View / Download pdf version
Falls prevention is everyone’s business. A new study shows that the Accident Compensation Corporation (ACC) accepts
more than 260 falls-related claims each day from retirement-age New Zealanders.1 Figures such as this underline
why the Health Quality & Safety Commission is revisiting reducing harm from falls as the latest six-month focus of
its Open for better care national patient safety campaign, in partnership with First, Do No Harm in the Northern
region.
The new focus, which builds on work across the sector and the Commission’s ongoing reducing harm from falls programme,
began on 1 April, in tandem with
April Falls
month. April Falls, now in its third year, is an annual Commission-supported
promotion for district health boards (DHBs) and other providers, and is aimed at those working in the health and disability
and aged residential care sectors, as well as consumers and their family/whānau. Embraced around the country, each April
it raises awareness about falls in older people, galvanising sector focus and re-energising vigilance in reducing harm
from falls and keeping older people safe while in our care. An innovative component is the third annual
April Falls
quiz to promote learning (individually or in groups). Entrants can win one of three prizes based around a development
activity that improves the capability of an individual, team or organisation.
Sharing the theme “Stand up to Falls”, this year’s April Falls and the overall campaign focus are emphasising the importance
of an integrated whole-of-system approach to falls – incorporating primary care, along with community, aged residential
care and hospital settings.
Why falls and why older people?
Work on the Commission’s reducing harm from falls programme began in mid-2012, with the first national April Falls promotion
in 2013. This was followed the next month by falls as the inaugural focus of the Open campaign.
The Commission leads the falls programme, with partners that include ACC and other key stakeholders. Older people are
the focus because, although falls occur at all ages, older people are at greater risk and are more susceptible to injury.2 For
an older person, a fall can be life-changing, impacting on their independence and wellbeing, with implications for their
family/whānau.
The first priority and focus for the programme was older people in care settings – hospital, aged residential care and
receiving care at home. This is because two things can be assumed about care settings: a degree of vulnerability on the
part of the older person and the need for a safe care environment. In the case of hospitals, falls are high harm events
for patients, consistently representing around half of all serious adverse events reported to the Commission.3 However,
further evidence indicated the volume of falls in the community and the need for a broader approach aimed at helping older
people stay independent and keeping them “on their feet”.4 Consequently, programme activities have grown
from the initial emphasis on the hospital setting to also supporting and promoting primary care and community-based efforts
for older people – which includes those who are generally healthy and active and those at risk of falling because of frailty
or other factors.
Falls are the most common and costliest cause of injury in older people
An important founding document for the Commission programme was the research paper Falling
costs: the case for investment by internationally recognised University of Otago falls prevention researchers Associate
Professor Clare Robertson and Professor John Campbell.5 They reported that falls are the most
common and costliest cause of injury in older people, with around 30 – 60% of people aged 65 and over falling each year
and 10 – 20% of those falls resulting in injury such as hip fracture, hospitalisation or death.6 “Falls
can result in fear of falling with subsequent avoidance of physical activity and decline in health, and they
are an independent predictor of premature admission to residential aged care, even if there is no injury.”5
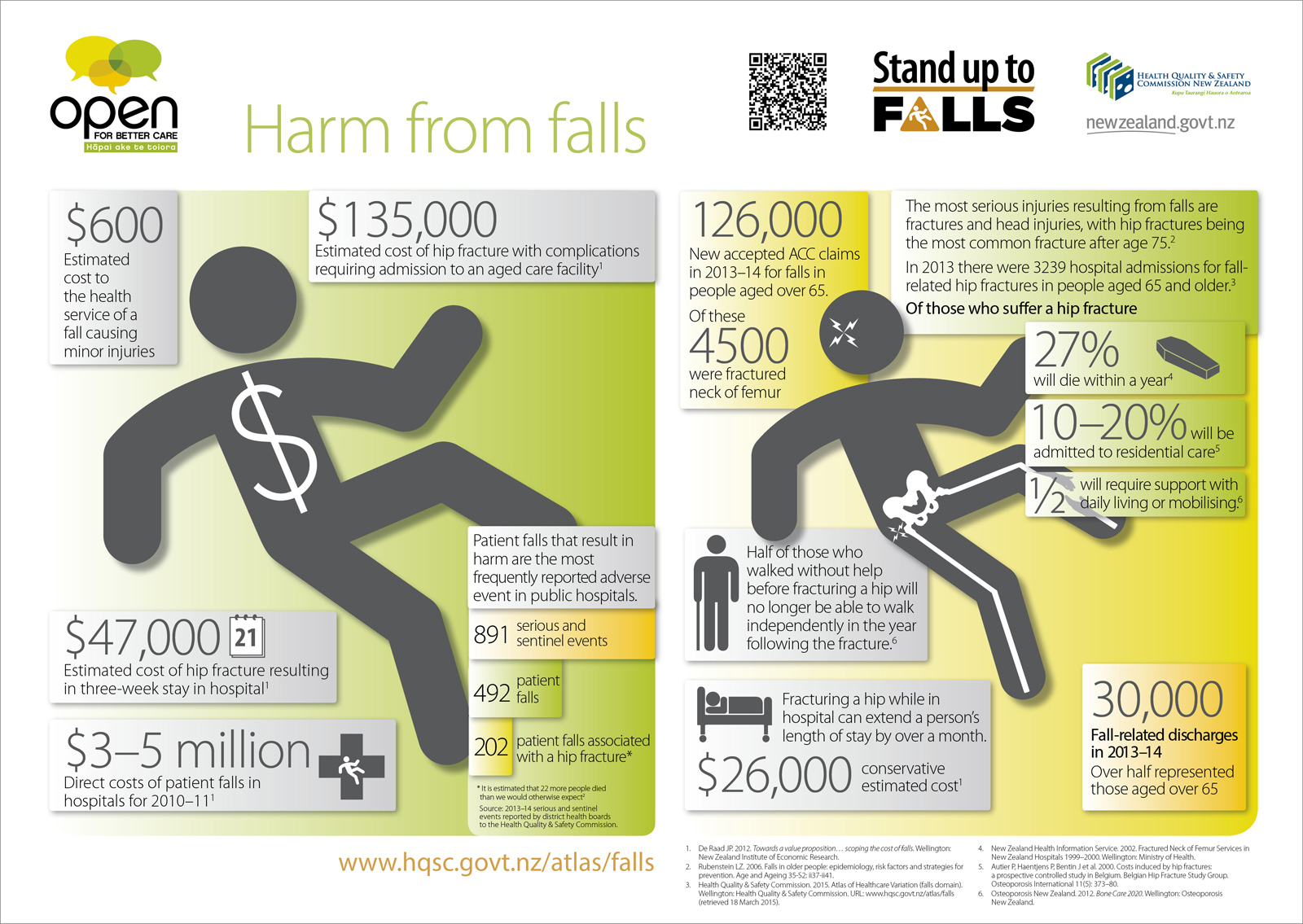
One estimate of the health service cost of falls is:4
- $600 for a fall with minor injuries
- $47,000 for a hip fracture with three weeks in hospital
- $135,000 for a hip fracture with complications and discharge to an aged residential care facility.
Of those who have a hip fracture, 27% will die within a year,7 10 – 20% will be admitted to residential
care,8 and 50% will require support with daily living or walking.9
Atlas of Healthcare Variation
To coincide with the launch of April Falls and the new campaign focus on falls, the Commission is publishing the findings
of a new falls domain in its Atlas of Healthcare Variation – a series of easy-to-use maps, graphs, tables and commentaries
to highlight differences in the provision and use of specific health services and outcomes.1
The falls domain shows data relating to falls by people aged 50 years and over, by DHB area. The data is based on people
with one or more accepted ACC claim in 2013, as well as on falls-related hospital admissions and hip fracture rates for
the same year.
In 2013, there were:1
- 92,301 people aged 50–64 years with one or more accepted ACC falls claim
- 44,140 people aged 65–74 years with one or more accepted ACC falls claim
- 33,142 people aged 75–84 years with one or more accepted ACC falls claim
- 20,103 people aged 85 years and over with one or more accepted ACC falls claim.
The figure for people aged 85 years and over represented a quarter of those in that age group and 55 accepted claims
a day. People aged 85 years and over were twice as likely to have an accepted claim as those aged 50–64 – and 15 times
more likely to be admitted to hospital as a result. Their average length of stay was 14.3 days. Although those aged 85
years and over make up 5% of the 50–plus age group, they account for nearly half of hip fractures relating to a fall.1
Falls are the most common and costliest cause of injury in older people, with around
30 – 60% of people aged 65 and over falling each year and 10 – 20% of those falls resulting
in injury such as hip fracture, hospitalisation or death.
Are falls inevitable?
In Falling costs, Robertson and Campbell showed the evidence in favour of effective interventions to help prevent falls,
concluding: “The population in New Zealand aged ≥65 years is projected to grow nearly three times by 2050, while
those aged ≥85 years will grow six times. With increasing numbers of older people and increasing incidence of serious
fractures such as hip fracture, associated health care costs will continue to rise […] The incontrovertible rationale
for investing health care expenditure in effective, cost-effective falls prevention strategies includes the rising costs
and the serious consequences of falls in older New Zealanders.”5
The Commission – through its falls programme as well as April Falls and the campaign focus on falls – supports and encourages
a number of proven preventive measures that can be integrated into routine health care.
These include:
- Exercise programmes, such as the Otago Exercise Programme, and group exercise classes, such as tai chi, which can reduce
falls by 30–40% in older people living in the community10
- Vitamin D prescribed for those at risk of vitamin D deficiency
- Home safety assessments and modifications where necessary
- Individually targeted multi-factorial interventions
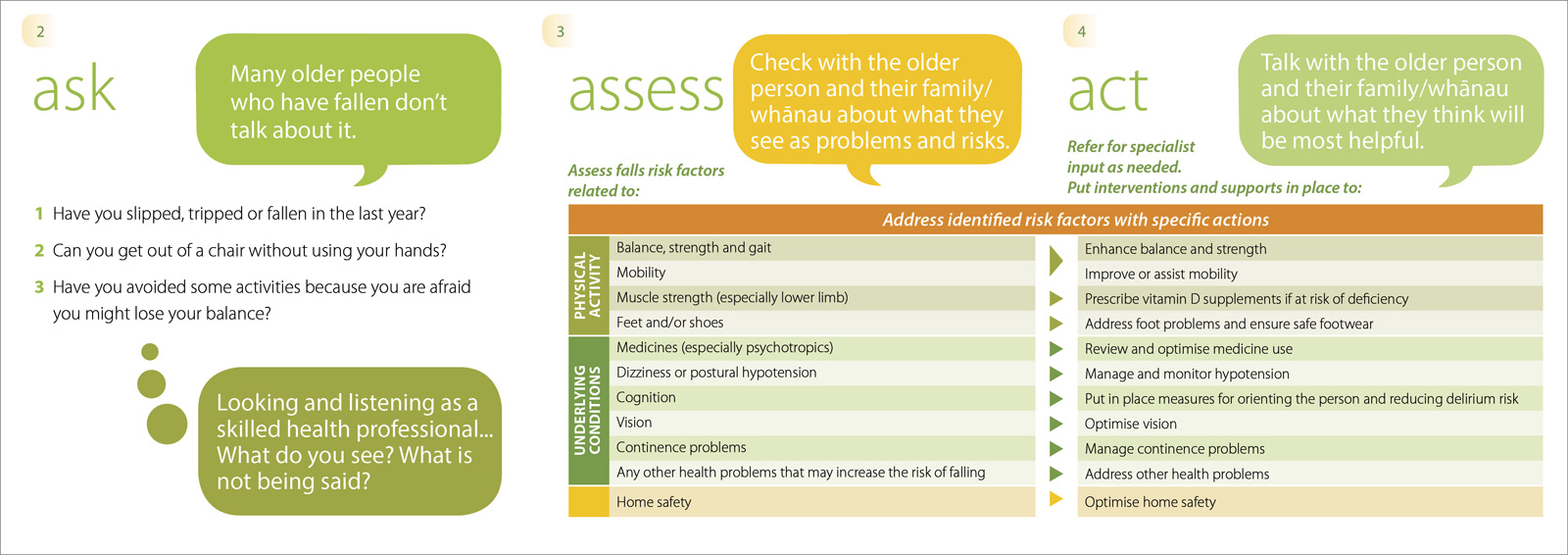
A suite of resources support the programme’s development of the “Ask, assess, act” concept – which poses the question:
“Is the older person in your care at risk of falling?” It encourages early conversations in screening for falls risk,
assessing those risk factors, and putting individualised interventions and supports in place as needed. While originally
developed with a focus on the hospital environment, the approach and tool is equally relevant across other settings.
Every older person is different
Underpinning the Commission falls programme are two fundamental principles:
- The need for individualised care. As British patient safety and falls expert Frances Healey says: “Every older
person is different. Don’t try to answer the question ‘What will stop older people falling?’ and just repeatedly
ask ‘What might stop this person falling?’”11
- The need for an integrated approach – with the aim of getting “the right people, doing the right things, in the
right order, at the right time, in the right place, with the right outcome”.12 That is to say, ensuring
services are coordinated around the needs and goals of the older person, their family/whānau and other carers.
Resources
The Commission has many free resources available for primary care practitioners as well as consumers and their families/whānau.
Links are available at the reducing harm from falls home page (www.hqsc.govt.nz/our-programmes/reducing-harm-from-falls)
and include:
Ask, assess, act (see above) – help-sheets, pocket cards and promotional posters are among the materials
that support this process, available from: www.hqsc.govt.nz/our-programmes/reducing-harm-from-falls/projects/ask-assess-act
Atlas of Healthcare Variation (see above) – other information in this interactive resource includes
about bisphosphonate and vitamin D received on discharge from hospital after a hip fracture. Available from: www.hqsc.govt.nz/atlas/falls
Audio-visual – Staying safe on your feet at home and Staying safe on your feet in the
community are among the programme’s videos. Available from: www.hqsc.govt.nz/our-programmes/reducing-harm-from-falls/publications-and-resources/videos
Dame Kate Harcourt story book and photo album – actress Dame Kate had a fall in late 2013 and these
resources tell about her injuries and the impact on her life while recovering, as well as about her resilient response
and new awareness of preventing falls at home. Available from: www.hqsc.govt.nz/our-programmes/reducing-harm-from-falls/april-falls/2014/dame-kate-harcourt-resources
Focus on Falls – the programme’s quarterly newsletter (is for everyone interested in understanding
and preventing falls in older people. Available from: www.hqsc.govt.nz/our-programmes/reducing-harm-from-falls/publications-and-resources/focus-on-falls)You
can sign up to receive the newsletter at www.hqsc.govt.nz/footer/subscribe
Patient information – available from: www.hqsc.govt.nz/our-programmes/reducing-harm-from-falls/projects/patient-information,
this is a package of downloadable materials, including ACC’s home safety checklist: www.acc.co.nz/PRD_EXT_CSMP/groups/external_ip/documents/checklist/prd_ctrb122330.pdf and Standing
up to falls: your guide to preventing falls and protecting your independence: www.acc.co.nz/PRD_EXT_CSMP/groups/external_ip/documents/guide/wim2_059285.pdf
10 Topics in reducing harm from falls – these downloadable PDFs cover core issues in falls prevention,
based on current evidence and best practice, and provide links to further resources (including videos and patient stories).
The topics are: Falls in older people: the impacts (1); Which older person is at risk of falling? Ask, assess, act
(2); Falls risk assessment and care planning – what really matters (3); Safe environment and safe care: essential in preventing
falls (4); After a fall: what should happen? (5); Why hip fracture prevention and care matters (6); Vitamin D and falls:
what you need to know (7); Medicines: balancing benefits and falls risk (8); Improving balance and strength to prevent
falls (9); and An integrated approach to falls in older people: what is your part? (10). Available from: www.hqsc.govt.nz/our-programmes/reducing-harm-from-falls/10-topics
Vitamin D prescribing – the programme’s page for this (www.hqsc.govt.nz/our-programmes/reducing-harm-from-falls/projects/vitamin-d)
has a downloadable consumer information brochure (www.hqsc.govt.nz/assets/Falls/PR/ACC-VitD-brochure-Aug-2014.pdf)
and a promotional poster for display in general practices
(www.hqsc.govt.nz/assets/Falls/10-Topics/topic7-vitamin-d-supplementation-posters-Dec-2013.pdf),
as well as residential care case studies (www.hqsc.govt.nz/our-programmes/reducing-harm-from-falls/10-topics/topic-7/case-studies).
ACC – Visit www.acc.co.nz/olderfalls for
ACC falls resources.
April Falls and Open for better care
You can follow April Falls activities here: www.hqsc.govt.nz/our-programmes/reducing-harm-from-falls/april-falls and
other falls campaign activities here: www.open.hqsc.govt.nz/falls.
Both April Falls and the campaign will be using the resources above alongside new ones.
April Falls will include local and regional activities across DHB regions, a national webinar about the Atlas of Healthcare
Variation falls findings on 14 April, 8–9 am (www.open.hqsc.govt.nz/falls/news-and-events/event/2051),
and the April Falls Quiz.
During the Open focus on falls, the Commission, in partnership with ACC and other key stakeholders, will be
launching a new ‘Stay independent’ toolkit for primary care practitioners and their patients, and sending out DHB-specific
posters showing how many of their 50–plus population were hospitalised in 2013 after a fall.
References
- New Zealand Health Quality & Safety Commission. Atlas of Healthcare Variation Falls Domain. Wellington: Health
Quality & Safety Commission, 2015. Available from: www.hqsc.govt.nz/atlas/falls
(Accessed Mar, 2015).
- Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age and Ageing 2006;35–S2:ii37–ii41.
- New Zealand Health Quality & Safety Commission. Making health and disability services safer – Serious adverse
events reported to the Health Quality & Safety Commission 1 July 2013 to 30 June 2014. Wellington: Health Quality & Safety
Commission, 2014.
- De Raad JP. Towards a value proposition…scoping the cost of falls. Wellington: New Zealand Institute of Economic
Research, 2012.
- Robertson MC, Campbell AJ. Falling costs: the case for investment. Report to New Zealand Health Quality & Safety
Commission. Dunedin: University of Otago, 2012.
- Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age and Ageing 2006;35¬–S2:ii37–ii41.
- New Zealand Health Information Service. Fractured neck of femur services in New Zealand hospitals 1999–2000. Wellington:
Ministry of Health, 2002.
- Autier P, Haentjens P, Bentin J, et al. Costs induced by hip fractures: a prospective controlled study in Belgium.
Belgian Hip Fracture Study Group. Osteopor Int 2000;11(5): 373–80.
- Osteoporosis New Zealand. Bone Care 2020. Wellington: Osteoporosis New Zealand, 2012.
- Robertson MC, Campbell AJ, Gardner MM, Devlin N. Preventing injuries in older people by preventing falls: a meta-analysis
of individual-level data. J Am Geriatric Soc 2002;50(5):905–11.
- Healey F. Reducing harm from falls. Wellington: New Zealand Health Quality & Safety Commission. Available from:
www.hqsc.govt.nz/our-programmes/reducing-harm-from-falls
(Accessed Mar, 2015).
- Allen D, Gillen E, Rixson L. Systematic review of the effectiveness of integrated care pathways: what works, for
whom, in which circumstances? Int J Evid Based Healthc 2009;7(2):61–74.