In this report 
View / Download pdf version of this report
The use of multiple medicines in older people with co-morbidities can be beneficial. However,
when the number of medicines concurrently used reaches five or more there is a pronounced risk of medicine errors1 and
adverse effects. This report will discuss polypharmacy in people aged over 75 years using data from the Ministry of Health
National Collections2,3 for all subsidised medicines dispensed between July 2011 and March 2012, and all registered
patients in New Zealand in the first quarter of 2012.
Definition of polypharmacy
This report focuses on continuous polypharmacy, which is the chronic use of multiple medicines over a long period of
time.1 This is an internationally accepted definition of measuring polypharmacy. It does not identify the number
of medicines patients are taking on a given day, but has the advantage of identifying long-term use of multiple medicines,
which poses a significant problem for General Practitioners.4 To analyse the prevalence of continuous polypharmacy
for patients aged over 75 years in New Zealand, data was collected for three three-month periods: July-September and October-December
2011 and January-March 2012. A medicine was included as contributing to polypharmacy if it was dispensed to the patient
in all three of the three-month periods.4 For the purposes of this report, combination medicines, such as an
ACE inhibitor plus diuretic, were classified as a single medicine.
Polypharmacy is common in people aged over 75 years
The medicines dispensed for 254,249 registered patients aged over 75 years in New Zealand were identified during the
nine months from July 2011 to March 2012.
| 79% |
of registered patients aged over 75 years were dispensed at least one medicine continuously, of those patients: |
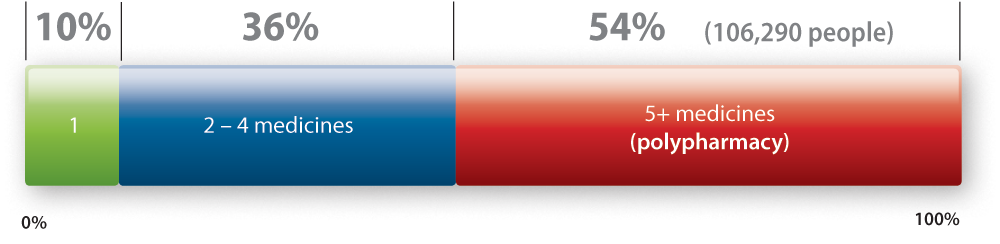
National data Prevalence of polypharmacy in people aged over 75 years
Multiple prescribers are associated with polypharmacy in people aged over 75 years
Patients who consult with multiple health providers are more likely to be prescribed multiple different medicines, and
therefore are at an increased risk of adverse medicine effects and interactions.
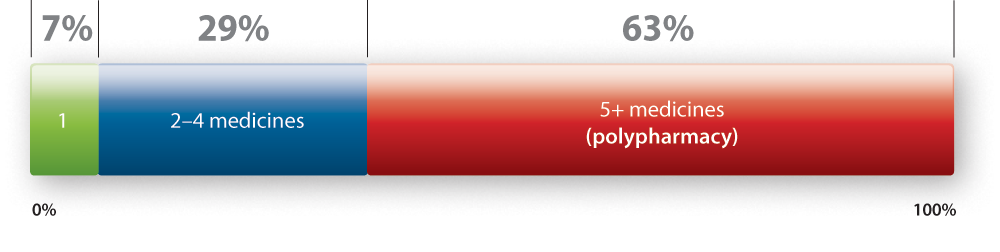
In New Zealand, 9% of all patients aged over 75 years were prescribed medicines by more than five health providers,
and 63% of those patients had polypharmacy (i.e. prescribed five or more different medicines continuously in the nine
month period). This represents a vulnerable patient group, that would benefit from individual management of their medicines.
National data Prevalence of polypharmacy in patients with five or more
prescribers
Polypharmacy in patients aged over 75 years at Sample Practice
100
patients aged over 75 years were dispensed at least one medicine continuously |
10%
of these patients were prescribed medicine by five or more health providers |
Polypharmacy in your registered patients aged over 75 years:
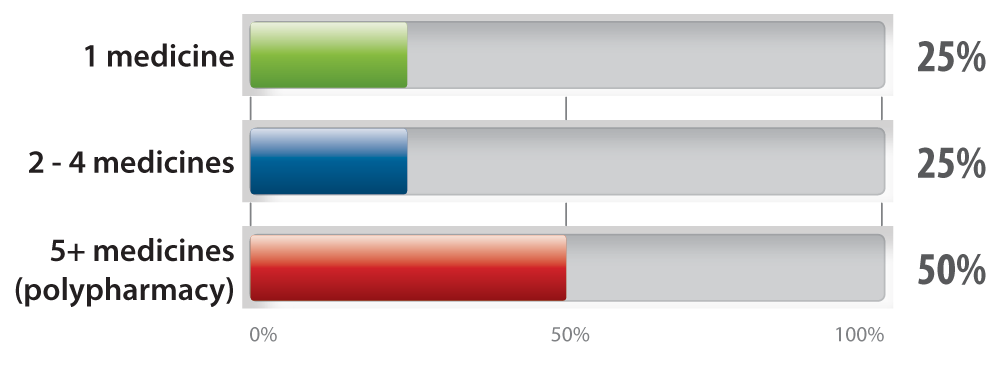 This
data includes prescribing by any New Zealand health provider including those who do not work in your practice. This
data includes prescribing by any New Zealand health provider including those who do not work in your practice. |
N.B. Some figures may not total 100% due to rounding.
- Bjerrum L, Rosholm JU, Hallas J, Kragstrup J. Methods for estimating the occurrence of polypharmacy by means of a
prescription database. Eur J Clin Pharmacol 1997;53:7-11
- Ministry of Health. Primary Health Organisation Enrolment Collection. (Accessed Aug, 2012).
- Ministry of Health. Pharmaceutical Collection. (Accessed Aug, 2012).
- Grimmsmann T, Himmel W. Polypharmacy in primary care practices: an analysis using a large health insurance database.
Pharm Drug Saf 2009;18:1206-13.