Prescriber responsibility and polypharmacy
It is increasingly recognised that health care for older people is improved when one prescriber takes responsibility
for all of a patient's medicines.1 An important reason for this is that multiple prescribers are associated
with increased polypharmacy (Figure 1). This exposes patients to increased risk, as the probability of an adverse drug
reaction occurring increases as the patient takes more medicines.2 Multiple prescribers are also an independent
risk factor for adverse drug reactions in older populations.3
Polypharmacy among older populations is also significantly associated with hypoglycaemia, malnutrition, pneumonia, fractures,
hospitalisation and death.5 An analysis of national dispensing data showed that 44% of enrolled patients aged
over 75 years in New Zealand used five or more medicines continuously over a nine month period in 2011/2012.4
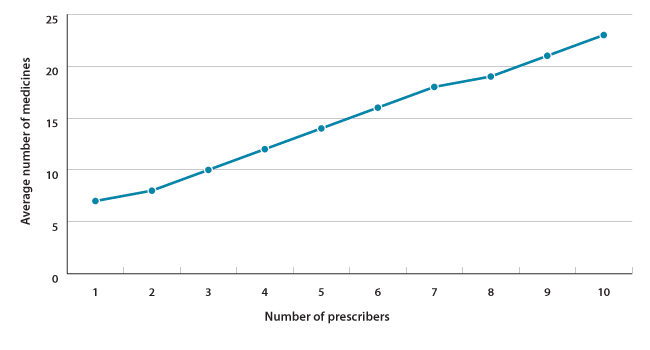
Figure 1: Average number of medicines prescribed per patient (Jul 2011 - Mar 2012) for all patients
aged over 75 years in New Zealand, by number of prescribers4
A single prescriber provides consistency
Oversight of medicines by a single prescriber allows for consistent advice and decision making. This is important when
treating elderly people, as prescribing recommendations are often based on studies of younger populations where co-morbidities
have been excluded. In older patients with complex co-morbidities, strict adherence to such guidelines can result in confusing
regimens with a high probability of adverse drug reactions.6 Prescribers need to tailor interventions to an
individual's overall risk, as the benefits gained by participants in clinical trials may not be generalisable to an older
person with multiple co-morbidities. In some cases, it may be jointly decided by patient and clinician to stop, or not
to initiate, treatment.
Adopting a standardised approach to prescribing for older people
Three essential elements of prescribing to older people in primary care are:
- The introduction of a standardised format when assessing medicine use
- Avoiding inappropriate prescribing
- The use of validated tools to withdraw unnecessary medicines
Standardising consultations with routine questions
What medicines are you currently taking?
Older people frequently have multiple co-morbidities and reduced renal and hepatic function. They are therefore more
likely to be affected by adverse drug reactions than younger people.
It is also important to find out if the patient is adhering to their prescribed medicines. Medicine non-adherence in
older people may occur due to forgetfulness, adverse effects, limited organisational skills or belief that the medicine
is unnecessary, ineffective or too costly.7 Reports of non-adherence in older people varies from one-quarter
to over one-half, depending on the definition and the population studied.7 Simple questions about what, why
and how patients take their medicines can reveal gaps in understanding and compliance that otherwise may not be volunteered.
Medicine organisers or blister packs may be introduced for patients who experience confusion or forget to take their medicines
regularly.
What medicines do you buy yourself and do you take medicines prescribed for anybody else? Some patients may not consider
products that they have purchased from the supermarket or health store as medicines. Specifically asking about medicine
purchasing habits may reveal relevant information. For example, an older person with chronic kidney disease taking angiotensin
converting enzyme inhibitors (ACEIs) and diuretics will be at increased risk of developing acute kidney injury if they
also take ibuprofen purchased from a supermarket.
Sharing of medicines is also common among older people. Survey results indicate that 13 - 20% of older people have shared
their medicine with another person.8
Over-the-counter (OTC) products and complementary and alternative medicines can also have significant interactions with
prescribed medicines, e.g. warfarin in combination with significant quantities of garlic, ginger, ginseng or ginkgo may
result in an increased risk of bleeding.9 One study of over 1000 people, with a mean age of 76 years, found
that approximately one-third of participants had complementary medicines in their home, with almost all of these in active
use.10 The most common potential adverse effects due to interactions between prescribed medicines and alternative
products were: increased risk of bleeding due to non-steroidal anti-inflammatory drugs (NSAIDs) interacting with vitamin
E, fish oils, ginkgo and garlic, or hyperkalaemia caused by ACEIs and concurrent use of potassium or
arginine supplements.10
Have you visited another doctor or been admitted to hospital?
Primary care management of medicines requires timely information about prescribing changes initiated in secondary care.
Asking patients if they have visited another health professional is a simple way of checking if their medicine regimen
has been altered. If the patient has had a consultation with another clinician, ask if they were prescribed any new medicines,
or if they were told that they could stop taking medicines that had been previously prescribed.
Hospital admission in older people is associated with an increase in the number of long-term medicines taken. A New
Zealand study of over 400 older people found that following a stay in hospital, the average number of medicines prescribed
to patients increased from 6.6 to 7.7.11 If secondary care prescribers are unaware of all the medicines a patient
is taking, the risk of prescription duplication and/or adverse drug reactions are increased. Furthermore, some medicines
initiated in secondary care may not be intended for long-term use, e.g. omeprazole taken for prophylaxis against stress
ulceration before surgery. Secondary care initiation of uncommon medicines can also present challenges to primary care
prescribers assessing the risk and benefits of continuing these medicines. Similarly, if secondary care prescribers are
unaware of the indications for continuing some medicines, e.g. antidepressants, appropriate treatment may be inadvertently
withdrawn.
 Best Practice tip: Practices may consider implementing a system where
older patients who have been recently discharged from hospital for non-routine events, are phoned and offered a follow-up
consultation to discuss any possible changes to their treatment.
Best Practice tip: Practices may consider implementing a system where
older patients who have been recently discharged from hospital for non-routine events, are phoned and offered a follow-up
consultation to discuss any possible changes to their treatment.
Do you have any concerns about any medicines you are taking?
Regularly assessing medicine effectiveness (including asking patients if they feel their medicines help) and monitoring
for adverse effects allows for appropriate dose adjustment and the risk of long-term adverse drug reactions to be minimised.
This question also provides a prompt for some older patients who may just "put up" with adverse effects without mentioning
them. Discussing concerns may also increase patients' health literacy and improve treatment adherence.
Actions and questions for prescribers
Medicines information gathered from consultations can be combined with information taken from patient records (including
hospital discharge notes and dispensing record) to reconcile the list of medicines a patient is taking.
Performing medicine reconciliations and medicine reviews
Medicine reconciliation is the systematic process of obtaining a complete list of all of a patient's medicines. It should
be performed whenever a patient is seen for the first time, or discharged from hospital. All medicines, including OTC
medicines, supplements and alternative products should be recorded in the PMS. This list should include doses, regimen,
administration routes and last dose taken.12 All drug allergies, intolerances and previous treatment terminations,
and the reasons for discontinuation, should also be recorded.
Many older patients take their medicines from blister packs and have limited knowledge about some medicines prescribed
to them. Suggesting that patients bring their medications to the consultation and performing a "brown-bag review" can
assist the reconciliation process.
Medicine reviews aim to eliminate medicines that are no longer required or have a high risk of toxicity. These should
be conducted annually for all older patients taking medicines and every six months for those taking multiple medicines,
e.g. five or more medicines taken simultaneously.1 However, thought should be given to the appropriateness
of medicines every time a prescription is renewed.
Pharmacist and/or nurse participation in the reconciliation process has been shown to be beneficial (see: "The Pharmacy
Services Agreement", below). A Canadian study found that in 120 patients aged over 50 years, following review by a pharmacist
and a nurse practitioner, the number of inappropriate medicines decreased from 27% to 9% and the number of patients taking
at least one inappropriate medicine decreased from 78% to 39%.13
Specifically trained clinical pharmacists can provide another level of expertise by contributing to medicine management
through clinical recommendation.
The Pharmacy Services Agreement - The changing role of the community pharmacist
Under the new Long Term Conditions (LTC) rules of the Pharmacy Services Agreement, community pharmacists will now be
identifying patients with complex co-morbidities and/or difficulties with medicine adherence. To assist pharmacists,
an objective assessment tool has been developed. Patients can be referred to be assessed by indicating "Refer for LTC
assessment" on a prescription or by contacting the pharmacist directly. Family members and patients themselves can also
request an LTC assessment.
Pharmacists will be funded to assist in the management of patients referred for LTC assessment. Part of the assessment
will be to determine dispensing frequency. Patients who are currently dispensed their medicines under Close Control can
remain on this dispensing frequency until they are assessed for LTC eligibility. Pharmacists have until 31 January 2013
to complete these assessments.
In addition to the LTC service, some DHBs are still funding medicine use reviews by accredited pharmacists to improve
patient education and adherence. To find out if this service is available in your area, contact your local DHB.
 For further information see: "New
service model for community pharmacy", BPJ 45 (Aug, 2012) or
www.pharmac.govt.nz/ccc
For further information see: "New
service model for community pharmacy", BPJ 45 (Aug, 2012) or
www.pharmac.govt.nz/ccc
Before prescribing a medicine, consider the following:
Am I treating the condition or a symptom? It is important to establish a diagnosis so that treatment will target the
underlying process rather than an isolated symptom. If a patient is taking multiple medicines, clinicians should exclude
the possibility that any new symptoms may be due to adverse drug reactions.
Be aware of the possibility of the prescribing cascade concept, which can begin when an adverse drug reaction is misinterpreted
as a new medical condition. This can result in a new medicine being unnecessarily prescribed to treat the adverse reaction
which in turn increases the risk of the patient experiencing another adverse drug reaction. An example of this is the
use of prochlorperazine for the treatment of dizziness in patients taking medicines such as antihypertensives.14 Prochlorperazine
is associated with postural hypotension and may exacerbate the original symptom and can also cause drug-induced parkinsonism.
These adverse effects may explain the resulting 50% increase in the observed rates of hip fracture in older people following
initiation of prochlorperazine.14
Have I considered non-pharmacological treatment? Non-pharmacological interventions, in some cases, can provide both
physical and psychological health benefits to older people, e.g. physiotherapy for chronic back pain. Improving nutrition
and physical activity can also reduce people's risk of chronic disease and increase their independence. The introduction
of mobility aids, e.g. a walking frame, may also improve quality of life.
 The Ministry of Health provide nutrition guidelines for healthy older
people, available from: www.health.govt.nz/search (key
words = nutrition older)
The Ministry of Health provide nutrition guidelines for healthy older
people, available from: www.health.govt.nz/search (key
words = nutrition older)
Is the medicine appropriate to the patient's condition and stage of life? When considering prescribing medicines to
older people it can be useful to group medicines into those that improve quality of life, e.g. analgesics, and those used
for disease prevention. The benefit of medicines that improve quality of life is clearly evident. However, preventative
interventions require (to some degree) the clinician convincing the patient, and themselves, that treatment will provide
benefit. For example, the Prospective Study of Pravastatin in the Elderly at Risk of vascular disease (PROSPER) trial
showed that while pravastatin given to over 5000 participants aged 70 - 82 years did reduce cardiovascular morbidity and
mortality, it was not associated with a reduction in all-cause mortality.17 This was partially explained by
an increased incidence of new cancer diagnosis, suggesting that for some patients, preventing one cause of death simply
revealed another. Some older patients, who had elected to take a statin to reduce cardiovascular risk for primary prevention,
may not have made the same decision if they had been told that treatment was unlikely to prolong their life. However,
aggressive statin treatment may be appropriate for a patient who has previously had a stroke and wishes to reduce the
risk of a second, potentially more disabling event from occurring.18 Clearly, discussions about medicines need
to be focused on the individual preferences of the patient and their specific circumstances and life stage.
Assessing prescription appropriateness
Factors which should be considered when prescribing medicines to older people include:19
- Remaining life expectancy (Table 1)
- Time until benefit of treatment
- Treatment target
- Goals of care
| Male |
Female |
| Age years |
Expected number of years of life remaining |
Age years |
Expected number of years of life remaining
|
| 65 |
18.8 |
65 |
21.2 |
| 70 |
15.0 |
70 |
17.1 |
| 75 |
11.5 |
75 |
13.3 |
| 80 |
8.6 |
80 |
9.8 |
| 85 |
6.2 |
85 |
6.9 |
| 90 |
4.5 |
90 |
4.8 |
Table 1: Life expectancy by age for older New Zealand male and female populations, 2009 - 201120
Consider using prescribing tools
Prescribing tools provide specific examples of medicines that may be inappropriate for older people and are an effective
way of reducing adverse drugs reactions.
The STOPP/START criteria were developed to improve prescribing to patients aged over 65 years. The criteria consist
of two components; the first to halt inappropriate or unnecessary medicines in older patients, the second is used to consider
medicine appropriateness when initiating treatment. An advantage of the STOPP/START criteria is that it accounts for patient
co-morbidities. The STOPP/START criteria was considered by an expert panel to be the most appropriate tool for measuring
treatment adherence and appropriateness in patients with multiple co-morbidities.12
 The STOPP/START toolkit can be accessed from:
www.cumbria.nhs.uk (key
words = STOPP/START).
The STOPP/START toolkit can be accessed from:
www.cumbria.nhs.uk (key
words = STOPP/START).
The Beers criteria consists of three lists of medicines ranked according to their potential for causing adverse reactions
in older people. It was recently updated by the American Geriatrics Society (AGS) in 2012.21 However, the criteria's
usefulness is limited as it does not take into account individual patient needs and co-morbidities.
The first grouping is medicines that are known to cause adverse reactions in older people. The second classification
is medicines that may be inappropriate for older people with specific diseases or risks factors. The third list is medicines
that should be prescribed to older people with caution.
 For further information see the American Geriatrics Society. Available
from: www.americangeriatrics.org (keyword search = Beers).
For further information see the American Geriatrics Society. Available
from: www.americangeriatrics.org (keyword search = Beers).
The New Zealand Formulary (NZF) presents two options for obtaining information about medicine interactions:
- Stockley's Interaction Alerts
- British National Formulary (BNF) interaction summaries
 For further information see: "Medicine
interactions: using the New Zealand Formulary", BPJ 46 (Sep, 2012).
For further information see: "Medicine
interactions: using the New Zealand Formulary", BPJ 46 (Sep, 2012).
The danger of under-prescribing
Under-prescribing is the omission of medicines which are generally recommended by clinical guidelines for the treatment
or prevention of a disease or condition.15 A study of 123 patients aged over 60 years found that approximately
one-third of instances of under-prescribing were not clearly justified.15
Commonly under-prescribed treatments for older people include medicines for the secondary prevention of coronary and
cerebrovascular diseases and osteoporotic fractures.8 In particular, there is good evidence of short-term
benefits gained from continuing treatment of hypertension in people aged over 80 years.16
Although inappropriate under-prescribing should be avoided, it is complicated by the fact that clinical guidelines
are generally for single conditions and do not take into account co-morbidities. The use of several different guidelines
for one patient with multiple conditions may lead to inappropriate prescribing, if all advice is followed concurrently.6
If prescribers are unsure whether a medicine is appropriate for an older patient then discussion with a geriatrician,
general physician or clinical pharmacist is recommended.
When medicines are prescribed
Consider if there are any medicines that can be altered or stopped if a new medicine is started, e.g. if the patient
is switched from an NSAID to an opioid, a gastro-protective medicine may no longer be necessary.
If repeating a prescription, confirm that the original is still applicable, e.g. if a loading dose of colecalciferol
has been prescribed, check that subsequent prescriptions do not repeat the loading dose.
Double check the prescription is correct both before printing it out and handing it to the patient.
Ensure the patient knows what medicine they have been prescribed and how it should be taken. Where appropriate, encourage
people to take educational material home about both the medicine prescribed and the condition being treated. This can
increase patient understanding and family/ whānau involvement in treatment.
When finishing a consultation a good approach to see if the patient has understood a message is to ask them what they
will say to their partner or family when they return home.
 The Ministry of Health website provides information and links to patient
resources for diseases that are common in older people, e.g. cardiovascular disease, cancer and diabetes. See:
www.health.govt.nz
The Ministry of Health website provides information and links to patient
resources for diseases that are common in older people, e.g. cardiovascular disease, cancer and diabetes. See:
www.health.govt.nz
Regular monitoring for adverse effects and treatment adherence
It has been suggested that suboptimal monitoring of older people taking medicines may be a more significant problem
than inappropriate prescribing.8 Effective monitoring requires regular recording of parameters such as body
weight and blood pressure, scheduling of relevant laboratory tests, e.g. serum creatinine and HbA1c, regular
communication between patient and clinician and a good knowledge of the patient's cognitive function and general wellbeing.
When to decide to withdraw a medicine
Medicine withdrawal should be considered for older people when:22
- There are a large number of medicines in use
- Adverse drug reactions are suspected or falls have occurred
- Treatment is ineffective
- The goals of care change due to declining organ function
A study investigating inappropriate medicine use in 70 community dwelling older people recommended discontinuation of
311 medications in 64 people.23 Of the medicines that were discontinued, only 2% were restarted due to the
recurrence of the original indication.23
Medicine groupings that may be appropriate for withdrawal in older people include; anticholinergics, antihistamines,
antiplatelet medicines, centrally acting medicines (e.g. antipsychotics, benzodiazepines), diuretics, NSAIDs, proton pump
inhibitors and vasodilators.
 For further information see: "A
practical guide to stopping medicines in older people", BPJ 27 (Apr, 2010).
For further information see: "A
practical guide to stopping medicines in older people", BPJ 27 (Apr, 2010).
If a medicine is withdrawn due to a suspected adverse drug reaction, symptom resolution can be expected once the medicine
has been cleared from the patient's blood (within three to five half-lives) - if the reaction is dose dependent.22 Symptoms
such as delirium and skin reactions and those caused by renal or hepatotoxicity may take considerably longer to resolve.
The "Pill Pruner"
A medication review guide for frail, older patients, the Pill Pruner, has been developed in New Zealand. The guide
condenses the STOPP/START criteria into the 13 most potentially inappropriate medicines relevant to New Zealand prescribing
practice. These are printed on a pocket-sized card.
The Pill Pruner was tested at Christchurch Hospital on two groups of 500 people aged over 75 years, consecutively admitted
to hospital. On admission, over 70% of patients were taking five or more medicines. Before the Pill Pruner was introduced,
the mean number of medicines on discharge increased from 6.8 to 7.7. When the Pill Pruner was introduced, no statistically
significant increase in discharge medicines occurred (medicines increased from 6.3 to 6.5). Over the course of the study
over 1000 medicines were stopped including: loop diuretics, antiplatelet medicine, statins, ACEIs, β-blockers and
benzodiazepines. There appeared to be no harmful effects of medicine withdrawal. Medicine changes were communicated to
the patient's General Practitioner and community pharmacist. Of the General Practitioners who responded to follow-up
questionnaires, less than 10% reported a need to restart medicines in patients.
The Pill Pruner has yet to be trialled in primary care. As hospital admission is frequently a period of acute illness
and increased need, use of the Pill Pruner in general practice may be even more effective. Publication of the results
of the Pill Pruner study is underway.

For further information see: "Polypharmacy in the elderly - evaluating the
Pill Pruner project." Available from:
http://www.otago.ac.nz/christchurch/research/populationhealth/studentships/
How to "de-prescribe" and issues to be aware of
Before "de-prescribing" an unnecessary medicine, a discussion should be held with the patient as to why the change
has been suggested and what can be expected. This is important, as many medicines have a placebo component to their effectiveness.
Explain that the process will be monitored.
If there is more than one medicine to be de-prescribed, these should be prioritised and withdrawn one at a time. The
dose should be slowly reduced over a period of weeks to months and the patient warned and monitored for signs of:22
- Withdrawal - common in medicines acting on the central nervous system
- Rebound symptoms - e.g. rebound tachycardia and hypertension following beta blocker withdrawal, or rebound gastric
acid secretion following withdrawal of a proton pump inhibitor
- Unmasked drug interactions - e.g. the INR of a normally stable patient taking warfarin may decrease over several
weeks following cessation of amiodarone
Clinicians should consider if any new symptoms are due to withdrawal or a re-emergence of the indicated condition.
If the patient experiences significant withdrawal, the medicine can be reintroduced, possibly at a reduced dose. Assessments
should also focus on the beneficial aspects of de-prescribing, which can reinforce patient adherence and the prescriber's
confidence to reduce medicines.