Published: October, 2024 | Review date: October, 2027
This audit assesses use of the ABC pathway for encouraging smoking cessation in primary care. It identifies whether:
- Smoking status is routinely documented for patients; and
- If those identified as smokers have been provided with brief advice to quit and offered cessation support.
Smoking rates have been steadily declining in New Zealand for at least a decade. In 2022/23, approximately 7% of people reported being daily smokers, down from 9% in 2021/22, and 16% in 2011/12.1 Decreases have been observed across all ethnic groups over time, however, inequity still persists, with daily smoking rates being comparatively higher among Māori (17%) and adults living in the most deprived communities (11%).1 There are also concerns around the effects of second-hand smoke exposure, which is still estimated to impact 3.2% of adults and children in New Zealand.2
Smoking is associated with a higher burden of disease than any other behavioural risk factor; there is no “safe” level of use. Despite these considerable harms, evidence suggests that cessation has both immediate and long-term benefits on a person’s health and quality of life.3 The greatest effect is achieved by people who quit at a younger age, however, quitting smoking at any age will lower the risk of morbidity and mortality. General practice is well placed to help people take the first step toward smoking cessation and most people who smoke want to quit and anticipate being asked questions about their smoking status by healthcare professionals.
For further information on smoking cessation, see: bpac.org.nz/2024/smoking.aspx
ABC: Ask, Brief advice, Cessation support
Ask, Brief advice, Cessation support (ABC) remains the standard of care for helping people to quit smoking. The ABC pathway can be easily integrated into everyday practice so that smokers are presented with abundant opportunities to quit:4
- Ask about the smoking status of every patient and document this information in their clinical record
- Briefly advise every person who smokes to stop, regardless of their desire or motivation to quit
- Cessation support should be discussed and strongly encouraged for every person who smokes. Healthcare professionals should offer to help patients access cessation support services, i.e. refer them or explain how they are accessed. Briefly explain the options available to improve the probability of success; the best results are achieved when clinicians both offer behavioural support and prescribe smoking cessation medicines (see: “Nicotine replacement therapy is useful for almost everyone who smokes”).
There is no set manner in which the brief advice to quit needs to be given. However, advice should always be tailored to the specific patient and their circumstances and it is important to correct any mistaken beliefs early. Opening with positive or gain-framed statements is a more successful strategy than the use of loss-framed statements, e.g. focus on the health and quality of life benefits, financial savings and encourage patients that cravings decrease over time, rather than saying “smoking harms your health”. As with the documentation of smoking status, it is important to record whether patients have been offered brief advice to quit and help accessing smoking cessation suppport (see codes below).
Codes for patient smoking status
| |
Definition
|
SNOMED CT term
|
SNOMED CT code
|
Read code
|
|
Non-smoker
|
Smoked fewer than 100 cigarettes in lifetime (including hand rolled cigarettes, cigars, cigarillos)
|
Never smoked
|
266919005
|
1371
|
|
Ex-smoker
|
Smoked more than 100 cigarettes in lifetime but has not smoked in the previous 28 days
|
Ex-smoking for less than 1 year*
|
735128000
|
137K
|
|
Ex-smoking for more than 1 year
|
48031000119106
|
137S
|
|
Current smoker
|
Smoked more than 100 cigarettes in lifetime and has smoked in the previous 28 days
|
Currently smoking
|
77176002
|
137R
|
N.B. Vaping status should also be routinely considered in addition to smoking status. For codes, see: www.health.govt.nz/strategies-initiatives/programmes-and-initiatives/smokefree-2025/information-for-practitioners-of-patients-who-are-quitting-smoking/recording-vaping-status
Codes for other aspects of the ABC pathway
| |
SNOMED CT term
|
SNOMED CT code
|
Read code
|
|
Delivery of brief advice to stop smoking
|
Brief smoking cessation advice
|
771155005
|
@ZPSB.10
|
|
Referral to stop smoking support
|
Referral to stop smoking support
|
395700008
|
@ZPSC.10
|
|
Provided smoking cessation support
|
Smoking cessation behaviour support
|
384742004
|
@ZPSC.30
|
|
Prescribed smoking cessation medicine
(e.g. NRT; see next section)
|
Smoking cessation medication
|
713700008
|
@ZPSC.20
|
|
Refused smoking cessation support
|
Smoking cessation advice declined
|
57861000210104
|
@ZPSC.90
|
Nicotine replacement therapy is useful for almost everyone who smokes
NRT can be safely used by almost anyone who wants to quit smoking and works by providing some of the nicotine the patient is used to without the additional toxic substances.3 Most patients trying to quit smoking do not use enough NRT and therefore have a higher risk of withdrawal symptoms; treatment with multiple forms (e.g. patches plus gum or lozenges) is advised in those with higher levels of nicotine dependence.3, 5 Combination NRT approximately doubles a patient’s chances of quitting smoking versus control.6
If required, there are also other pharmacological options to help support smoking cessation, including buproprion, nortriptyline and varenicline. Varenicline is the most effective of these alternative treatments and is funded with Special Authority approval for patients who have previously tried to quit with other smoking cessation medicines. However, varenicline has been out of stock in New Zealand for some time; it is reported by Pharmac that it may be restocked in late March, 2025.
References:
- Ministry of Health. Annual update of key results 2022/23: New Zealand Health Survey. 2023. Available from: https://www.health.govt.nz/publication/annual-update-key-results-2022-23-new-zealand-health-survey (Accessed Oct, 2024).
- Environmental Health Intelligence New Zealand (ehinz). Second-hand smoke exposure. 2024. Available from: https://www.ehinz.ac.nz/indicators/indoor-environment/second-hand-smoke-exposure-2/ (Accessed Oct, 2024).
- Royal Australian College of General Practitioners (RACGP). Supporting smoking cessation: A guide for health professionals. 2024. Available from: https://www.racgp.org.au/clinical-resources/clinical-guidelines/key-racgp-guidelines/view-all-racgp-guidelines/supporting-smoking-cessation (Accessed Oct, 2024).
- Ministry of Health. The New Zealand guidelines for helping people stop smoking. 2021 Update. Available from: https://www.health.govt.nz/strategies-initiatives/programmes-and-initiatives/smokefree-2025/information-for-practitioners-of-patients-who-are-quitting-smoking/recording-vaping-status (Accessed Oct, 2024).
- Ministry of Health. Guide to prescribing nicotine replacement therapy (NRT). 2021. Available from: https://www.health.govt.nz/system/files/2014-06/guide-to-prescribing-nicotine-replacement-therapy-2021.pdf (Accessed Oct, 2024).
- Lindson N, Theodoulou A, Ordóñez-Mena JM, et al. Pharmacological and electronic cigarette interventions for smoking cessation in adults: component network meta-analyses. Cochrane Database of Systematic Reviews 2023;2023. doi:10.1002/14651858.CD015226.pub2
Summary
The audit involves sampling two groups of patients from your practice. The first group is used to calculate the percentage of patients who have had their smoking status recorded. The second group is a sample of patients recorded as current smokers and is used to calculate the percentage who have been offered brief advice and cessation support.
Recommended audit standards
Given the significance of smoking as a modifiable risk factor for disease, recording smoking status for all patients, and offering quit advice and help with accessing cessation support to every person who smokes, are important goals of primary care.
Any adult patients who do not have smoking status information in their clinical notes should be flagged for review. In addition, patients who are current smokers who have not been offered quit advice and help with accessing cessation support should be flagged for review. There should ideally be an improvement in the achieved percentage between the first and second audit cycles.
Eligible patients
This audit has two sample groups: all patients within the practice aged 18 years and older* are eligible for Group 1, and all patients recorded as current smokers (regardless of age) are eligible for Group 2.
* 18 years has been selected as the lower age for this audit, however, some clinicians may choose to use a lower age cut off depending on their patient population.
Identifying patients
Two samples need to be identified for this audit. The first group can be randomly selected from patients aged 18 years and older in the practice register. The second group can be identified by running a query through the PMS for enrolled patients coded as current smokers (see: “Codes for patient smoking status”).
Sample size
It is recommended that 30 patients are randomly selected and audited for each group.
Criteria for a positive outcome
A patient is considered a “positive result” for the purposes of the audit if:
- Group 1 – they have their current smoking status recorded in their patient notes (see: “Codes for patient smoking status”)
- Group 2 – they were given brief advice on smoking cessation within the last 12 months and were offered smoking cessation support within the last 12 months (see: “Codes for other aspects of the ABC pathway”)*
* Face-to-face delivery is ideal, but offers of support can be delivered over the phone if this is not possible, e.g. time constraints, patients without regular appointments. Sending texts or letters can only be considered an offer of support (and coded as such) if the patient replies, either to decline or accept/seek further information.
Data analysis
Use the data sheet provided to record your data. A positive result for Group 1 is any patient who has a “Yes” in column “A”. A positive result for Group 2 is any patient who has a “Yes” in both columns “B” and “C”.
Clinical audits can be an important tool to identify where gaps exist between expected and actual performance. Once completed, they can provide ideas on how to change practice and improve patient outcomes. General practitioners are encouraged to discuss the suitability and relevance of their proposed audit with their practice or peer group prior to commencement to ensure the relevance of the audit. Outcomes of the audit should also be discussed with the practice or peer group; this may be recorded as a learning activity reflection if suitable.
The Plan, Do, Study, Act (PDSA) model is recommended by the Royal New Zealand College of General Practitioners (RNZCGP) as a framework for assessing whether a clinical audit is relevant to your practice. This model has been widely used in healthcare settings since 2000. It consists of two parts, the framework and the PDSA cycle itself, as shown in Figure 1.
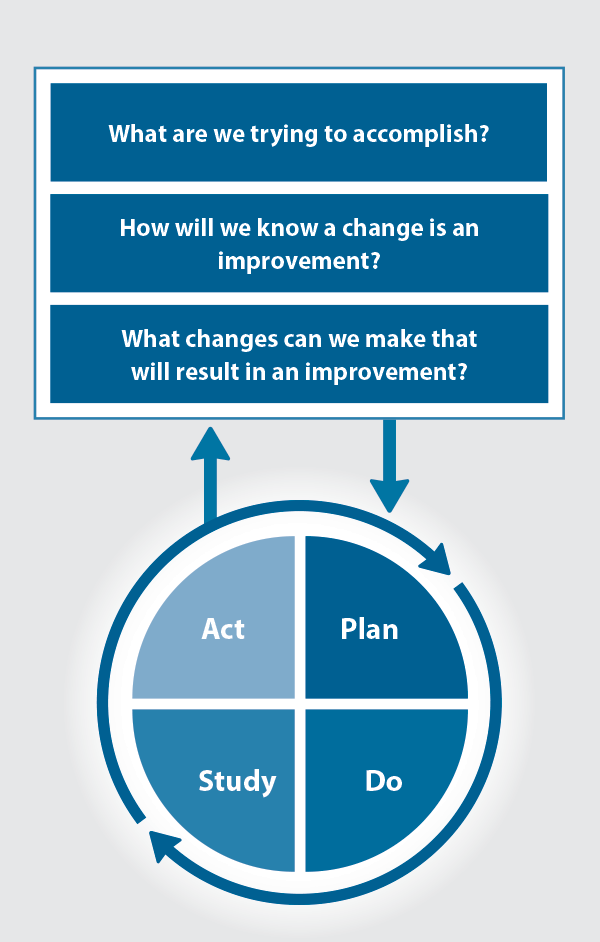
Figure 1. The PDSA model for improvement.
Source: Plan, Do, Study, Act (PDSA) cycles and the model for improvement
1. The framework
This consists of three questions that help define the “what” and “how” of an improvement project (in this case an audit).
The questions are:
- "What are we trying to accomplish?" – the aim
- "How will we know that a change is an improvement?" – what measures of success will be used?
- "What changes can we make that will result in improvement?" – the concept to be tested
2. The PDSA cycle
This is often referred to as the “engine” for creating, testing and carrying out the proposed changes. More than one cycle is usually required; each one is intended to be short, rapid and frequent, with the results used to inform and refine the next. This allows an ongoing process of continuous learning and improvement.
Each PDSA cycle includes four stages:
- Plan – decide what the change to be tested is and how this will be done
- Do – carry out the plan and collect the data
- Study – analyse the data, assess the impact of the change and reflect on what was learned
- Act – plan the next cycle or implement the changes from your plan

Claiming credits for Te Whanake CPD programme requirements
Practice or clinical audits are useful tools for improving clinical practice and credits can be claimed towards the Patient Outcomes (Improving Patient Care and Health Outcomes) learning category of the Te Whanake CPD programme, on a two credit per learning hour basis. A minimum of 12 credits is required in the Patient Outcomes category over a triennium (three years).
Any data driven activity that assesses the outcomes and quality of general practice work can be used to gain credits in the Patient Outcomes learning category. Under the refreshed Te Whanake CPD programme, audits are not compulsory and the RNZCGP also no longer requires that clinical audits are approved prior to use. The college recommends the PDSA format for developing and checking the relevance of a clinical audit.
To claim points go to the RNZCGP website: www.rnzcgp.org.nz
If a clinical audit is completed as part of Te Whanake requirements, the RNZCGP continues to encourage that evidence of participation in the audit be attached to your recorded activity. Evidence can include:
- A summary of the data collected
- An Audit of Medical Practice (CQI) Activity summary sheet (Appendix 1 in this audit or available on the
RNZCGP website).
N.B. Audits can also be completed by other health professionals working in primary care (particularly prescribers), if relevant. Check with your accrediting authority as to documentation requirements.
