Published: July, 2025 | Review date: July, 2028
This audit identifies patients who were issued a “Fully unfit” or “Fit for selected work” medical certificate in the past 12 months to assess whether the designation, and the overall proportion of “Fully unfit” medical certificates issued, was appropriate.
“Prescribing” time off work can be considered as a treatment like prescribing a medicine for pain management after an injury. Short-term absences from work immediately post-injury can be important for recovery, however, as with any treatment, potential associated harms must be considered before initiation, e.g. prolonged recovery, reduced social interaction, increased risk of long-term unemployment. Inappropriately designating a patient as “Fully unfit” rather than “Fit for selected work” could be viewed in the same light as prescribing an opioid analgesic when paracetamol or a NSAID is sufficient or prescribing a long course of pain relief when discomfort is expected to resolve within a short timeframe.
Regularly reviewing whether the benefits of continuing to prescribe time off work outweigh the potential risks is also necessary, much as it is when prescribing a medicine with potential for misuse.
ACC definitions for medical certification have evolved over time with “Fully unfit” undergoing the most significant change. The three categories of medical certification when lodging ACC45 and ACC18 forms are:
- Fully fit – able to functionally perform full pre-injury work duties and hours
- Fit for selected work – able to engage in physical rehabilitation and some level of work with support, e.g. amended duties, workplace adaptations, altered hours or a phased return to work
- Fully unfit – essentially hospitalised or “house-bound”, and should meet one of the following limited criteria:
- Total inability to work – the patient is either admitted to hospital or unable to effectively mobilise from their bed
- Contagion risk or quarantine need – the patient is at risk of infection due to their injury and the environment they usually work in and is unable to work remotely
- Health and safety risk – the patient being in the workplace, even with assistance or modifications, poses a specific health and safety hazard to themselves, their co-workers or the general public, e.g. due to the impact of the injury or the medicines being taken. This criterion does not apply when the patient is functionally able to perform alternative tasks, even if these do not align with their usual role in the workplace.
Selecting the appropriate medical certificate designation is critical as a prompt return to, and recovery at, work can improve physical rehabilitation, mental health and help to maintain social/vocational connections. As such, “Fit for selected work” should generally be the first consideration for most injured patients who are not “Fully fit” for work. If time fully off work is required to support initial recovery, a pragmatic approach is required, e.g. sign the patient off work for a short time only post-injury before re-assessing if they can transition to “Fit for selected work” or “Fully fit”.
For further information on navigating the ACC Recovery at Work process, including considerations when conducting an initial medical certification consultation, medical certificate definitions, as well as the ACC-mediated supports available if further assistance is required, see: https://bpac.org.nz/2024/recovery-work.aspx
Summary
This audit focuses on the appropriate designation of “Fully unfit” or “Fit for selected work” when issuing a medical certificate to a patient following injury.
Recommended audit standards
Ideally, only patients who meet ACC’s limited criteria are issued an ACC18 “Fully unfit” medical certificate, while most patients who are not “Fully fit” for work should be issued an ACC18 “Fit for selected work” medical certificate. Therefore, the overall proportion of“Fully unfit” medical certificates should be low. This may not be achieved on the first cycle of the audit but should be the aim for the second cycle. ACC45 medical certificates are excluded from this audit because a short period away from work following a significant injury is more likely to be appropriate (ACC45 certificates are, however, included in the “Working audit” option – see below).
It is acknowledged that previously, you may have decided that a “Fully unfit” medical certificate was the most appropriate course of action even though ACC criteria were not met (or you were not fully aware of the criteria). This audit includes the option of recording justification for your decision on the data sheet, providing an opportunity to reflect on whether you would make the same decision now after having read the Recovery at Work education resources.
Other optional data recording include:
- Injury type - consider whether this influences decision-making about medical certification
- Length of time the certificate is issued for - reflect on whether this was reasonable and whether it is also influenced by injury type
 Alternatively, consider a “working audit” where data are collected over time when an eligible patient presents following an accident resulting in injury. If the patient is not “Fully fit” for work, issue a medical certificate that is designated “Fully unfit” or “Fit for selected work”, based on the ACC criteria. Both ACC45 or ACC18 medical certificates can be included in this audit option as the patient may be presenting for the first time or a subsequent visit, e.g. doctors working in urgent care are more likely to see patients at first presentation and issue ACC45 medical certificates rather than ACC18 certificates.
Alternatively, consider a “working audit” where data are collected over time when an eligible patient presents following an accident resulting in injury. If the patient is not “Fully fit” for work, issue a medical certificate that is designated “Fully unfit” or “Fit for selected work”, based on the ACC criteria. Both ACC45 or ACC18 medical certificates can be included in this audit option as the patient may be presenting for the first time or a subsequent visit, e.g. doctors working in urgent care are more likely to see patients at first presentation and issue ACC45 medical certificates rather than ACC18 certificates.
Eligible patients
All patients who were issued an ACC18 “Fully unfit” or “Fit for selected work” medical certificate in the past 12 months are eligible for this audit. If the patient was issued more than one ACC18 medical certificate for the same claim over this period, you can use the most recent certificate issued or select one at random; be consistent with your selection method.
If conducting a working audit, any adult patient in paid employment who has had an accident resulting in injury, and who is not “Fully fit” for work, is eligible for this audit.
Identifying patients
You will need to have a system in place that allows you to identify eligible patients and audit their clinical notes. Many practices will be able to do this by running a “query” through their PMS to find all patients who have presented following an injury in the past 12 months. Keywords such as “ACC45”, “ACC18” or “accident” may be useful to include when building the query. The clinical notes of these identified patients will then need to be reviewed, and those issued a “Fully unfit” or “Fit for selected work” medical certificate selected for this audit.
If conducting a “working audit”, fill in the data sheet when you have a consultation for an injury-related reason with an eligible patient and issue either an ACC45 or ACC18 medical certificate, until the required number of patients has been reached.
Sample size
The number of eligible patients will vary according to your practice demographic. A sample size of 20 to 30 patients is sufficient for this audit.
If conducting a working audit, a smaller sample size may be necessary to complete it within your planned time frame.
Criteria for a positive outcome
For a positive result:
- Patients issued a “Fully unfit” medical certificate in the past 12 months should meet ACC criteria for this designation (refer to criteria in “Background” section)
- All other patients who did not meet ACC criteria for “Fully unfit” medical certification in the past 12 months were issued a “Fit for selected work” medical certificate (those issued a “Fully fit” certificate are not part of the eligible group for this audit)
- The percentage of patients issued a “Fully unfit” medical certificate should be less than those issued a “Fit for selected work” certificate: a specific target for this percentage is not possible to set due to the variable nature of injury assessment, but a reasonable target would be fewer than 50% and the lower the percentage, the more likely it is to reflect close adherence to the criteria
If conducting a working audit, a positive result is if the patient is issued a “Fully unfit” medical certificate only if they meet ACC criteria for this designation. The remaining patients who are not “Fully fit” for work should be issued a “Fit for selected work” medical certificate.
Data analysis
Use the sheet provided (Data sheet A or B) to record your data. The percentage achievement for both the main and secondary outcomes can be calculated by dividing the number of patients with a positive result by the total number of patients audited.
Optional: In practice, several factors may influence your decision when issuing medical certificates. The data sheets include options to record the justification for your decision, the injury type and the length of time each medical certificate was issued for. Clinicians may choose to include one or more of these options to record and analyse as part of their audit. It is encouraged to discuss your results with your colleagues as part of the reflection process. Can you identify any patterns and do these factors influence the designation of the medical certificate you issue?
Clinical audits can be an important tool to identify where gaps exist between expected and actual performance. Once completed, they can provide ideas on how to change practice and improve patient outcomes. General practitioners are encouraged to discuss the suitability and relevance of their proposed audit with their practice or peer group prior to commencement to ensure the relevance of the audit. Outcomes of the audit should also be discussed with the practice or peer group; this may be recorded as a learning activity reflection if suitable.
The Plan, Do, Study, Act (PDSA) model is recommended by the Royal New Zealand College of General Practitioners (RNZCGP) as a framework for assessing whether a clinical audit is relevant to your practice. This model has been widely used in healthcare settings since 2000. It consists of two parts, the framework and the PDSA cycle itself, as shown in Figure 1.
1. The framework
This consists of three questions that help define the “what” and “how” of an improvement project (in this case an audit).
The questions are:
- "What are we trying to accomplish?" – the aim
- "How will we know that a change is an improvement?" – what measures of success will be used?
- "What changes can we make that will result in improvement?" – the concept to be tested
2. The PDSA cycle
This is often referred to as the “engine” for creating, testing and carrying out the proposed changes. More than one cycle is usually required; each one is intended to be short, rapid and frequent, with the results used to inform and refine the next. This allows an ongoing process of continuous learning and improvement.
Each PDSA cycle includes four stages:
- Plan – decide what the change to be tested is and how this will be done
- Do – carry out the plan and collect the data
- Study – analyse the data, assess the impact of the change and reflect on what was learned
- Act – plan the next cycle or implement the changes from your plan
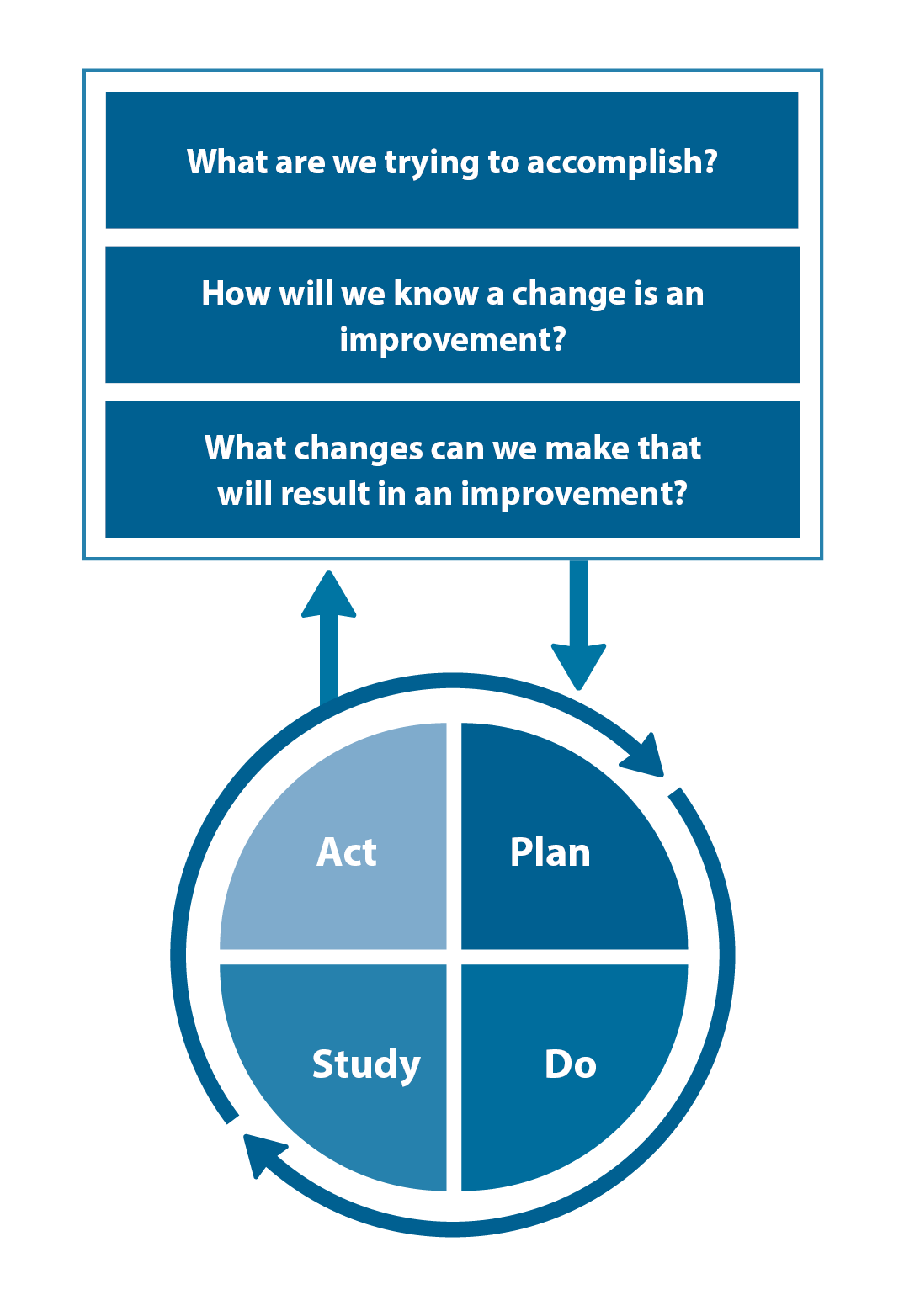
Figure 1. The PDSA model for improvement.
Source: Plan, Do, Study, Act (PDSA) cycles and the model for improvement

Claiming credits for Te Whanake CPD programme requirements
Practice or clinical audits are useful tools for improving clinical practice and credits can be claimed towards the Patient Outcomes (Improving Patient Care and Health Outcomes) learning category of the Te Whanake CPD programme, on a two credit per learning hour basis. A minimum of 12 credits is required in the Patient Outcomes category over a triennium (three years).
Any data driven activity that assesses the outcomes and quality of general practice work can be used to gain credits in the Patient Outcomes learning category. Under the refreshed Te Whanake CPD programme, audits are not compulsory and the RNZCGP also no longer requires that clinical audits are approved prior to use. The college recommends the PDSA format for developing and checking the relevance of a clinical audit.
To claim points go to the RNZCGP website: www.rnzcgp.org.nz
If a clinical audit is completed as part of Te Whanake requirements, the RNZCGP continues to encourage that evidence of participation in the audit be attached to your recorded activity. Evidence can include:
- A summary of the data collected
- An Audit of Medical Practice (CQI) Activity summary sheet (Appendix 1 in this audit or available on the
RNZCGP website).
N.B. Audits can also be completed by other health professionals working in primary care (particularly prescribers), if relevant. Check with your accrediting authority as to documentation requirements.
 This audit was supported by ACC.
This audit was supported by ACC.
