The importance of calculating cardiovascular risk
Cardiovascular risk management is central to general practice. The current approach to this involves calculating the
patient’s cardiovascular risk, helping patients to understand what their risk means, and empowering patients, especially
those with high cardiovascular risk, to make changes to reduce their risk. During these discussions if information is
not delivered in a way that the patient understands then their ability to make informed decisions that are beneficial
to their health is likely to be limited.
Calculating cardiovascular risk in New Zealand
In New Zealand, an equation based on Framingham data is used to calculate combined five-year cardiovascular risk. While
this equation is not a perfect predictor of outcomes, it is very good at identifying those patients who are at a higher
risk of experiencing a cardiovascular event.1 The five-year cardiovascular risk combines key factors into
an overall risk. This is intended to assist patient understanding, and allows clinicians to have an overview of the patient’s
health, rather than focusing on individual risk factors. The goal of the health professional is to help the patient to
lower their overall cardiovascular risk and to place the patient’s cardiovascular risk in the context of other co-morbidities,
e.g. chronic obstructive pulmonary disease (COPD).
Many General Practitioners have validated electronic cardiovascular calculators embedded into their decision support
tools, e.g. bestpractice or Predict, which enable rapid calculation of cardiovascular risk.* Furthermore, guidelines are
relatively clear in the management of individual cardiovascular risk factors. However, increasing a patients understanding
of cardiovascular risk and empowering them to use this information to make decisions is arguably the greatest challenge
in the management of cardiovascular health. This is because many people base their assessment of risk on emotions, that
will influence their decisions rather than data.2 The task of communicating risk is further complicated because
as many as one in five well-educated people incorrectly interpret basic statistical information.3
* Validated electronic cardiovascular calculators are not available in all regions. The New Zealand Cardiovascular
Risk Charts can be used by clinicians in place of electronic calculators. These are available online at
www.health.govt.nz/system/files/documents/publications/090311_cvd_poster_final.pdf
or in the New Zealand Primary Care Handbook 2012.
Shared decision-making is central to risk management
Discussions with patients about treatment options for cardiovascular disease are best managed with a shared decision-making
approach. This involves the clinician using their knowledge and skills to enable the patient to arrive at a decision which
best fits the patient’s values and priorities. This process takes many factors into account, including:
- The patient’s age, ethnicity, co-morbidities and frailty
- The benefits versus harms of any interventions
- The patient’s family/whānau
- Current evidence-based guidelines
- The patient’s internal concerns, beliefs, expectations and values
- The health professional’s clinical experience
- The patient’s occupation, hobbies and commitments
- The patient’s socioeconomic and occupational status which may limit their ability to meet the cost of appointments,
travel to clinics or take time-off work to attend consultations
- The patient’s willingness to consider change at this stage
Patients are more likely to take responsibility for managing their own health if they are actively engaged in treatment
decisions and their family/whānau are encouraged to be involved.4 Being actively involved in self-management
means patients are also more likely to be satisfied with their treatment.4 For shared decision-making to be
meaningful patients need to understand the reasons why health professionals are making recommendations. Therefore discussions
with patients about cardiovascular risk are crucial. These become even more important when the balance between the advantages
and harms of a treatment are finely weighted, e.g. treating patients with statins when their cardiovascular risk is moderate;
a strong patient preference for longevity of life or avoidance of adverse effects may be the difference between treating,
or not treating.
The morbidity and mortality of cardiovascular disease
Cardiovascular events are the leading cause of mortality in New Zealand, accounting for almost one-third of deaths
annually; every 90 minutes one New Zealander dies of coronary artery disease.11 Stroke is the leading cause
of disability among adult New Zealanders; seven out of ten patients that survive a stroke will be disabled long-term.11
Discussing cardiovascular risk with patients
Following a cardiovascular risk assessment all patients should be given the opportunity to discuss their result, regardless
of their level of cardiovascular risk.5 Some patients may appreciate being offered the opportunity to do this
with whānau/family being present. The outcomes of this discussion will be influenced by the ability of the health professional
to deliver information so that it is understandable to the patient. Health professionals who do this well will naturally
adjust the complexity of the discussion and use different tools to explain concepts, as appropriate to the individual
patient.
There are no clear recommendations about how risk should be communicated to patients, because each individual will interpret
information differently and each representation of risk carries its own connotations and biases, e.g. absolute versus
relative risk.6 In psychological studies, how risk-related information is presented to patients has been repeatedly
shown to influence how risk is perceived, and to a lesser extent this effect has also been demonstrated in clinical encounters.7 Risk
perception is vitally important because it, not clinical assessments, forms the basis for patient decision-making.8
Health professionals and patients may think differently about risk
Health professionals deal with the concept of cardiovascular risk daily. However, explaining this concept to people
who are not familiar with it can be challenging because:
- It is an abstract concept that does not apply to the present, but rather to an unspecified point in time at some
stage in the next five years
- Even those at high five-year risk of a cardiovascular event, e.g. 25%, are still unlikely to experience an event
in the next five years, i.e. there is a 75% chance that they will not experience an event
Cardiovascular tools should therefore be used as a prompt for discussions about cardiovascular risk, with clinical expertise
helping individual patients understand their risk.
First define what you mean by cardiovascular event
In New Zealand cardiovascular events are defined as a diagnosis of: myocardial infarction, new angina, ischaemic stroke,
transient ischaemic attack (TIA), peripheral vascular disease, congestive heart disease or cardiovascular-related death.9 Depending
on the patient’s experience and level of health literacy, terms such as stroke, heart attack and cardiovascular disease
can mean different things.10 For example, if a patient has a relative who has had only a minor TIA then they
may not be overly concerned about their likelihood of experiencing a similar event. Presenting a balanced and accurate
picture of the morbidity and mortality associated with cardiovascular events will help some patients to make informed
decisions (see: “The morbidity and mortality of cardiovascular disease”).
Distinguishing between modifiable and non-modifiable risk factors
For patients who are at increased risk of cardiovascular disease due to non-modifiable factors, e.g. age or an early
family history of ischaemic heart disease, it is important to acknowledge that these are outside the control of the patient
and yet may contribute substantially to their risk.
Conversely, it is important that patients understand there are a number of modifiable risk factors that they can alter
to improve their health. A series of interviews with 25 Māori patients in Northland with ischaemic heart disease, found
that Māori patients were often aware of family histories of cardiovascular disease and that there was a genetic component
to cardiovascular risk.12 However, it was also found that these patients had less of an understanding of the
impact of lifestyle factors on cardiovascular risk.12 This small study shows the need to explore patients’
awareness of the factors that contribute to their cardiovascular risk.
Present risk as statements rather than probabilities
Presenting risks as frequency statements, rather than single event probabilities, has been shown to reduce the likelihood
of information being misunderstood.13 For example, if the patient has a five-year cardiovascular risk of 15%,
then it is more useful to tell them that 15 out of 100 patients like them will experience a cardiovascular event over
the next five years. Doing this removes the potential for confusion over reference classes.13 For example,
some patients may think that a 15% risk of a cardiovascular event refers to a 15% heart attack, which they may perceive
as a mild or small heart attack, while other patients may think there is a 15% chance they will have a heart attack every
day, and become highly anxious.
Negotiating risk reduction with patients
The overarching principle of cardiovascular risk management is that those at higher risk have the greatest potential
to gain from interventions. However, many patients struggle with this principle because some of the factors that contribute
to cardiovascular mortality are insidious and asymptomatic, e.g. hypertension. From the patient’s perspective it may seem
logical to take a medicine to treat a symptom such as pain, however, they may be significantly more reluctant to take
a pill everyday for dyslipidaemia if “I am feeling fine.” Converting patients from a “how I feel” approach, to a more
prognostic “how long will I live” view of their own health is frequently reported to be one of the greatest challenges
in working alongside patients with long-term conditions.14 This task is made more difficult by the fact that
many interventions also involve the risk of symptomatic adverse effects, e.g. myalgia associated with statin use. However,
for a trusting relationship to continue to evolve between patient and clinician the possibility of adverse effects of
treatment should always be mentioned when discussing the pros and cons of treatment options. Explaining to patients that
they are unlikely to feel an elevated blood pressure unless it is extreme is a simple way to begin conversations about
risk factors that may be hidden to the patient. During consultations avoid descriptive terms, e.g. high-risk, which may
have different meanings for different people and provide numeric examples with a consistent denominator where possible.2
Present a variety of treatment options to patients
When “making recommendations” it is easy for health professionals to narrowly suggest one course of action as outlined
in a guideline, rather than helping patients see all of the options that are available. A wider perspective gives patients
a number of options to consider, and for some, a sense of empowerment. When discussing the options available, the status
quo, i.e. no change, is also a possibility. This “options approach” fits well with the process of informed consent, where
patients are entitled to the risks and benefits of all reasonable options of care.
Patients may need time to consider their options
Many patients will be at the contemplative stage of change, and need time to think before deciding whether to begin
a particular cardiovascular risk reduction treatment. This may involve discussion with family/whānau, or require more
than one consultation with a health professional.
Remember that, for many patients, beginning long-term treatment for a chronic condition is a negative milestone in their
life. Furthermore, the daily process of “taking pills” reminds them that they have a long-term medical condition. Denial
and avoidance of “pill taking” can therefore be understood as natural human reactions in this context. Encouraging patients
to think of pills as a positive step, helping them to live long enough to see grandchildren marry (or another goal that
is important to them), may help to change this mindset.
Consider individual risk factors when deciding on the order of interventions
It is easier for a patient to achieve a clinically significant reduction in a risk factor that is very high than it
is for one that is mildly abnormal.5 Patients need to understand this when choosing between treatment options.
For example, smoking cessation is likely to be of increased importance to a patient with elevated risk who has respiratory
symptoms due to COPD. Lifestyle interventions can be presented as an alternative to medicines, e.g. “if you managed to
lose a few kilograms by September I don’t think there would be a need for you to start taking pills for hypertension.”
It will also often be necessary to treat multiple risk factors simultaneously.5 Regardless of what level of
cardiovascular risk a patient has they should be encouraged to exercise regularly, for example 30 minutes on most days.
 Best Practice Tip: Visit our Facebook page (www.facebook.com/bpacnz)
to comment on an excellent nine minute summary on the multiple benefits of exercise (also appropriate for patients to
view): www.youtube.com/watch?v=aUaInS6HIGo
Best Practice Tip: Visit our Facebook page (www.facebook.com/bpacnz)
to comment on an excellent nine minute summary on the multiple benefits of exercise (also appropriate for patients to
view): www.youtube.com/watch?v=aUaInS6HIGo

The “Your Heart Forecast” tool
In 2008 the “Your Heart Forecast” tool was developed to support cardiovascular risk communication and this tool has
now largely replaced the 2003 cardiovascular risk charts.5 The “Your Heart Forecast” tool is designed to
help health professionals explain to patients what their cardiovascular risk means. It provides a visual story for patients
in four stages:19
- First, the patient is provided with their current cardiovascular risk, i.e. you are here
- The patient’s cardiovascular risk is then compared to a peer with ideal modifiable risk factor control
- The patient is then shown what will happen if they continue without making any changes in their life, i.e. their
heart forecast
- Finally, the patient is shown what would happen to their future risk if they made changes to their lifestyle
There is currently no patient outcome data available to assess the effectiveness of “Your Heart Forecast”, although
a questionnaire of 47 health professionals showed that the tool improved clinicians understanding of cardiovascular risk
and increased their confidence in explaining cardiovascular risk to patients.19
 The “Your Heart Forecast” online tool is available within New Zealand from:
www.heartfoundation.org.nz
The “Your Heart Forecast” online tool is available within New Zealand from:
www.heartfoundation.org.nz
Graphical presentation improves understanding of risk
When presented with information about risk and probabilities people often pay more attention to the number of times
an event happens (the numerator) and less attention to the number of opportunities it had to happen (the denominator).15 This
effect is referred to as denominator neglect.15 A graphical representation is one way to overcome denominator
neglect. A large systematic review of multiple studies found that the use of graphical presentations of information relating
to health risks resulted in increased patient understanding and satisfaction.16
It is well established that graphical tools are more effective at conveying the benefits of cardiovascular interventions.17 In
a study of 100 patients in Auckland with a history of cardiovascular disease presented with information about a hypothetical
medicine, the majority of patients who expressed a preference for how information was presented, preferred to have it
displayed graphically.18 Relative risk was the next most preferred method of presentation, although presenting
information in this form may be considered coercive.18 Interestingly, stating the number needed to treat (NNT)
was the least preferred method of presentation. This suggests that while NNT may be a useful method of expression for
clinicians, it may be less so for patients. NNT has also been found to decrease patient understanding of risk in other
studies.16
The New Zealand Heart Foundation has provided two graphical online tools, one for health professionals
(see: The “Your Heart Forecast” tool) and one for the general public. Both tools are designed
to communicate, rather than calculate, cardiovascular risk.* The “Know Your Numbers” tool is available to all people and
is intended for use without the support of a health professional. This tool does not include the physical effects of inactivity
in its calculation, although it does recommend exercising on most days for 30 minutes.
* When calculating a patient’s five-year cardiovascular risk it is important to use a validated decision-support
tool, or the New Zealand Cardiovascular Risk Charts.
 The “Know Your Numbers” tool is available from:
www.knowyournumbers.co.nz/
The “Know Your Numbers” tool is available from:
www.knowyournumbers.co.nz/
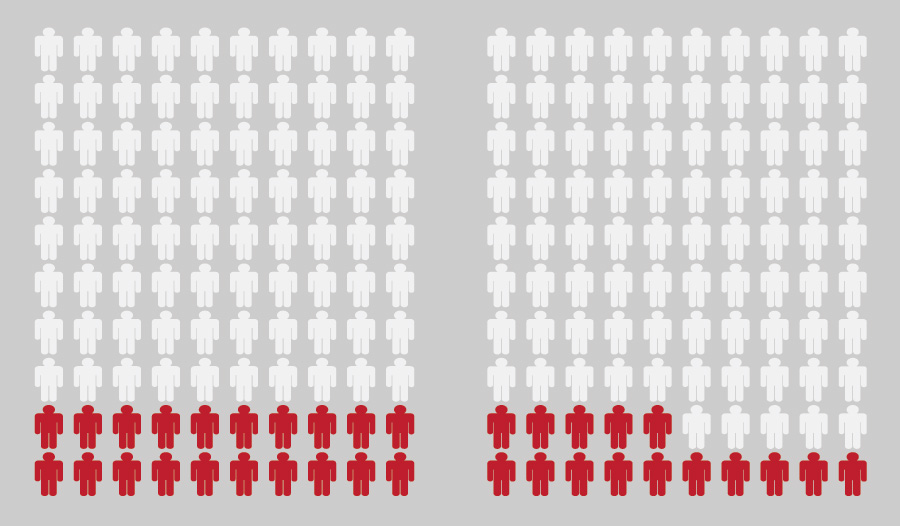
Figure 1: Graphic representation of a five-year cardiovascular risk of 20% and how the benefit of
a reduction of risk to 15% may be explained to a patient, adapted from Paling, 2003,2 available from
www.bmj.com/content/327/7417/745
Present absolute risk rather than relative risk
It has been shown that when patients are presented with information in the form of absolute risk they have an increased
understanding, but are less likely to take action to reduce their risk based on this information.16 Presenting
the benefits of a cardiovascular intervention in terms of relative risk reduction is often more motivating for patients,
but information presented solely in this manner can be easily misinterpreted,2 raising the issue of informed
consent.7, 13, 18 Increasingly, it is being recommended that risk reduction should be presented in absolute
terms, where possible.2, 20 An example of the way that information about absolute risk reduction could be
conveyed to a patient with a five-year cardiovascular risk of 20% who smokes would be: “If 100 people like you stopped
smoking, then every five years there would be at least five fewer CVD events among these people*.” However, clinical experience
and patient knowledge will ultimately decide the preferred method of presenting information about cardiovascular risk
to a patient. Checking with the patient that they have understood the intended meaning of the example is recommended whatever
method of explanation is chosen.
* Presuming quitting smoking would reduce the patient’s five-year cardiovascular risk by 5%
Framing affects perception
Framing refers to presenting logically equivalent information in different ways. This is an important concept when discussing
cardiovascular risk with patients because although survival and mortality figures for a condition or procedure will be
logically equivalent, e.g. 95% survival and 5% mortality, presenting only one or the other may result in markedly different
results when patients are asked to make a treatment decision. A meta-analysis of four studies found that respondents were
1.5 times more likely to chose surgery over other treatments when surgery efficacy was framed in positive terms (percent
survival), compared to negative framing (percent mortality).21 It is recommended that when treatment effects
are discussed with patients that health professionals express the information in more than one way, in order to present
a balanced view and facilitate patients making informed decisions.21 When discussing a possible lifestyle
intervention with a patient a balanced framing of the benefits would be, “If you give up smoking you could live an extra
five years and be much less likely to be disabled by a stroke like your uncle was.” The benefits versus risks of starting
a medicine could be presented by saying, “This medicine has a good chance of lowering your cholesterol, making you healthier,
and helping you live several years longer. A small number of people may also experience side effects like the muscle aches
we talked about before.”
Present benefits from short to long-term
The degree to which people are motivated by short and long-term benefits varies, and for some patients short-term gains
are more important than long-term benefits.14 This may partially explain why some patients persist with behaviour
that they know is doing them long-term harm. For example, the damage caused by smoking one cigarette may appear to be
negligible to the smoker, however, the pleasure of smoking one cigarette may be perceived as being substantial. By framing
the benefits of an intervention as both short-term and long-term, health professionals are likely to broaden the appeal
of the message to patients. For example, “if you quit smoking today”:
- Within two days food will smell and taste better
- Within three months your circulation will improve and that leg pain may go away
- After a year you will be able to afford to go on holiday
- Ten years from now you will be more likely to see your grandchildren
Set S.M.A.R.T targets
Cardiovascular risk reduction is dependent on patients understanding their risk and wanting to reduce it; a journey
that is unique for every patient. A suggested format for interventions to be presented in is:
- Specific – a specific target would be “I’m going to walk 30 minutes each day during lunch”, rather than: “I’m going
to exercise more”
- Measurable – this allows everyone to know if it has been achieved or not
- Achievable – unrealistic targets will cause patients to lose motivation. Modest targets, e.g. 500 g of weight loss
a week, are achievable and are more likely to increase patient confidence
- Recorded – patients are more likely to respond positively when they can measure their progress towards a future goal
- Time bound – goals are more likely to be achieved if they are bound to an agreed time-frame, e.g. by their daughter’s
wedding
Writing down goals and sharing them with others is likely to make them more concrete and may mean the patient has a
greater chance of achieving them.
Tailor interventions to the patient’s lifestyle
Cardiovascular interventions should aim to improve aspects of life that are important to the patient and their family/whānau.
Health professionals who have a longstanding and trusting relationship with patients and their family/whanau are likely
to understand some of the personal motivators for engaging patients with cardiovascular interventions. Asking patients
“what makes you smile?” is a good way to find out what they enjoy, and this answer can be used as a focus for interventions.
For example, a patient with children may be motivated to exercise by playing with their children in the park or coaching
one of their sport teams. This patient-centred model of care seeks to find common ground with clinical priorities and
the individual patient’s beliefs, goals and expectations (see: “Using the Te Whare Tapa Whā framework”).
In situations where there is not a longstanding relationship, or where patients are unwilling to consider lifestyle
change or treatment, i.e. they are at a pre-contemplative stage of change, the clinician still needs to respect the patient’s
decision-making autonomy, and work to maintain a trusting therapeutic relationship.
Check what the patient is taking away from the discussion
It is important not to overwhelm patients with information.10 An “Ask, tell, ask” approach, or a “chunk
and check” approach to consultations means that information is presented to patients at a controlled rate, with pauses
to confirm comprehension and agreement. A discussion about a cardiovascular risk factor can be started with a question
like, “Why do you think your blood pressure might be up?” Asking a patient what they will tell their family/whānau is
a simple way to check what message the patient is taking away at the end of the consultation. It also emphasises the benefit
of including the patient’s family in their management plan. Information that is written down and can be taken away or
accessed via the internet means the patient is able to review the material on their own or with family/whanāu to improve
understanding.
Before the end of the consultation, ask the patient to suggest a reasonable timeframe for the next consultation, e.g.
“When would you like to catch up again?”. Active management can be reserved for patients at higher risk, or who have difficulties
attending consultations. More frequent consultations that are focused on specific issues may be more beneficial than longer
appointments where multiple issues are addressed.
What matters to the patient – not what is the matter with the patient
Some patients may be reluctant to initiate a medicine, e.g. statins, once they have an increased understanding of the
benefits versus risks of treatment. Sometimes it is necessary for health professionals to accept that most human decisions
are made on an emotional basis.2 Patients usually know that aspects of their lifestyle are unhealthy. By assessing
patient readiness to change, the clinician may strengthen their relationship with the patient, so they are better placed
to enable them to make healthier decisions about their lives at a later date. As one experienced diabetes educator said
“I may know what is best for another person’s health, but I am ignorant and arrogant if I think I know what is best for
another person’s life.”14
Using the Te Whare Tapa Whā framework
Te Whare Tapa Whā is a conceptual framework developed as a way to view Māori well-being in a broad context. Over time
Te Whare Tapa Whā has become a basis for developing health practice from national policy to models of service delivery.
The four realms of this framework are centred on taha wairua (the spiritual side), taha hinengaro (thoughts and feelings),
taha tinana (the physical side), and taha whānau (family).
Te Whare Tapa Whā encourages health professionals to consider not only the physical person and their conditions, but
also the other elements of the framework when consulting with patients. It is seen as being a way to both enhance the
relationship between the patient and the health professional, and to support health outcomes. By linking the benefits
of an intervention to the ability of a patient to participate fully in all aspects of their life, from personal to community,
the patient is encouraged not to think of medicines in isolation. An example of describing cardiovascular risk management
using the four elements of Te Whare Tapa Whā is shown in Table 1.
Health professionals need to have a good understanding of a patient, including their whānau, beliefs, education and
values in order to use the Te Whare Tapa Whā framework effectively. Asking patients what they see as being important
in their life and talking about their priorities allows health professionals to gain a wider knowledge about patients
they are consulting with.
Table 1: Engaging patients in cardiovascular risk management using the Te Whare Tapa Whā framework
| Wairua (Spiritual) |
Hinengaro (Psychological) |
Tinana (Physical) |
Whānau (Family) |
| Improved health provides a sense of well-being or happiness that is likely to be
noticed by whānau |
Improved cardiovascular management provides greater confidence in health and reduces
anxiety |
Improved cardiovascular health means participation in, and enjoyment from, a wider
range of physical activities |
Knowledge that family members are likely to live longer provides a sense of security
for the whānau |
The “how to” of cardiovascular risk assessment
The current recommendation for the age at which patients should first be offered a cardiovascular risk assessment depends
on a variety of unmodifiable and modifiable risk factors (Table 2).
Calculations of cardiovascular risk using Framingham-based equations for patients outside the age range of 35 – 75*
years are less accurate, but may still be useful for the purposes of shared decision-making.5 This includes:5
- Patients with a HDL < 0.7 mmol/L - because there is a risk they have a genetic lipid disorder
- Patients with known familial dyslipidaemias or suspected genetic lipid disorders
- Patients with type 1 diabetes, type 2 diabetes with microalbuminuria or type 2 diabetes for longer than ten years
* In patients aged under 35 years their risk level should be calculated as if they are were aged 35 years.5
What should be recorded when performing a cardiovascular risk assessment?
The recommended information required to perform a five-year cardiovascular assessment is listed in Table
3.
If the patient’s total cholesterol (TC) or total cholesterol:high-density cholesterol (TC:HDL-C) ratio is above 8 mmol/L
then the test should be repeated, and a fasting lipid test considered if the patient has never had their lipid levels
measured before.5 It is acceptable to use blood pressure and non-fasting TC, HDL-C and HbA1c that have been
recorded in the previous five years for cardiovascular risk assessment, if the patient’s circumstances have not significantly
changed.5 The clinical importance of a current cardiovascular risk assessment rises as the patient’s cardiovascular
risk increases.5 Following an assessment the recommended risk factor monitoring period is determined by the
individual patient’s level of cardiovascular risk:5
- For patients with established cardiovascular disease initially at three months, then as clinically indicated
- For patients with a cardiovascular risk greater than 20%, annually, or as clinically indicated
- For patients with a cardiovascular risk from 10 – 20% as clinically indicated with a more intensive focus on patients
with a higher combined risk. If the patient is not taking medicines to reduce their risk then offer reassessment at
one year, for patients with a risk from 15 – 20%, and every two years for patients with a risk from 10 – 15%.
- For patients with a cardiovascular risk of less than 10% offer a further assessment in five to ten years
Cardiovascular risk is adjusted for some patient groups
The following patient groups will have 5% automatically added to their cardiovascular risk by the calculator as current
Framingham-based estimates will tend to underestimate their cardiovascular risk:5
- Māori, Pacific or Indo-Asian peoples
- Patients with diabetes and microalbuminuria or persistent proteinuria, or diabetes for longer than ten years, or
with HbA1c consistently ≥ 64 mmol/L
- Family history of premature coronary heart disease or ischaemic stroke in a first-degree relative
 A new cardiovascular disease risk assessment equation based on New Zealand
data is anticipated to be available later in 2014.
A new cardiovascular disease risk assessment equation based on New Zealand
data is anticipated to be available later in 2014.
Table 2: The recommended age in years to begin cardiovascular risk assessments in patients without
cardiovascular disease, adapted from Cardiovascular Disease Risk Assessment, 2013.5
| Patient group |
Males (years) |
Females (years) |
Patients without symptoms or known risk factors |
45 |
55 |
Māori, Pacific or Indo-Asian patients* |
35 |
45 |
Patients with known cardiovascular risk factors or at high risk of developing diabetes |
35 |
45 |
Family history of:
- Diabetes in a first-degree relative
- Premature coronary heart disease or ischaemic stroke in a first-degree relative (father or brother < 55 years,
mother or sister < 65 years)
|
35 |
45 |
Personal history:
- Current smoker, or have quit smoking in the past 12 months
- Gestational diabetes or polycystic ovary syndrome
- Blood pressure ≥ 160/95 mmHg or TC:HDL ≥ 7
- HbA1c 41 – 49 mmol/mol
- BMI ≥ 30 or truncal obesity ≥ 100 cm in men or ≥ 90 cm in women
- eGFR < 60 mL/min/1.73m2
|
35 |
45 |
Patients with type 1 or type 2 diabetes |
Annually from diagnosis |
Annually from diagnosis |
*Indo-Asian peoples include: Indian, including Fijian Indian, Sri Lankan, Afghani, Bangladeshi, Nepalese,
Pakistani and Tibetan
Table 3: The recommended information to be recorded when performing a cardiovascular risk assessment,
adapted from Cardiovascular Disease Risk Assessment, 2013.5
| Category |
Record |
Patient characteristics |
- Age
- Gender
- Ethnicity
- Smoking status
|
Family history |
- Type 2 diabetes
- Premature coronary heart disease or ischaemic stroke in a first-degree relative (father or brother < 55 years,
mother or sister < 65 years)
- Genetic lipid disorder
|
Medical history |
- Diabetes
- History of cardiovascular disease
- Renal impairment
- Atrial fibrillation
- Genetic lipid disorder
|
Medical history |
- One sitting blood pressure for the purposes of risk assessment, if not above 160/95 mmHg, otherwise the average
of two
- BMI and waist circumference
- HbA1c
- Non-fasting lipid profile
|