In this article 
View / Download pdf
version of this article
Contributed by Professor D Robin Taylor, Medical Adviser, Asthma and Respiratory Foundation of New
Zealand
THE GOOD NEWS ABOUT ASTHMA is that hospital admission rates have halved since their peak in the mid 1980s. The bad news
is that they have remained almost static for the last ten years, and are still occurring at twice the rate of the 1970s
(Figure 1). Hospital admissions are a good surrogate for other important morbidity associated with asthma e.g. days off
work and school. The problem of asthma morbidity still requires our attention.
One approach to this problem has been the promotion of Self Management Plans (occasionally referred to as Action Plans
if the focus is exclusively on how to treat acutely deteriorating asthma). These are designed to encourage early intervention
so that even if an acute exacerbation of asthma cannot be prevented, perhaps its severity can be significantly reduced.
The literature is mixed as to the success of Self Management Plans ranging from enthusiasm to ambivalence.1–3 Perhaps
for this reason, complacency has set in and they have become less commonly used. In one Canadian report only about 10%
of patients with asthma had an Action Plan.4
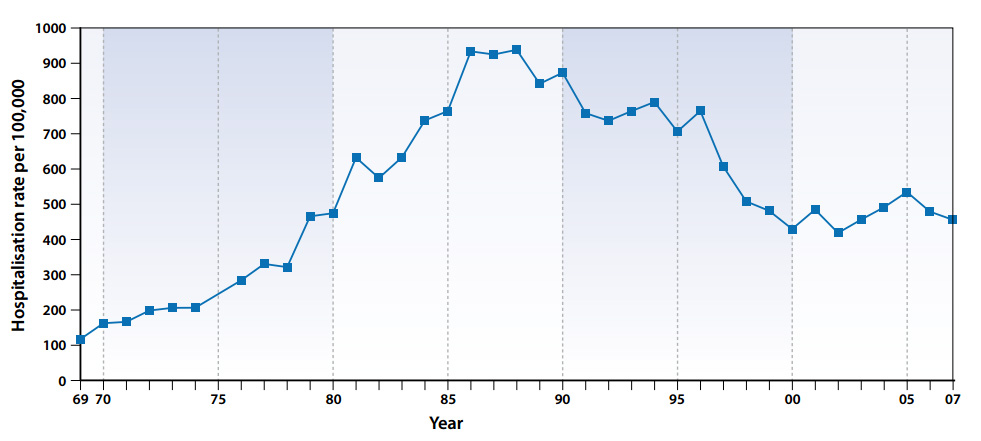 |
| Figure 1: New Zealand hospital admission rates for asthma |
Targeting vulnerable patients
Plans are not necessary for everyone. However, at the very least, Self Management Plans should be given to individuals
who are susceptible to troublesome or life-threatening asthma. This is judged on their individual history. What has happened
in the past has the potential to happen again in the future. If a patient’s history includes life-threatening episodes,
hospitalisation, or more commonly, the need for a course of oral steroid, then time and effort should be devoted to providing
a Plan for these individuals so that the past is not repeated. Patients with “brittle asthma” should also
be targeted.
Educational and other objectives
The aim is to empower patients to take action which will reduce the severity of asthma exacerbations and hence the risk.
Delay should be avoided. Limited access and the financial cost of medical advice after hours or at weekends should be
factored in. Any disincentive to early intervention should be addressed. There is clear evidence that a Plan should be
written rather than just oral. If possible it should be provided to a carer or immediate support person as well as the
patient.
Heeding the warning signs
It helps to work through and reflect on the narrative of a previous asthma exacerbation and focus on key warning signals.
Plans should usually be based on changes in symptoms rather than peak flows. The onset, or an increase in night waking
or an increasing need for “reliever” inhaler medication, are classic signs of deteriorating asthma.
Using peak flows should be encouraged to objectively verify what the patient is experiencing. In “poor perceivers” they
may have an even more critical role. If possible use peak flow data from a previous exacerbation. For example, if a patient
previously required admission to hospital and at that time the peak flow was 250 L/min., then this is clearly undesirable
irrespective of whether it is 70% or 40% of the predicted peak flow. The intervention with oral steroid should have begun
when the peak flow reached say 350 L/min. There is scope for variation in the threshold for intervention depending on
experience.
Intervention
Instructions should be given regarding the use of “reliever” bronchodilator as well as the use of oral prednisone.
The liberal use of beta-agonist in this setting is not contra-indicated, but adverse effects may occur when consumption
remains high for more than a few days. The use of Symbicort (formoterol/budesonide) as “reliever” (so-called
SMART regimen) should be limited to 12 additional doses. Thereafter if bronchospasm persists, salbutamol via a spacer
should be used.
Different practitioners may advise different regimens for oral prednisone tapering. There is no evidence one way or
the other. What the patient has used in the past and is familiar with will usually suffice. Prednisone 40 mg/day for five
days followed by 20 mg/day for five days is our usual “recipe”. It is not set in stone. A shorter period of
treatment may suffice. It may also be appropriate to give the patient a supply of prednisone tablets.
The Asthma and Respiratory Foundation of New Zealand has developed a revised version of its Self-Management Plan for
asthma (available from www.asthmanz.co.nz). Patients with asthma,
as well as their family doctors and practice nurses, are encouraged to revisit using a Self Management Plan. Perhaps we
can again make inroads into reducing asthma morbidity in New Zealand.
Further reading
- Gibson PG, Powell H. Written action plans for asthma: an evidence-based review of the key components. Thorax 2004;59(2):94-9.
- Toelle BG, Ram FS. Written individualised management plans for asthma in children and adults. Cochrane Database Syst
Rev 2004(2):CD002171.
- Zemek RL, Bhogal SK, Ducharme FM. Systematic review of randomized controlled trials examining written action plans
in children: what is the plan? Arch Pediatr Adolesc Med 2008;162(2):157-63.
- Beauchesne MF, Levert V, El Tawil M, Labrecque M, Blais L. Action plans in asthma. Can Respir J 2006;13(6):306-10.