Delaying skin deterioration in older patients: managing dry skin
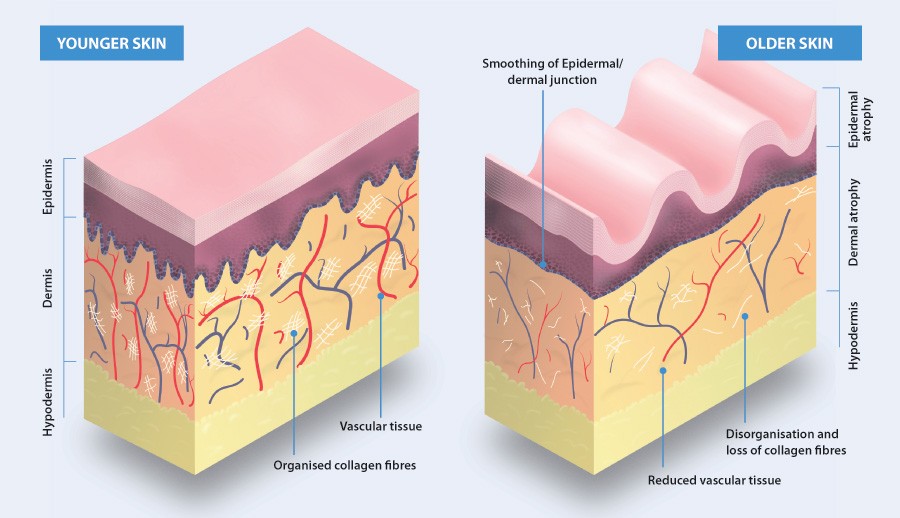
As skin ages, the epidermis and dermis become thinner and flatter and the skin’s mechanical strength declines.1 There
is a reduction in the number of cutaneous blood vessels and nerve endings, and in the amount of connective tissue, which
contains collagen and elastin.1 The skin has a decreased ability to retain moisture, to control temperature
and to sense the surrounding environment.1 Environmental factors, such as exposure to UV radiation, also have
a detrimental effect on skin health over time.
Skin management in older people focuses on preventing or delaying damage and monitoring skin regularly. Prevention includes
looking after the health of the skin and maintaining a balanced diet, with sufficient intake of protein, vitamins and
fatty acids.2 The ability of skin to regenerate once damaged is reduced in older people. Immune function also
declines with age, therefore older people have an increased susceptibility to infection, e.g. in wounds caused by scratching.
 For further information, see: “Skin and the biology of ageing”.
For further information, see: “Skin and the biology of ageing”.
Identify dry skin early
Dry skin (xerosis) is a common dermatological feature in older people.3 This is caused by water loss from
the stratum corneum, and as a consequence the skin is more likely to crack, which can result in itching, bleeding and
asteatotic dermatitis.4 Troublesome dry skin is often under-reported and patients may wait many years before
asking a health professional for advice.4
All older patients should have their skin periodically assessed for signs of excessive dryness. Possible causes of dry
skin include:3
- Cold, dry air during winter
- Direct skin exposure to fan heaters
- Excessive immersion in water
- Use of alkaline soaps and detergents with ingredients that damage the skin barrier
- Chronic sun damage
- Papulosquamous skin conditions, e.g. eczema, psoriasis
- Chronic illnesses, e.g. hypothyroidism, chronic kidney disease (CKD)
- Genetic inheritance, e.g. ichythyosis vulgaris, characterised by persistently dry, thickened, rough skin
- Systemic disease, e.g. lymphoma, malnutrition, resulting in acquired ichythyosis
Excessively dry skin is often scaly or cracked. This is frequently seen on the legs in older people, where skin may
have the appearance of cracked porcelain, referred to as eczema craquelé (Figure 1).
Removing triggers for dry skin may reduce the need for treatment
Take a history from patients with dry skin to identify any obvious causes. Advise the patient to avoid soap and other
alkaline cleansers and any topical products containing alcohol or fragrance. Wearing loose clothing and avoiding woollen
fabrics may reduce skin irritation.
Reducing the time spent in the shower or bath, and avoiding very hot water decreases lipid loss from the skin and may
limit skin irritation.
Emollients are used to treat dry skin
Patients with dry skin should apply emollients at least twice daily, ideally within minutes of washing the skin, and
at other times if necessary.1 These are available in a range of different formulations, including creams,
ointments and lotions (Table 1).1
Emollients can hydrate the skin by two mechanisms:
- Drawing water from the dermis to epidermis due to the presence of humectants, e.g. urea or glycerol
- Preventing water from escaping with an oily layer, e.g. ointments
Emollients generally have a neutral or low pH which helps to maintain the barrier function of skin,3 and
are also reported to have anti-inflammatory properties.4
The choice of emollient is based on how dry the patient’s skin is and their preference; patients are most likely to
be adherent to a treatment if they are using a preparation they are comfortable with. A process of trial-and-error may
be required, however, an emollient with a 10% urea content is a reasonable starting point (Table 1).3 Some
patients may report a mild stinging or itchy rash associated with the use of urea.5 Emollients containing
urea should not be used on areas of dermatitis or broken skin, on any area that is infected or where there is severe or
widespread erythema.
Emollient products may need to be changed depending on the season, the patient’s lifestyle and disease severity.4 Patients
who experience drier skin during winter may benefit from temporarily using an emollient with a thicker lipid film, e.g.
an occlusive ointment. Due to their high oil content, ointments can be messy and may stain clothes, and therefore are
best applied at night. Greasy emollients may lead to infected or irritant folliculitis. If this occurs, the patient should
be switched to a less greasy product. Antibiotics may also be required if infection is present, e.g. flucloxacillin if
Staphylococcus aureus is suspected.
A patient using a leave-on emollient can also be prescribed a wash-off emollient, e.g. aqueous cream BP or emulsifying
ointment (see: “Aqueous cream or emulsifying ointment should not be used as leave-on products”).4
An evidence-based approach to skin care is important and it should not be assumed that all naturally occurring oils
are beneficial to human skin. For example, olive oil has historically been recommended as an emollient for infants with
dry skin. However, this practice has been shown in adults to be detrimental to skin hydration and to adversely affect
skin integrity.6
Recommend non-soap based bath products
Soaps that contain lanolin and glycerine, or moisturising soaps, are less likely to cause skin flaking than standard
products. However, it is best that patients with dermatitis avoid all soaps. In addition, the use of lanolin may cause
allergic contact dermatitis in some patients.7 Non-soap based bath and shower products are available on prescription
(Table 1) and over-the-counter (OTC). Emollient bath additives, e.g. oatmeal colloidal (unsubsidised),
can be added to bath water and skin hydration improved by soaking for 10 – 20 minutes.8 Advise patients that
bath and shower products, especially oils, can make surfaces slippery and care needs to be taken. Non-slip mats and/or
the installation of a rail in the shower box or next to the bath, may help reduce the risk of falling.
Emollients should be prescribed in sufficient quantity to have an optimal effect, and the amount will
vary depending on which areas of the body are affected (Table 2).4 If the patient spends
a significant portion of their time away from home, an additional smaller-quantity pack will allow them to use the product
during the day.
Fire hazard with paraffin-based emollients
Emulsifying ointment, petroleum jelly, or 50% liquid paraffin and 50% white soft paraffin, can be ignited when present
on clothes or dressings. This risk is greatest when large areas of the body are being treated, or when dressing or bandages
become soaked in the ointment. Patients should keep away from open fires and flames, e.g. candles, and be advised not
to smoke when using these products.
Table 1: Emollient selection aide for subsidised products used for the treatment of dry skin
in older patients*8,9
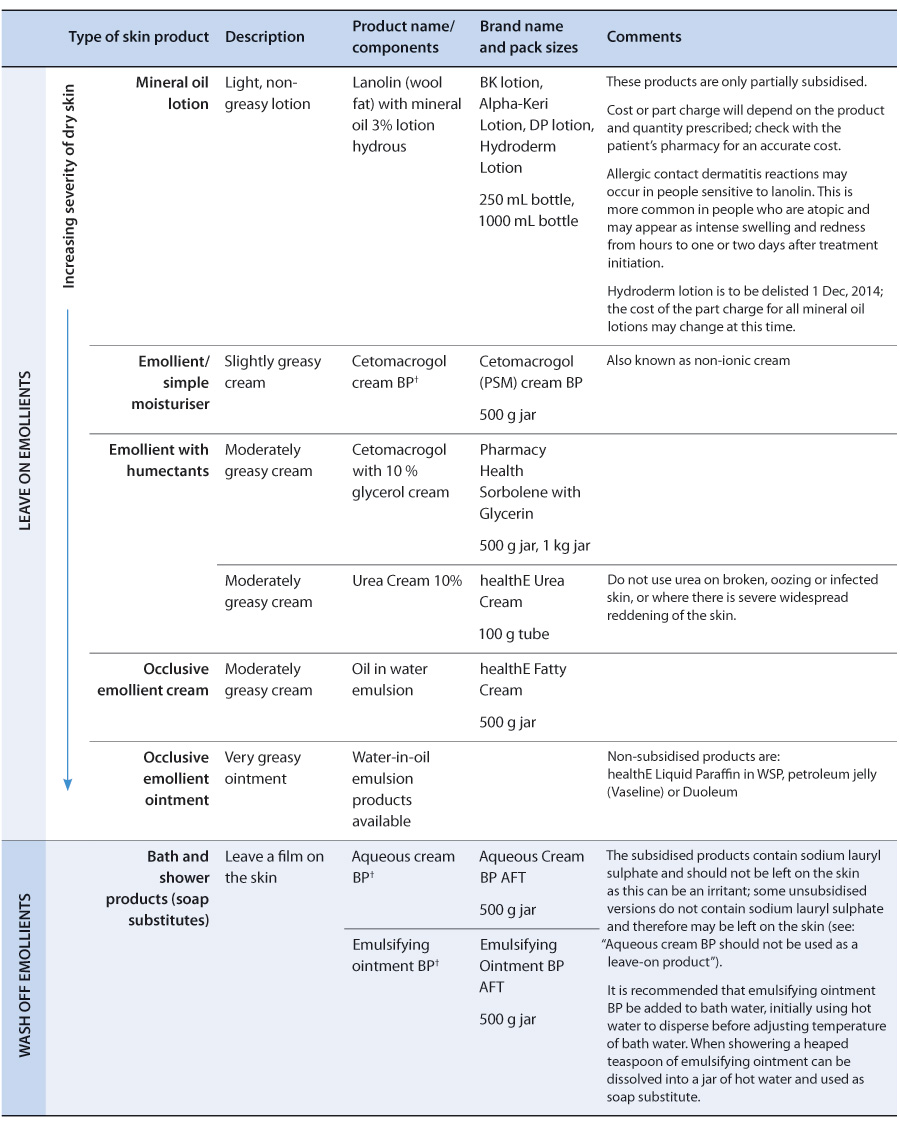
†Some products contain ‘BP’ in their name. This stands for British Pharmacopoeia, which is a detailed
collection of standard specifications and formulae for compounded medicinal and pharmaceutical products.
*NOTE: the quantity of supply by the dispensing pharmacy will be the full three-month quantity prescribed,
unless the prescriber endorses each skin product on the prescription clearly with the words “Trial Period” or “Trial”,
and specifies the maximum quantity to be dispensed at any one time; liaison with the patient’s pharmacy is helpful.
Table 2: Recommended quantities of topical emollients to be prescribed for an adult, with
twice daily application for one week to specific body areas8
| Body area |
Creams and ointments |
Lotions |
| Face |
15 – 30 g |
100 mL |
| Both hands |
25 – 50 g |
200 mL |
| Scalp |
50 – 100 g |
200 mL |
| Both arms or both legs |
100 – 200 g |
200 mL |
| Trunk |
400 g |
500 mL |
| Groin and genitalia |
15 – 25 g |
100 mL |
Emollients are best applied by dotting the product on the skin then spreading it using a downward stroking
motion.1 It is not necessary to spread the product until it is all absorbed. A clean spatula should be used
to extract the emollient from the tub so pathogens are less likely to be introduced into the preparation. Alternatively,
the emollient can be decanted into a clean, empty pump dispenser. In patients who are older, obese or have arthritis the
assistance of a partner or carer may be necessary when applying the emollient.
Emollients can be used in conjunction with other topical treatments. If an emollient and a topical
corticosteroid are prescribed at the same time, e.g. for a patient with atopic dermatitis, the emollient should be prescribed
and applied at ten times the quantity of the steroid.4 The use of emollients in conjunction with topical corticosteroids
can reduce the need for corticosteroid use without a loss of treatment efficacy (by improving skin health).4 Ideally
one product, i.e. emollient or corticosteroid, should be applied at least 30 minutes before the other; the order of application
is not important.4
Cosmetic products containing fragrance and colour have no therapeutic value and should be avoided as these can alter
skin pH, irritate, cause contact allergy and worsen dry skin
Aqueous cream or emulsifying ointment should not be used as leave-on products
Aqueous cream BP first appeared in the British Pharmacopoeia in 1958 and its original formulation has been unchanged
since. It was intended for use as an emollient wash product,10 however, it has been frequently prescribed as a leave-on
emollient for patients with atopic dermatitis in New Zealand and in other countries.11 In 2009 it was reported that aqueous
cream BP accounted for approximately one-quarter of all topical emollients prescribed in the United Kingdom.11 A growing
body of evidence now suggests that for some patients, aqueous cream BP should not be used as a leave on emollient and
that doing so can cause significant damage to the skin barrier.
Aqueous cream BP is formulated using emulsifying ointment. Emulsifying ointment contains emulsifying wax, which in turn
contains sodium lauryl sulphate (1% w/v in aqueous cream). Sodium lauryl sulphate is a surfactant used in a wide range
of products due to its solubilising, wetting, suspension stabilising, emulsifying and frothing properties.12 Sodium lauryl
sulphate is known to increase the permeability of the skin barrier and is often used as a model irritant in experiments.12
Concerns about the possible adverse effects of aqueous cream BP were first noted in studies assessing children in which
over half of patients reported a cutaneous reaction described as a “stinging” sensation when the product was applied.12
Several small studies in adults have reinforced these concerns and led to a number of dermatologists recommending that
aqueous cream BP should not be used as a leave-on emollient in patients with atopic dermatitis.11
In one study of six volunteers, with no history of skin disease, aqueous cream BP was applied to the forearm, twice
daily for four weeks.12 A significant reduction in skin thickness and an overall increase in transepidermal water loss
was reported.12 Another study involved 13 volunteers with a previous history of atopic dermatitis, but without current
symptoms.11 Again, aqueous cream BP was applied to the forearm, twice daily, for four weeks. Aqueous cream BP was described
as causing severe damage to the skin barrier.11 The minimum recommended doses were used in these studies and therefore
more frequent use of aqueous cream BP, or use of the product by patients with more severe forms of dermatitis, may cause
more extensive skin damage.
Aqueous cream and emulsifying ointment are therefore not recommended as leave-on emollients, but are still suitable
as soap substitutes because in this situation, the product is washed off and is only in contact with the skin for a short
time.
Managing dry, itchy skin in older patients
In older people, dry skin is frequently associated with pruritus due to the reduced lipid content in the skin, the decreased
production of sweat and sebum, and diminished vascular perfusion.3 Dry skin and pruritus commonly occur without a visible
inflammatory rash and are sometimes referred to as “winter itch” or “seventh age itch”. Scratching can lead to secondary
dermatitis with dry scaly plaques (lichen simplex).
The patient’s history is likely to contain clues to the source of their symptoms. Considerations for health professionals
when discussing dry and itchy skin with a patient include:3
- Are the patient’s symptoms general or localised? Generalised skin symptoms are more suggestive of a systemic cause.
Localised pruritus without a primary rash may be of neuropathic origin.
- Has the patient noticed a rash? Itchy rashes are most often due to eczema, scabies, urticaria, and insect bites,
however, there are many more possible diagnoses.
- Is there any time of day when the symptoms are worse? For example, night time is often associated with worsening
symptoms in patients with scabies.
- Have any of the patient’s family members or contacts developed similar symptoms that suggest an infectious condition,
e.g. scabies.
- Is the patient aware of anything that can improve their symptoms, e.g. a specific treatment?
- Did the onset of the patient’s symptoms coincide with the initiation of any medicines?
- Could the patient’s symptoms be related to gardening or another outdoor activity? Plant dermatitis (phytodermatitis)
can occur after contact with plants such as the Rhus tree (Toxicodendron succedaneum), Primrose (Primula
obconia) or Chrysanthemum.13
A diagnosis of atopic dermatitis (eczema) generally occurs early in life and is more likely in patients with another
atopic condition, i.e. asthma or allergic rhinitis. Atopic dermatitis is reported to affect approximately 3% of the adult
population and may persist into older age.14 In adults, the dermatitis is often persistent and localised to the hands,
eyelids, flexures and nipples. The skin is often more dry and lichenified than seen in children with eczema.15 Recurrent
staphylococcal infections may also occur.15 Irritant contact dermatitis due to exposure to water or detergents is more
likely to occur in patients with atopic dermatitis.15
 For further information see: “Managing eczema”, BPJ 23 (Sep, 2009).
For further information see: “Managing eczema”, BPJ 23 (Sep, 2009).
Psoriasis can start later in life and is reported to affect approximately 2 – 4% of the population.16 The condition
is often mild and may or may not be itchy.16 Approximately 5% of these patients will develop psoriatic arthritis involving
single or multiple joints, which can be debilitating.16 Psoriasis appears as red, scaly plaques with well defined edges
and silvery-white scale, and is often symmetrical.16 Scale may be less obvious if the patient has been using emollients
regularly.16
 For further information see:
“The treatment of psoriasis in primary care”, BPJ 23 (Sep, 2009).
For further information see:
“The treatment of psoriasis in primary care”, BPJ 23 (Sep, 2009).
Consider other causes of dry, itchy skin
Other skin disorders frequently encountered in older patients that cause dry, itchy skin include:3
- Adverse reactions to medicines, e.g. antibiotics
- Localised contact irritant dermatitis, e.g. vulval dermatitis due to urinary incontinence (see:”Vulvovaginal
health in post-menopausal women”)
- Localised contact allergic dermatitis (occurs less frequently ), e.g. hair dye dermatitis
- Venous eczema associated with leg oedema and lipodermatosclerosis
- Localised inflammatory skin disorders, e.g. lichen sclerosus ( For further information, see:
www.dermnetnz.org/immune/lichen-sclerosus.html)
- Grover disease – mainly affects older males and may appear as itchy crusted papules on the trunk. It is more common
in winter and although frequently itchy there may be no other symptoms ( For further information, see:
www.dermnetnz.org/scaly/grovers.html).
- Bacterial infections, e.g. cellulitis
- Intertrigo due to seborrhoeic dermatitis
- Fungal infections, e.g. Candida albicans
When examining the patient’s skin, pay particular attention to their feet, especially in older patients with diabetes.
Examine the soles of the feet for scale and between the toes for maceration and fissuring suggestive of tinea pedis. Nail
changes can help in the diagnosis of fungal infections and psoriasis. Cellulitis is painful and should be suspected in
patients with erythema, swelling and skin that is hot to the touch. Referral and/or skin biopsy should be considered for
patients with skin lesions that cannot be classified on examination. Further investigations may be appropriate in patients
with itchy skin and additional features consistent with an underlying condition. For example, HbA1c testing should be
considered in patients with pruritus, polyuria and polydipsia, or liver function testing in a patient with pruritus and
other symptoms of liver dysfunction.
A general approach to pruritus
Scratching can exacerbate pruritus. It can also result in secondary lesions that may mask the primary cause of the patient’s
pruritus. Excoriations or bruising may be present on areas such as the back if the patient has used a hair brush or doorway
to alleviate their itch, therefore a thorough inspection of the skin is necessary.
Resisting scratching can be as stressful as pruritus itself. Some patients may find pressing on the affected area, rather
than scratching, provides relief. The use of a damp cloth, reduction of night-time heating and tepid showers may be beneficial.
Suggest patting skin dry rather than vigorous towel-drying following washing to reduce the risk of further skin damage.
Some patients may be able to tolerate wearing gloves or mittens while they sleep to prevent further skin damage.
Topical products may provide limited relief of pruritus
Over-the-counter topical products containing menthol or phenol cause nerve fibres to transmit a cold, itch-relieving
sensation when they evaporate.3 Menthol is safe and non-toxic when applied to unbroken skin; emollient products containing
approximately 1% menthol are suitable for older patients, although care should be taken to avoid mucus membranes and genitals.3
There are no subsidised proprietary products that contain menthol, but menthol in other bases, e.g. aqueous cream, 10%
urea cream, wool fat with mineral oil, 1% hydrocortisone with wool fat and mineral oil lotion, or glycerol, paraffin and
cetyl alcohol lotion, can be prepared by pharmacists if prescribed.
Tar (2.3%) with triethanolamine lauryl sulfate (6%) (Pinetarsol solution) is indicated and fully-subsidised for the
treatment of dry, itchy, inflamed or flaky skin conditions, e.g. eczema, dermatitis and psoriasis. Bathing for five to
ten minutes in a warm to tepid bath with 15 – 30 mL of Pinetarsol added may provide relief for the patient.8
Capsaicin cream (0.075%) can desensitise sensory nerve fibres and exert an antipuritic effect.3 This treatment may be
beneficial for neuropathic, systemic and dermatological pruritus, although pain, burning and stinging at the site of application
may mean that treatment is not tolerated by the patient.3 Capsaicin cream is only subsidised for patients with post-herpetic
neuralgia, diabetic neuropathy or osteoarthritis (Special Authority criteria apply). It can be purchased OTC.
Local anaesthetics and topical antihistamines are only slightly effective in treating pruritus and can occasionally
cause sensitisation.8 Calamine aqueous cream (containing zinc oxide) and calamine lotion (containing phenol 0.5% and zinc
oxide) are fully subsidised, but can increase skin dryness and are therefore not recommended.8
Managing skin tears due to dry, itchy skin
Older skin is more fragile and therefore more likely to tear when subjected to trauma – even with minor injury such
as scratching. Unsteadiness, impaired vision and immobility mean that older people are more likely to walk into objects,
and sensory impairment may mean that they are less likely to notice that they have experienced an injury.
Skin tears in older people often occur on the upper and lower limbs and on the back of the hands.17 Where
a patient requires assisted lifting or bathing by a carer the risk of skin tears in other areas may be increased. Older
people and their carers can reduce the risk of skin tears by keeping their nails well trimmed, not wearing jewellery and
placing padding around corners of objects, e.g. beds. Gardening and interacting with pets are also common causes of skin
tears in older people. Encourage older patients to wear gloves and protective clothing when working outside and to keep
pets claws trimmed and discourage them from jumping up where possible. Advise patients to report and seek treatment for
any significant skin tears as early treatment reduces the likelihood of complications developing.
Assessing skin tears
When assessing a skin tear it is important to note any underlying conditions that may influence the patient’s rate of
healing, e.g. diabetes or venous insufficiency. The patient’s tetanus vaccination status should also be considered.
A baseline assessment of the wound allows the healing process to be monitored. It is recommended to include the:17
- Date that the injury occurred and its anatomical location
- Length, width, depth and presence of skin flap
- Wound bed characteristics and percentage of viable tissue: eschar (scab) is usually seen as hard and black, and slough
(dead tissue) is generally cream or yellow in colour
- Extent of any flap necrosis
- Type and quantity of exudate
- Presence of bleeding or haematoma
- Surrounding skin integrity
- Presence and severity of any pain
- Signs of infection
 Best practice Tip: A photographic record with a ruler to demonstrate wound size
can be useful for monitoring wounds.
Best practice Tip: A photographic record with a ruler to demonstrate wound size
can be useful for monitoring wounds.
Treating skin tears
The goals of skin tear management are to:17
- Preserve the skin flap and protect the patient’s surrounding tissue
- Reapproximate the wound margins without overly stretching the skin
- Reduce the risk of infection
Dressings that encourage a moist wound healing environment should be selected.17
Clean the wound with either warm saline or water to flush the wound and remove any debris or residual
haematoma.17 The surrounding skin should be patted dry, taking care not to cause further injury.
Any viable skin flap should be gently replaced using a dampened cotton tip, gloved finger, careful
use of tweezers or a silicone strip.17 A moistened non-woven swab can be applied to the flap for five to ten
minutes to soften it and make it easier to align.17
A barrier cream, e.g. dimeticone 5%, can be applied as appropriate to prevent the surrounding skin
breaking down due to periwound moisture.17
There is no single dressing that is recommended for all skin tears. The choice of dressing will be
influenced by the location and type of tear and clinical experience. An optimal dressing for a skin tear injury will:17
- Provide an anti-shear barrier
- Optimise healing by providing a moist environment with bacterial exclusion and optimal pH
- Be flexible and moldable to contours
- Attach securely to the patient without causing ischaemia
- Be durable
- Not cause trauma on removal
- Allow for movement
- Be cosmetically acceptable
If an adhesive wound-closure strip is considered, e.g. steri-strips, then sufficient space should be left between each
strip to allow drainage and swelling to occur.17 Care should be taken to prevent tension over flexure sites
which can cause ischaemia.17 Tissue glue can be used to hold skin in contact with skin, but should not be
used under the skin flap. Calcium alginate, foam or fibre dressings may help with exudate absorption.17 Sutures
and staples are generally not recommended in patients with fragile skin, however, these may be necessary when treating
deep or full-thickness lacerations.17
Dressings should be left in place for several days to allow the skin flap to adhere.17 When using an opaque
dressing an arrow indicating the direction of removal may be useful.
If the patient is at increased risk of infection, e.g. the patient has diabetes or has a history of skin infections,
then empiric oral antibiotics may be considered, e.g. flucloxacillin (erythromycin if penicillin-allergic). Topical antibiotics
or antiseptics should not be routinely used for wound management.
Review and reassess the wound at each dressing change. The dressing should be gently worked away from
the attached skin flap. Soaking dressings in saline or using silicon-based adhesive removers can reduce trauma to the
healing wound.17 Cleaning should not disrupt the skin flap. The wound bed should be assessed for changes.
If the skin or flap is pale and darkened, it should be re-examined after 24 – 48 hours.17 If the skin flap
is not viable then debridement is usually necessary.17
Increased pain may indicate that the patient’s wound has become infected. However, routine microbiological assessment
of wounds is not necessary as swabbing a wound that is not infected can result in the identification of organisms colonising
the wound rather than those causing an infection. Consider swabbing a wound if there are clinical signs that the wound
is infected and it is deteriorating, increasing in size or failing to heal.18 In patients with diabetes, or
another condition associated with reduced perfusion and immune function, a lower threshold for swabbing the wound may
be appropriate as the classical clinical signs of infection may not be present.19
Oedema may cause levels of exudate to be increased. Patients with skin tears on their legs may need to elevate the wound
to reduce the likelihood of oedema complicating wound healing. However, regular movement of the leg in patients who are
able to exercise should also be encouraged to improve circulation. In patients without peripheral artery disease and diabetes
mellitus, graduated compression therapy should be considered early in the treatment process in order to prevent the development
of a chronic leg ulcer.
 For further information see: “Microbiological
assessment of infected wounds: when to take a swab and how to interpret the results”, BT (Jun, 2013).
For further information see: “Microbiological
assessment of infected wounds: when to take a swab and how to interpret the results”, BT (Jun, 2013).
Skin and the biology of ageing
The process of ageing involves genetics, physiological processes and environmental factors. As ageing progresses, body
function is reduced at all levels, from cells to organs, including the skin.20
The outer most layer of the epidermis, the stratum corneum, forms the skin barrier that restricts water loss and prevents
entry of pathogens, irritants and allergens. Healthy skin contains densely packed corneocytes, which are flattened dead
cells without a nucleus or organelles. These cells are embedded in extracellular lipids, such as ceramides.4 Corneocytes
contain natural moisturising factors, including urea, which attract and hold water inside the cell.4, 5 In healthy skin,
transepidermal water loss is minimised by the secretion of sebum onto the skin surface from the sebaceous glands.2
Over a life-time the epidermis and dermis becomes thinner and flatter; this is associated with a reduction in the number
of cutaneous blood vessels and nerve endings, and a reduction in connective tissue containing collagen, elastin and ground
substance (Figure 3).1 Cumulative exposure to ultraviolet (UV) radiation damages DNA and causes extracellular proteins
to degrade. The skin’s mechanical strength declines and there is a decreased ability to retain water, control temperature
and sense the environment.1 Production of sebum also declines making corneocytes more susceptible to desiccation and shrinkage.1
Skin accumulates advanced glycation end products (AGEs) over time, which are the product of non-enzymatic reactions
between reducing sugars, e.g. glucose, and proteins, lipids or nucleic acids.20 AGEs are reactive compounds that cause
proteins, such as collagen, to crosslink, resulting in a loss of skin elasticity.20 AGEs are of dietary origin and endogenously
produced. The rate of AGE formation is elevated in people with diabetes and they are also increased by smoking and food
preparation methods, e.g. fried food generally has a far higher AGE content than steamed or boiled food.20 Exposure to
UV radiation may accelerate the formation of AGEs.20 Various receptors interact with AGEs that are involved in inflammation,
immune responses, cell proliferation and gene expression.20 Accumulation of AGEs is associated with angiopathy and solar
elastosis (a thickening and yellowing of the skin due to sun damage).