
B-QuiCK: Smoking cessation
Follow the ABC pathway principles to encourage smoking cessation
Ask about the smoking status of every patient and document this information in their clinical record. The patient’s smoking status should be re-assessed regularly (e.g. annually), particularly among patients aged under 30 years, or anyone identified as being a current smoker or ex-smoker.
| |
Definition
|
SNOMED CT term
|
SNOMED CT code
|
Read code
|
|
Non-smoker
|
Smoked fewer than 100 cigarettes in lifetime (including hand rolled cigarettes, cigars, cigarillos)
|
Never smoked
|
266919005
|
1371
|
|
Ex-smoker
|
Smoked more than 100 cigarettes in lifetime but has not smoked in the previous 28 days
|
Ex-smoking for less than 1 year |
735128000
|
137K
|
|
Ex-smoking for more than 1 year
|
48031000119106
|
137S
|
|
Current smoker
|
Smoked more than 100 cigarettes in lifetime and has smoked in the previous 28 days
|
Currently smoking
|
77176002
|
137R
|
Briefly advise every person who smokes to stop, regardless of their desire or motivation to quit. Opening with positive or gain-framed statements is preferable, e.g. focus on the health and quality of life benefits, financial savings and reassure patients that cravings decrease over time, rather than saying “smoking harms your health”. Record the delivery of advice in the clinical record.
| |
SNOMED CT term
|
SNOMED CT code
|
Read code
|
|
Delivery of brief advice to stop smoking
|
Brief smoking cessation advice
|
771155005
|
@ZPSB.10
|
Cessation support should be discussed and strongly encouraged for every person who smokes (at least annually). Healthcare professionals should offer to help patients access cessation support services, i.e. refer them or explain how they are accessed. Quitline is the main national smoking cessation service provider, available all hours. There are also a wide range of local “stop smoking services” (see: https://www.smokefree.org.nz/help-advice/stop-smoking-services). Document whether the patient accepts or declines smoking cessation support.
| |
SNOMED CT term
|
SNOMED CT code
|
Read code
|
|
Referral to stop smoking support
|
Referral to stop smoking support
|
395700008
|
@ZPSC.10
|
|
Provided smoking cessation support
|
Smoking cessation behaviour support
|
384742004
|
@ZPSC.30
|
|
Prescribed smoking cessation medicine
|
Smoking cessation medication
|
713700008
|
@ZPSC.20
|
|
Refused smoking cessation support
|
Smoking cessation advice declined
|
57861000210104
|
@ZPSC.90
|
Discussion points for addressing perceived barriers to smoking cessation
Perceived barrier (from patient)
Including mistaken beliefs or perspectives
|
Potential response or strategy to address barrier
(from healthcare professional)
|
|
Concerns that it is too hard to quit
|
- Discuss why previous smoking cessation attempts (if any) were not successful, and what could be done differently next time
- Emphasise that external support (e.g. from the primary care team, Quitline, local services) and medicines can significantly improve the success of quit attempts
|
|
Fear that it is too late to quit and derive health benefits
|
- Explain that health benefits still occur at any age; these are both immediate and long-term
- Emphasise other quality of life benefits
- Provide evidence and feedback, e.g. use a CVD risk calculator and alter status from current smoker to previous smoker, use case studies to outline health benefits obtained by others
|
|
Apprehension about cravings and withdrawal symptoms, e.g. irritability, low mood/anxiety, restlessness, poor concentration, increased appetite, difficulty sleeping
|
- Reassure them that withdrawal symptoms are transient; most peak within days of smoking cessation, and disappear completely within 2 – 4 weeks
- Not everyone gets every withdrawal symptom
- NRT helps reduce the severity of withdrawal symptoms
- Plan a course of action for dealing with cravings, e.g. the “4 Ds”: delay, deep breaths, drink water, do something else
|
|
Belief that using NRT is a sign of weakness and not necessary
|
- Reframe the purpose of NRT support; it is providing the chemical their body is already used to (nicotine) without the other toxic components in cigarettes
- Highlight the difference in smoking cessation success rates with and without NRT
|
|
Belief that smoking helps reduce stress and improves their mood/mental health
|
- Explain that nicotine drives changes in the brain that cause stress in its absence (i.e. it causes stress rather than reliving it); each cigarette further contributes to this cycle of dependence
- Identify triggers for smoking and discuss other potential relaxation strategies
|
|
Concerns over potential weight gain
|
- Acknowledge that on average people gain 2 – 4 kg when quitting, but it is usually not permanent and substantial weight gain is uncommon. There are multiple contributors to weight gain after cessation, e.g. slower metabolism and increased appetite due to nicotine withdrawal, “snacking” in the place of smoking in response to cravings, food tastes/smells better
- Discuss approaches to minimise weight gain and that this may also be a good time to make other positive lifestyle changes, e.g. improve diet, increase exercise
- Highlight that even if patients gain weight, they will still be “fitter” i.e. their breathing/heart rate during daily activities will improve
|
|
Apprehension around peer and social pressure
|
- Suggest avoiding high risk situations early in the quit attempt, if possible, e.g. drinking alcohol, social encounters with others who smoke
- Rehearse ways to say no to cigarettes if offered and encourage them to ask people to stop offering cigarettes
- Having a “quit buddy”, if possible
|
Offer pharmacological cessation support to all patients who want to quit smoking
(in additional to behavioral support)
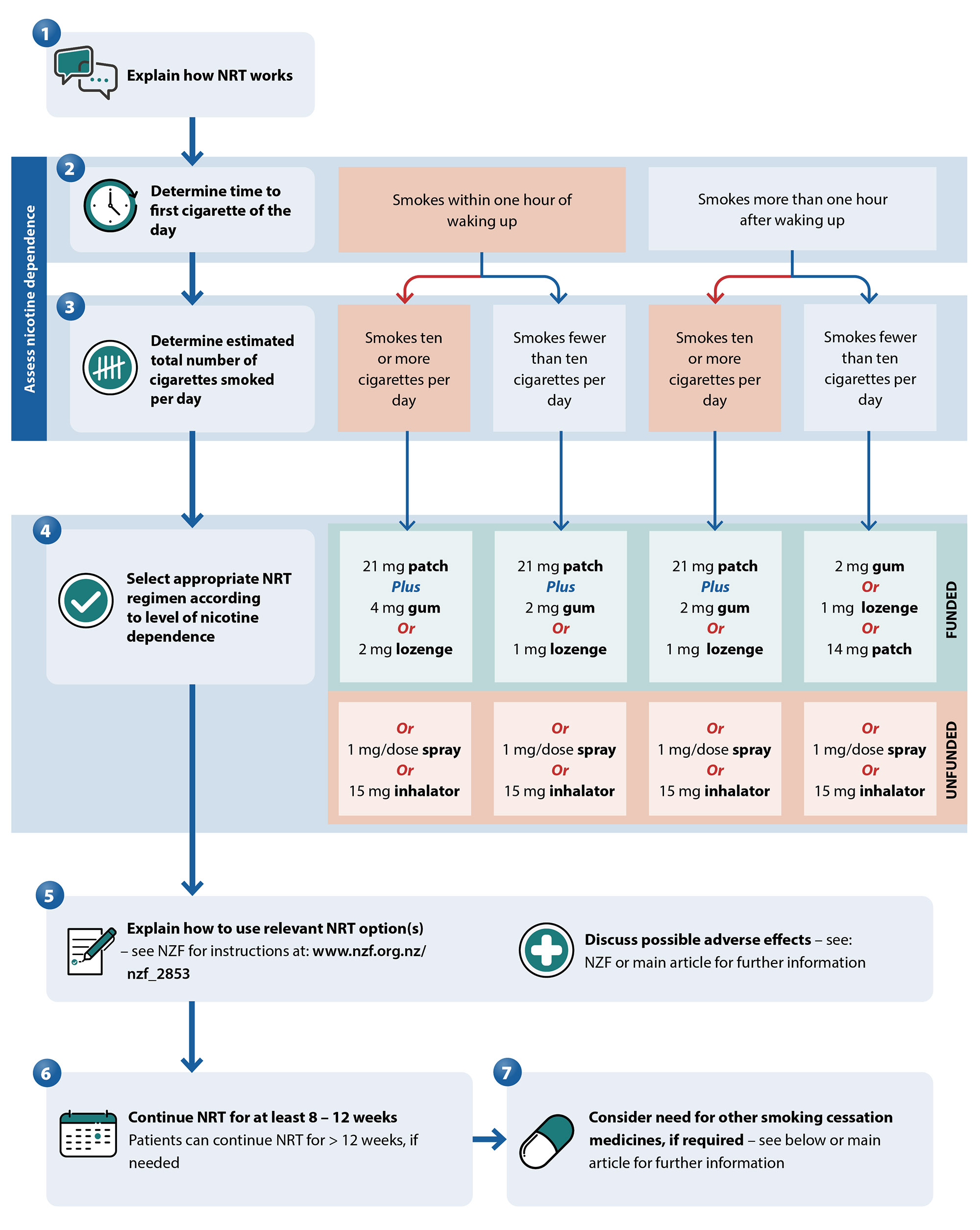
Nicotine replacement therapy (NRT) is generally the first medicine(s) used
Other smoking cessation medicines may be appropriate for patients who prefer quitting using a medicine that does not contain nicotine, or as second-line options.
They are not used in combination with each other, and generally are not used at the same time as NRT. See NZF for contraindications.
|
Bupropion |
Nortriptyline |
Varenicline* |
Step 1 |
Set a quit date |
Step 2 |
Initiate bupropion one to two weeks before quit date, initially at a dose of 150 mg, once daily |
Initiate nortriptyline 10 – 28 days before quit date, initially at a dose of 25 mg daily |
Initiate varenicline one to two weeks before quit date, initially at a dose of 500 micrograms, once daily, for the first three days |
Step 3 |
After three days, increase the dose to 150 mg, twice daily (minimum of eight hours between doses)† |
Increase the dose gradually over ten days to five weeks to 75 – 100 mg |
Increase the dose to 500 micrograms, twice daily, for four days |
Step 4 |
Continue use of 150 mg, twice daily, for at least seven weeks in total (longer durations are acceptable, if needed, e.g. up to 12 weeks) |
Continue use for three months in total (can be continued for up to six months, if required) |
Increase the dose to 1 mg, twice daily |
Step 5 |
|
|
Most patients should continue with this maintenance dose for 11 weeks. However, if not tolerated, reduce to 500 micrograms, twice daily. |
* Special Authority approval criteria applies for funded access. Varenicline has been unavailable in New Zealand for some time. It has been reported that it may be back in stock by late March, 2025.
† Maximum daily dose is 150 mg in older frail patients, those with risk factors for seizures, or in patients with renal/hepatic dysfunction.
Vaping is not an “official” smoking cessation tool, but essentially acts as a form of NRT (i.e. delivering nicotine without the other toxic components in cigarettes). However, long-term safety is uncertain, and depending on the nicotine concentration and daily liquid volume used, vaping can still result in significant nicotine intake. If switching to vaping is being considered as a strategy to quit smoking, discuss these issues with patients before they start vaping and help estimate the maximum amount of nicotine they should be vaping if they switch (based on their current level of smoking). Establish a plan to subsequently quit vaping too.
A New Zealand vaping cessation guide and background evidence review has just been released (Oct, 2024); it is available on the National Training Service website: www.nts.org.nz.





