as of 30th June, 2024).
Patients taking medicines associated with myasthenia gravis should be advised to be aware of new or worsening symptoms, including drooping eyelids, double vision, chewing or swallowing difficulties, speech disturbance, limb weakness and shortness of breath, and to seek medical care if these occur. Consider stopping the medicine if appropriate. Read the full article here.
Medicines Monitoring reminders: be alert to new-onset eczema in patients taking calcium channel blockers, and potential mood changes in patients taking direct acting oral anticoagulants; report any suspected cases to CARM. See Bulletin 97 and Bulletin 105, respectively, for further information.
View the full edition of Prescriber Update here
Health and Independence Report 2023 | Ministry of Health
The Health and Independence Report 2023 presents an overview of the current state of public health in Aotearoa New Zealand, using health-related data from a range of sources for the 2023 calendar year. Life expectancy, morbidity and mortality, the impacts of COVID-19 and a range of other health measures, e.g. immunisations, long-term conditions, primary care, are reported.
The report shows that people of Māori and Pacific ethnicity, and people with a disability continue to experience inequity and poorer health outcomes compared to the general population. Time taken to get an appointment remains the most common reason for not attending primary care, followed by cost. Read the full report here.
Further information, including data tables, is available here. There is also an associated press release detailing some of the key findings.
Gynaecological Cancer Awareness Month
September is Gynaecological Cancer Awareness Month. The focus this year is on ovarian cancer, which is the second most common gynaecological cancer after endometrial cancer. Ovarian cancer has a higher mortality rate that other gynaecological cancers, however, there is currently no reliable screening test. Diagnosis relies on the prompt recognition and investigation of symptoms (see below). Clinicians should have a low threshold for initiating further investigations in patients with suspicious symptoms if they are post-menopausal and/or if the symptoms are new, severe, unusual, recurrent or persistent, e.g. occurring 12 or more days per month.
Key symptoms and signs that may suggest a diagnosis of ovarian cancer include:
- Abdominal bloating or distension
- Abdominal or pelvic pain
- Early satiety or loss of appetite
- Increased urinary frequency or urgency
- Changes in bowel habit*
- Fatigue
- Unexplained weight loss
- Post-menopausal bleeding
* New symptoms suggestive of irritable bowel syndrome in females aged > 50 years are unusual; consider the possibility of ovarian (or bowel) cancer in these patients
bpacnz has published a series of gynaecological cancer articles with support from Te Aho o Te Kahu, Cancer Control Agency. This collection covers the early detection and diagnosis of ovarian cancer, as well as cervical, endometrial, vulval and vaginal cancers, managing follow-up and ongoing surveillance in primary care. Click here to browse these resources.
Blue September: Prostate cancer awareness
This month marks the annual Blue September prostate cancer awareness month and fundraiser. Prostate cancer remains the third highest cause of cancer mortality in males in New Zealand. This year, the Prostate Cancer Foundation NZ is encouraging people to “do something blue to help a mate through.” This is also an opportunity for clinicians to ask males aged over 50 years (or 40 years in those with a family history of prostate cancer) about any lower urinary tract symptoms or concerns, as this can identify patients in whom further investigation is warranted, e.g. prostate specific antigen (PSA) testing, digital rectal examination (DRE).
Blue September resources are available here.
For further information on testing for prostate cancer in primary care, see: bpac.org.nz/2020/prostate.aspx and bpac.org.nz/report/2020/psa.aspx
Upcoming Goodfellow Unit webinars
The Goodfellow Unit, University of Auckland, is hosting several free access webinars in the coming months. These webinars are intended to provide topical and relevant health information for primary care clinicians. Continuing professional development (CPD) points are also available. Webinars are often recorded and available to watch at a later date. Upcoming webinars include:
In brief: New IMAC factsheets
IMAC publishes factsheets on a range of topics relating to vaccination. New factsheets are added, and existing ones are updated over time. Recent factsheets that may be of particular interest to primary care include:
Paper of the Week: TCAs for IBS?
People with irritable bowel syndrome (IBS) can experience a substantial reduction in quality of life, both through physical symptoms and negative social effects. IBS is a diagnosis of exclusion and may take some time to be diagnosed. Some patients may feel their symptoms are minimised, especially given that an underlying cause is rarely found, and first-line treatments involve education and lifestyle modification (e.g. low FODMAP diet, change in dietary fibre). Many patients will also trial over-the-counter products, e.g. probiotics, bowel health supplements, peppermint oil.
Medicines are typically reserved for the management of specific symptoms when first-line options have not been effective, e.g. loperamide, mebeverine, lactulose. Tricyclic antidepressants (TCAs) can also be considered off-label for IBS symptoms. Typical dosing is to initiate patients on 5 – 10 mg of amitriptyline or nortriptyline, once daily, and up-titrate to a maximum of 30 mg in fortnightly intervals. TCAs have been shown to reduce abdominal pain and improve other IBS symptoms, e.g. diarrhoea, however, patients may be reluctant to try a medicine traditionally used for depression. Some clinicians may also be hesitant or reluctant to prescribe a TCA for a patient with IBS.
A study published in the British Journal of General Practice investigated patient and clinician opinions concerning the use of amitriptyline for IBS symptoms. A sample of participants and general practitioners already involved in a study comparing low-dose amitriptyline with placebo for IBS were interviewed. Several themes were identified including concerns about the conventional use of amitriptyline as an antidepressant (and the associated stigma), the considerations regarding long-term use of amitriptyline such as impact on future medicines decisions and polypharmacy, and the demand for new IBS treatment approaches. The authors concluded that the potential benefits of trialling low-dose amitriptyline in patients with IBS outweigh the risks, in most cases, but clear communication regarding those benefits and risks is required to address any patient concerns.
How do you approach patients diagnosed with IBS who cannot successfully manage their symptoms with lifestyle modifications? Would you consider prescribing low-dose TCAs for patients with IBS? If you have prescribed a TCA for a patient with IBS, has it been effective? Was the patient accepting of treatment with a TCA?
Read more
- A nested qualitative interview study was conducted within the Amitriptyline at Low-dose and Titrated for Irritable Bowel Syndrome as Second-line Treatment (ATLANTIS) trial, a randomised, double-blind, placebo-controlled trial carried out in 55 General Practices located in West Yorkshire, Wessex and West England
- Participants in the ATLANTIS trial were randomised to receive either low-dose amitriptyline (10 mg, once daily at night, titrating up to 30 mg, once daily) or a placebo for six months, with the option of a further six months treatment
- Expressions of interest were also sought to take part in the qualitative study
- After six months, 23 participants from the treatment group and 19 controls were interviewed (n = 42, 71% female). At 12 months, follow-up interviews were conducted with 19 participants (nine from the treatment group). Interviews were also conducted with 16 general practitioners involved in the ATLANTIS trial at this time point.
- Notably, the sample population was not representative of the general population; the ethnicity of 98% of participants and 75% of general practitioners was listed as “white”
- Difficulties contacting participants and delays relating to COVID-19 were cited as reasons for the low number of follow-up interviews
- All participants (and general practitioners) who expressed interest in the qualitative study and replied to the authors were included
Three main themes were identified from both participant and general practitioner responses:
Concern about amitriptyline being indicated for depression
- The use of amitriptyline as an antidepressant and the stigma associated with depression were viewed as potential barriers to treatment. Consider explaining to patients that “yes, the medicine is technically an antidepressant, but it is commonly used to treat pain and other conditions”, and give an example of another medicine that is used for other indications, e.g. “bupropion (Zyban) is used by many people for smoking cessation, but it is actually an antidepressant”.
- Psychological adverse effects of TCAs were a primary concern for participants
- General practitioners perceived that patients can be reluctant to take antidepressants for depressive symptoms and may be even more reluctant to trial an antidepressant for a “functional health problem”
- Clear explanation of the difference in dosage of amitriptyline between the treatment of IBS and depression and that the risk of adverse effects is reduced with lower doses may increase patient acceptance
- Self-titration of amitriptyline dosing may be appropriate for some patients, giving them more control over their IBS management. Amitriptyline self-titration guidance for patients used in the ATLANTIS trial is available here.
Concern regarding the need for a long-term medicine for IBS management
- There was hesitancy to “medicalise” IBS, especially if lifestyle modifications can effectively manage symptoms for some people
- Clinicians felt prescribing amitriptyline long-term has implications for future medicines decisions, contraindications, polypharmacy (i.e. anticholinergic burden) and increased resource requirements, e.g. repeat prescriptions, more regular patient follow-up
- A well-established body of literature for amitriptyline gave clinicians and participants more confidence when prescribing or taking amitriptyline, as opposed to trialling a novel or unproven medicine
N.B. Patient tolerance can limit use; nortriptyline is likely to have a similar effect on IBS symptoms as amitriptyline and is often better tolerated.
A new approach to managing IBS
- Given the challenging nature of managing IBS that often involves trialling multiple treatments, tricyclic antidepressants, e.g. amitriptyline, nortriptyline, can be viewed as a useful tool for clinicians to offer patients and as a source of hope for those with persistent symptoms
Teasdale E, Everitt H, Alderson S, et al. Low-dose amitriptyline for irritable bowel syndrome (IBS): a qualitative study of patients’ and GPs’ views and experiences. Br J Gen Pract 2024;:BJGP.2024.0303.
For further discussion on the use of TCAs in IBS, see: bpac.org.nz/BPJ/2014/February/ibs.aspx
 This Bulletin is supported by the South Link Education Trust
This Bulletin is supported by the South Link Education Trust
If you have any information you would like us to add to our next bulletin, please email:
editor@bpac.org.nz
© This resource is the subject of copyright which is owned by bpacnz. You may access it, but you may not reproduce it or any part of it except in the limited situations described in the terms of use on our website.





