The burden of bipolar disorder
Bipolar disorder first appeared in the medical literature in the 1850s when alternating melancholia and mania were paired
in a single condition.1 For a number of years the diagnosis was termed “manic-depressive disorder”, but this
was replaced by bipolar disorder in 1980 when the Diagnostic and Statistical Manual of Mental Disorders, 3rd Edition (DSM-III)
was released.1 Bipolar disorder is characterised by extreme mood swings – from hopeless depression to euphoric
or irritable mania – with each episode usually bookended by symptom-free periods referred to as euthymia (Figure
1, over page).2 However, many patients will have milder symptoms which can make diagnosing bipolar disorder
challenging. Depression is the most common symptom and people with severe forms of bipolar disorder may be symptomatically
unwell nearly 50% of the time.3
In New Zealand, bipolar disorder may be more prevalent among Māori (4.6%), compared to Pacific peoples (3.7%) and people
of European and other ethnicities (1.8%).4 The first noticeable mood disturbance in people with bipolar disorder
often occurs during adolescence; one study found the mean age of onset was 17 years (+/- 4 years).5
The mood disturbances experienced by people with bipolar disorder can vary greatly. In some people, mild episodes of
mania (hypomania, see opposite) are associated with increased creativity and productivity. In other patients, an episode
of mania may be severe enough to require immediate hospitalisation and involuntary committal under the Mental Health Act.
In between mood episodes, people with bipolar disorder may also experience cognitive impairment, e.g. problems with memory
and attention, and relationship and occupational difficulties due to residual problems caused by past behaviour.6 People
with bipolar disorder are 15 times more likely to commit suicide than people in the general population and it is estimated
that bipolar disorder may account for one-quarter of all completed suicides.6 Approximately 10 – 15% of people
with untreated bipolar disorder can be expected to die due to suicide.2
The severity of mania determines the type of bipolar disorder
General Practitioners are often the first clinician to suspect a patient has a mental illness. Although depression is
the most common symptom of bipolar disorder, mania is the cardinal feature and its severity is used by Psychiatrists to
categorise the patient’s disorder.
A full manic episode is described as a distinct period of abnormally and persistently elevated or irritable
mood, accompanied by an abnormally and persistently increased amount of goal-directed activity or energy, lasting at least
one week and present most of the day, nearly every day (see: “The DSM-V criteria for episodes of mania
and depression”).6 Secondary episodes of mania caused by medicines, drugs or other disorders,
e.g. attention-deficit/hyperactivity
disorder or personality disorders, are not part of the bipolar spectrum.6 During a manic episode a person
may develop grandiose plans, or embark upon multiple overlapping and complex projects, often without any experience in
the field, e.g. writing a novel or seeking funding for an impractical invention.6 Full mania causes a noticeable
social or occupational impairment, with poor judgement, and in some people a psychosis that causes them to be a danger
to themselves and others.6 A decreased need for sleep is an important feature of all forms of mania.6
Hypomania is characterised by the same features as mania but the patient’s episode is less severe and
does not cause the same degree of social or occupational impairment.6 During an episode of hypomania, the
patient may feel very positive, be highly productive, and function well, but people close to them will have noted the
mood swing as being uncharacteristic.7 Episodes of hypomania may last for shorter periods than episodes of
mania.
Many people with bipolar disorder will experience periods of mild depression or mania not pronounced enough to be diagnosed,
i.e. subsyndromal (sub-clinical), between more severe mood swings (Figure 1).2 A study
that analysed the weekly symptoms of patients with severe bipolar disorder in a mental health facility for 13 years, found
that almost three-quarters (74%) of symptomatic weeks involved subsyndromal depression and hypomanic symptoms.3 The
symptomatic status of patients changed on average six times a year.3 However, there is considerable individual
variation in the duration of mood cycles and the period between mood changes can be days, weeks or even years.2
Types of bipolar disorder
Bipolar I disorder is diagnosed when patients have experienced at least one episode of mania (as opposed
to hypomania).6 The mean age of onset for the first mood disorder is approximately 18 years for people with
bipolar I disorder, however, first onset has been seen in people aged over 65 years.6 Many people with bipolar
I disorder will be able to function fully between episodes, but 30% of people affected are reported to be severely impaired
at work, which can result in reduced socioeconomic status, particularly if they experience repeat episodes.6 The
incidence of bipolar I disorder is similar among females and males.6
Bipolar II disorder is diagnosed in people who have had at least one episode of depression and one
episode of hypomania, but have never experienced an episode of full mania. The average age of onset of bipolar II disorder
is in the mid 20’s; slightly later than for bipolar I disorder.6 Fifteen percent of people with bipolar II
disorder are reported to experience dysfunction between episodes.6 Clinical data suggests that bipolar II
disorder is more common in females, however, this may be because females with bipolar II disorder are more likely to seek
treatment.6
Cyclothymic disorder is diagnosed when an adult patient has had numerous subsyndromal hypomanic episodes
and numerous depressive episodes over a two year period, neither of which meet full DSM-V criteria for either mania or
depression.6 Cyclothymic disorder will progress to either bipolar I disorder or bipolar II disorder in 15
– 50% of people.2
“Rapid cycling” specifies that a patient has had four or more mood episodes, i.e. major depression,
mania or hypomania, within one year.6 Rapid cycling of moods in patients with bipolar disorder is associated
with a reduced response to treatment and poorer outcomes.8
A “mixed episode” is where the patient experiences mania and depression during the same period, for
a week or more.9 For example, during a mixed episode a patient might report feeling sad or hopeless with suicidal
thoughts, while feeling highly energised.7 Outwardly they may appear agitated with disturbed sleep patterns
and a major change in appetite.7
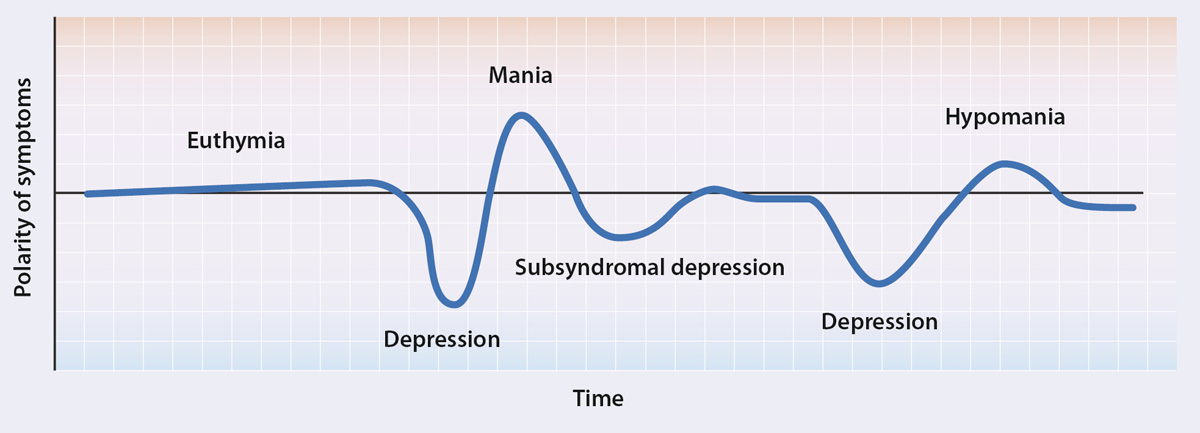
Figure 1:
The typical mood fluctuations over time of a person with bipolar disorder, adapted from Muzina et al, 20072
The cause of bipolar disorder is often multi-factorial
The cause of bipolar disorder is unknown and is likely to be multi-factorial. There is, however, a strong inheritable
component to the disorder. The risk of a first degree relative of an affected person developing bipolar disorder is between
5 – 10%, but this increases to 40 – 70% for monozygotic twins.10 There is good evidence that many genes are
involved, each contributing a small portion of the risk.10 The fact that monozygotic twins do not display
identical rates of bipolar disorder suggests that environmental influences also play a role.
Bipolar disorder is often diagnosed as major depression
It is retrospectively reported that approximately one-third of patients with bipolar disorder will have been initially
diagnosed as having major depression; this is because:2
- Depression is more common
- Depression is the most frequent symptom experienced by people with bipolar disorder and during an episode of mania
people are less likely to consider themselves unwell and therefore will not present for treatment
- The criteria for a diagnosis of major depression is the same as the diagnosis of depression in patients with bipolar
disorder
- Patients may not remember, or may be embarrassed about, manic episodes and therefore be reluctant to report them
Treatment for depression with antidepressants can have serious consequences for patients with bipolar disorder.2 If
an antidepressant is prescribed to a patient with bipolar disorder it is usually in combination with a mood stabiliser,
e.g. lithium, to reduce the risk of a swing to mania.9 Increased mood cycling has been reported in patients
with bipolar disorder taking antidepressant monotherapy.11 A study of over 3000 patients with bipolar disorder
treated with either an antidepressant alone, or an antidepressant with a mood stabiliser found that the risk of patients
requiring treatment for mania was increased almost three-fold by antidepressant monotherapy.11 The risk of
mania requiring treatment was significantly decreased after three to nine months of concurrent treatment with a mood stabiliser
and an antidepressant.11
Identifying patients who may have bipolar disorder
Due to the cyclic nature of bipolar disorder it may take months, or even years, for a patient to be diagnosed. In the
United Kingdom and the United States, the mean delay from the onset of symptoms to a correct diagnosis in a patient with
bipolar disorder has been estimated to be ten years.12 Mild symptoms or relatively infrequent swings to mania
are likely to contribute to this delay for some patients. All patients who are suspected of having bipolar disorder should
usually be referred to a Psychiatrist or an acute mental health service, depending on the severity of their symptoms and
the degree of clinical suspicion. Bipolar disorder can occur in children, but is difficult to diagnose as children may
switch between moods of happiness, silliness and irritability depending on the occasion and their level of development.6
A formal diagnosis of bipolar disorder is generally made by a Psychiatrist. An accurate and early diagnosis may decrease
mortality due to suicide in patients with bipolar disorder.
When to suspect bipolar disorder
People with bipolar disorder often have:2
- A family history of bipolar disorder or “manic depression”
- Problems with alcohol
- Displayed risk-taking behaviour in the past, e.g. sexual, financial or travel-related
- A history of complicated and disrupted circumstances, e.g. multiple relationships, switching jobs frequently or frequent
change of address
Differentiating bipolar disorder from major depression
To reduce the likelihood of patients with bipolar disorder being diagnosed with major depression, General Practitioners
should ask patients with symptoms of depression about any history of mania/hypomania. Compared to patients with major
depression, patients with bipolar disorder are more likely to display racing thoughts and/or irritability when they are
not depressed. Patients with bipolar disorder are also more likely to have suicidal thoughts during periods of depression.2 Patients
with depression who do not respond to antidepressants, or respond erratically, e.g. a rapid response within days of starting
treatment or a brief relief with a return of symptoms, should be reassessed for bipolar disorder.2
Mixed mood episodes of bipolar disorder
Patients with mixed mood episodes can be hard to diagnose; clinicians need to be alert to mixed mood episodes because
when they are combined with a lack of sleep, and/or alcohol, the risk of the patient committing suicide is greatly increased.13
Females with bipolar disorder are more likely to experience mixed mood episodes and to have more rapid cycling of episodes.13 There
is not known to be a causal relationship between episodes of bipolar disorder and the monthly female hormone cycle, although
pregnancy may be a trigger for episodes of hypomania in females with bipolar II disorder.6
Referral to a psychiatric service
An acute mental health service may be the first point of contact for family when a person with bipolar disorder experiences
a manic episode. General Practitioners may be involved in this referral, but in an acute situation the patient may present
directly to hospital. In rural areas there is often reduced access to Mental Health Services and General Practitioners
may be more closely involved in diagnosing bipolar disorder following discussion with a Psychiatrist.
The initial psychiatric assessment will be based on the patient’s presenting symptoms, the frequency and amount of time
symptoms are experienced and any available family history of mental illness. Once the possibility of medicine or substance-induced
symptoms has been excluded, DSM-V criteria are then applied to establish a diagnosis. It is important to include information
about any history of alcohol or drug use when referring patients for psychiatric assessment, as approximately 70% of patients
with bipolar disorder have a substance abuse disorder.13
Managing patients diagnosed with bipolar disorder
Generally, the management of patients with bipolar disorder is led by a Psychiatrist, and the primary care team is involved
in liaising between the psychiatric multi-disciplinary team and social services, as well as supporting the patient and
their family. Family and friends are an important support network for people with mental illness and this is particularly
important in rural areas if there is reduced access to Mental Health Services. General Practitioners usually provide repeat
prescriptions and monitor the patient’s adherence to, and the effectiveness of treatment. Many of the medicines used to
treat bipolar disorder have significant adverse effects and a proactive approach to patient management, e.g. reducing
cardiovascular risk, is required. More than half of patients with bipolar disorder also have an alcohol use disorder which
can complicate any assessment of the patient’s mood and increases the risk of the patient attempting suicide.6
Medicines are the mainstay of treatment, however, self-management of bipolar disorder and engagement with the patient’s
family is also essential. It is important to educate patients and their families about bipolar disorder, to help reduce
stigma, and to address any confusion between bipolar disorder and other forms of mental illness such as schizophrenia.
Ensure that the information provided is understood by the patient and their family and is presented in a culturally appropriate
way. Patients who have an understanding of their condition may be better equipped to recognise when a change in mood is
about to occur.
Patients can reduce the likelihood of experiencing mood swings by maintaining daily routines that include regular medicine
use and healthy sleep patterns, exercise and avoidance of alcohol.9 Maintaining a daily pattern of activity
can have positive effects for patients with bipolar disorder and reduce the likelihood of new mood episodes.15 Treatment
non-adherence in patients with bipolar disorder is a major risk factor for relapse.9 Ongoing education about
bipolar disorder for the patient and their family increases the likelihood that patients will adhere to treatment.16

Traditional Māori beliefs about mental illness
Listening, being respectful to other points of view and understanding one’s own cultural values are core components
of cultural competency that make reconciling different belief systems easier.
Traditional explanations for mental illnesses in other cultures can be quite different to those of Western medicine,
and there is the potential for conflict between traditional Māori and Western psychiatric approaches to mental health.
For example, Mate Māori is considered to be a cause of illness or uncharacteristic behaviour resulting from an infringement
of tapu or the infliction of an indirect punishment. It may take several forms, both physical and mental, and can be an
explanation to Māori for emotional, behavioural or psychiatric disorders. Māori may be reluctant to discuss mate Māori
with clinicians due to fear of ridicule or perceived pressure to choose between psychiatric and Māori beliefs. However,
the two approaches can co-exist. Mate Māori does not exclude a mental disorder and may be used to help understand the
cause of the illness.
Traditional Māori beliefs are an area of expertise of tohunga and kaumātua assisted by kaitakawaenga (Māori cultural
workers). It is appropriate to seek expert cultural assistance if these concepts arise when working with Māori.
 For further information see: “
Recognising and managing mental health problems in Māori”, BPJ 28 (Jun, 2010).
For further information see: “
Recognising and managing mental health problems in Māori”, BPJ 28 (Jun, 2010).
Pharmacological treatment of symptoms
Many of the medicines used to treat patients with bipolar disorder have potentially severe adverse effects and treatment
choices may vary as the patient’s symptoms change. The initial choice of treatment depends on whether the patient is manic
or depressive, the severity of their symptoms, patient preference and the balance of benefit versus risk of adverse effects.
Treatment decisions are often made by the Psychiatrist who will prescribe additional medicines if required, e.g. if the
patient undergoes rapid cycling of their mood. The General Practitioner should alert the Psychiatrist to any changes in
the patient’s mood that might require a change in treatment.
Lithium has been used for over 60 years for the treatment of bipolar disorder and is still frequently prescribed (see:
”Monitoring the safe use of lithium”).16 Other medicines used in the management
of patients with bipolar disorder include mood stabilisers, antipsychotics and antidepressants. Patients will usually
require ongoing laboratory monitoring while taking these medicines (Table 1), and prescribers need
to consider potential medicines interactions. For example, oestrogen-containing medicines such as combined hormonal contraceptives
can reduce the effectiveness of lamotrigine.
 See the New Zealand Formulary for
details on medicine interactions.
See the New Zealand Formulary for
details on medicine interactions.
Medicine choices may be different in females with bipolar disorder who may become pregnant – lithium, valproate and
carbamazepine are all associated with a risk of foetal abnormalities (Pregnancy Risk Category D) and effective contraception
is recommended for all females of child-bearing age who are taking these medicines.17 The risk to foetal development
is higher if these medicines are used in the first trimester, or in combination.17 Valproate is associated
with the highest risk and should be avoided in women of child-bearing age.17
Treatment of episodes of mania
Patients and their families should be educated in detecting early signs of manic episodes, e.g. increased activity or
a decreased need to sleep.13 When this occurs, encouraging the patient to continue their treatment and maintain
a daily routine is important; patients who are manic may not feel they need treatment. Reducing stimulants, such as coffee,
is recommended and it should be reiterated that restoration of sleep is an important aspect of treatment.9 During
an acute episode of mania the patient’s safety and the risk of their reputation being damaged should be assessed, along
with any potential safety risk to others. It may be necessary to contact a Mental Health Service if there are safety concerns
involving dependents, or where the patient exhibits a marked loss of control, poor judgement or will have difficulty managing
a concurrent long-term condition, e.g. type I diabetes. During an episode of mania a person may engage in indiscriminate
sexual encounters without regard for the risk of sexually transmitted infections, pregnancy or the social consequences
of their actions; long-term contraception, e.g. Depo-Provera, may be appropriate for some female patients.6
A Psychiatrist is likely to recommend the tapering and then withdrawal of medicines that may enhance manic episodes,
e.g. antidepressants.9 Depending on the individual patient, the following medicines may be prescribed for
treating mania in a patient with bipolar disorder:9
- Lithium is effective in treating patients during a manic episode and is useful for its antisuicidal properties. However,
lithium takes six to ten days to take effect and therefore may be used initially in combination with short-term antipsychotics
and benzodiazepines. For example, lorazepam may be used for several days and gradually withdrawn as the patient’s condition
improves.16
- Valproate may provide a more rapid response than lithium
- An atypical antipsychotic may be prescribed alone or in combination with either lithium or valproate
- The typical antipsychotic haloperidol is effective at controlling acute mania, but does not prevent depression and
has an increased risk of extrapyramidal adverse effects
Approximately half of patients with an episode of mania can be expected to respond to monotherapy with either lithium,
valproate or an atypical antipsychotic, while three-quarters of manic patients are likely to respond to a combination
of either lithium or valproate with an atypical antipsychotic.9 The same medicines that are used to treat
mania may be prescribed for patients with hypomania, although the dose may be lower.2 Electroconvulsive therapy
(ECT) may be effective for patients with treatment-resistant mania or depression and may be considered if the adverse
effects of pharmacological treatment are a serious concern, e.g. women who are pregnant.2,3
Treatment of episodes of depression
Early symptoms of an episode of depression may include a loss of energy, difficulty concentrating and a low mood.13 Treatment
adherence is also an issue during periods of depression as patients may feel their treatment regimen is a burden to them.13 During
a depressive episode patients are at an increased risk of suicide.9
A Psychiatrist may prescribe lithium, valproate or lamotrigine as a mood stabilising regimen for depression in patients
with bipolar disorder.9 This will then allow for the safe use of antidepressants, e.g. an SSRI, without an
increased risk of mania developing.9 If an antidepressant is prescribed for patients with bipolar disorder,
SSRIs are preferred (in combination with another medicine) to tricyclic antidepressants as they are less dangerous if
taken in overdose.9 Atypical antipsychotics may be used to settle agitation often seen in patients with depression
and mania; whether these medicines have specific antidepressant or mood stabilising actions is uncertain.
Treatment of patients with rapid cycling or mixed episodes
Patients with rapid cycling or mixed episodes may be more difficult to manage than those with either an isolated episode
of mania or depression. Different combinations of medicines may be appropriate for these subtypes of bipolar disorder.
Rapid cycling can be induced by substance use and antidepressant monotherapy.9
Depending on the individual patient, the following medicines may be prescribed for treating rapid cycling of mood in
patients with bipolar disorder:9, 16
- Valproate, lithium, olanzapine, lamotrigine or quetiapine as monotherapy
- Lithium with valproate and lithium with carbamazepine or lamotrigine, in combination
Depending on the individual patient, the following medicines may be prescribed for treating mixed episodes in a patient
with bipolar disorder:16
- Olanzapine, quetiapine and valproate, usually with a mood stabiliser
- Olanzapine with fluoxetine or valproate with olanzapine in combination
Table 1: Guidelines for monitoring medicines used in bipolar disorder9, 17, 18
|
Baseline investigation |
Ongoing monitoring |
Lithium |
See: "Monitoring the safe use of lithium" |
See: "Monitoring the safe use of lithium" |
Valproate (sodium) |
Identify any history of haematological or hepatic disease.
Measure FBC, LFT, electrolytes and creatinine.
Advise the patient to stop treatment and seek medical attention if dermatological, liver or haematological-related
adverse effects develop (see next column). |
Measure weight, FBC, LFTs every three months for one year and then annually. Patients should seek medical advice
if they develop fever, infection, rash, abdominal pain, vomiting, yellowing of the skin, bruising or bleeding.
Reproductive endocrine disorders, e.g. menstrual disorders, polycystic ovary syndrome and hyperandrogenism are more
common in females taking valproate.19 Valproate (pregnancy risk category D) should not be used during
pregnancy or in females of childbearing age unless there are no safer alternatives, in which case
effective contraception should be used.
Valproate can reduce bone mineral density and the patient’s diet should contain adequate calcium. Weight-bearing
exercise can improve balance and bone strength. |
Carbamazepine |
|
Measure FBC the first month after treatment, then six-monthly. Measure LFTs, electrolytes, urea and creatinine,
monthly for three months and then annually. Patients should seek medical advice if fever, rash, mouth ulcers, bruising
or bleeding develops.
Effective contraception is recommended when carbamazepine (pregnancy risk category D) is prescribed to females of
childbearing age. |
Lamotrigine |
|
Advise patients to seek emergency medical attention if a rash develops (characteristically maculopapular and occuring
within the first eight weeks of treatment).20
Effective contraception is recommended when lamotrigine (pregnancy risk category D) is prescribed to females of childbearing
age. |
Atypical antipsychotics, e.g. olanzapine, quetiapine, risperidone, aripiprazole or ziprasidone |
Identify any family history of cardiac issues including congenital long QT syndrome |
Measure weight, weekly for first weeks of treatment to detect those at risk of rapid weight gain and then every
three months.
Measure blood pressure and HbA1c every three months for one year, then annually. In patients with an increased risk
of diabetes, test fasting glucose monthly for the first three months due to rapid rise in glucose levels, then HbA1c
every three months.
Measure lipid profile at three months and then annually.
An ECG should be requested by the prescribing clinician if the patient is at an increased risk of QT-interval prolongation,
e.g. patients with bradycardia or a history of electrolyte imbalances. Atypical antipsychotics may not be appropriate
for patients with a congenital long QT syndrome as use of atypical antipsychotics is associated with an increased risk
of sudden cardiac death.21 In theory this risk may be further increased by the concurrent use of lithium.
Measure prolactin levels in females with unexplained amenorrhoea or males with reduced libido who are taking risperidone.
CNS depression, anticholinergic effects, e.g. dry mouth and constipation, dizziness, extrapyramidal effects, e.g.
dyskinesias, may also occur. |
Managing patients during periods of euthymia
Clinicians can anticipate changes in circumstances that make a relapse of symptoms more likely and help the patient
and their family to develop stable daily routines that includes taking medicines regularly. At each consultation the clinician
should consider:
- Are the patient’s symptoms under control?
- Has there been any change in circumstances that may cause the patient excess stress, e.g. a change in occupation,
relationship status, social isolation or finances?
- Has the overall health of the patient changed, e.g. alcohol consumption, weight, smoking status or substance use?
Discussing the patient’s mood may help the patient to gain insight into their disorder and promote self-management,
e.g. moderating the use of alcohol and avoiding alcohol altogether during depressive or manic episodes. If a person with
bipolar disorder becomes symptomatic their family can assist by encouraging them to delay making any important decisions
until their mood has stabilised.
Develop strong relationships with patients and the people supporting them
The common goal of all treatment plans should be a structured and supportive relationship between the patient and their
family and the patient and the clinician. This makes communication easier and the patient is more likely to value interactions
with clinicians. Regular contact is one of the best ways to achieve this and maintain the patient’s adherence to treatment.
During the maintenance period the primary care team in conjunction with the patient’s family should:
- Monitor sleep patterns which may be an early sign of a mood change
- Monitor for subsyndromal depression
- Consider if psychological or social support, e.g. counselling, would benefit the patient. Mental Health Services are
able to meet the patient regularly in their own home in some areas.
General Practitioners should ensure they are receiving regular copies of outpatient attendance notes when the patient
visits the consulting Psychiatrist.
 The Ministry of Health has a list of resources available to people who are affected
by bipolar disorder, go to:
https://www.health.govt.nz/your-health/conditions-and-treatments/mental-health/bipolar-disorder
The Ministry of Health has a list of resources available to people who are affected
by bipolar disorder, go to:
https://www.health.govt.nz/your-health/conditions-and-treatments/mental-health/bipolar-disorder
Monitor all aspects of the patient’s health
Cardiovascular disease, obesity, and diabetes (“the metabolic syndrome”) are common among people with bipolar disorder;
long-term care of patients with bipolar disorder involves close monitoring of cardiovascular risk.12 It is
likely that the cardiovascular risk of people with bipolar disorder is increased due to higher rates of smoking and reduced
physical activity during periods of depression, as well as the adverse effects of the medicines used to manage the disorder,
e.g. weight gain and hyperlipidaemia. Advice about smoking cessation, alcohol reduction, diet and exercise should be included
in all management plans.
Contraception and pregnancy planning should be discussed with female patients due to the risk of mood stabilising medicines
causing birth defects.18 Folic acid supplementation is recommended to reduce the risk of foetal neural tube
deficits in females taking valproate and carbamazepine (although these medicines, especially valproate, are not recommended
during pregnancy or in females of child-bearing age unless there are no safer alternatives). Hepatitis B vaccination may
be appropriate for patients with a history of drug taking or promiscuous behaviour.
Monitor for other forms of mental illness
Patients with bipolar disorder can be expected to develop more than one psychiatric disorder during their lives. Many
patients with bipolar I disorder are reported to have some form of anxiety disorder and substance misuse disorders are
also common.13 Patients with bipolar disorder and co-morbid anxiety may self-medicate with alcohol or other
substances.9 Concerns about the emergence of an additional psychiatric co-morbidity should be discussed with
a Psychiatrist.
Be prepared for the lifecycle of bipolar disorder
Patients, their families and health professionals should be prepared for the cyclic nature of bipolar disorder. Some
patients will need to be admitted into hospital care during episodes of acute mania with the patient returning to community-based
care between episodes. When the patient transitions from tertiary to primary care the support of their family and General
Practitioner is important in re-establishing routines in order to reduce the risk of a relapse.
Monitoring the safe use of lithium
Lithium is an effective treatment for acute mania, acute depression and long-term mood stabilisation in people with
bipolar disorder.16 However, lithium is associated with a risk of serious adverse effects and patients need
to be monitored closely.
Lithium has a relatively slow onset of action and will take six to ten days to produce a clinical effect in patients
who are manic, and six to eight weeks for patients with bipolar depression.16 Lithium is available in 250
mg capsules, and 250 mg and 400 mg tablets.17 The bioavailability of the different formulations of lithium
varies widely, therefore if the preparation is changed, careful monitoring is required, particularly if switching between
modified and immediate-release formulations.17
Monitor serum lithium levels: Lithium has a narrow therapeutic index and patients need to be monitored
to ensure safe and effective serum lithium levels are achieved and to prevent the development of adverse effects. Local
guidelines can vary and Psychiatrists may adjust recommendations depending on the individual patient.
The patient’s lithium serum concentration should be measured five to seven days after dose initiation, or dose change,
with the blood sample taken 12 hours after dosing. Generally the patient’s serum lithium is titrated to 0.6 – 0.8 mmol/L
as this is reasonably well tolerated; a higher concentration (0.8 – 1 mmol/L) is recommended for acute episodes of mania,
17 and
for patients who have experienced a relapse or have subsyndromal symptoms. Lithium levels should be monitored weekly after
initiation and after every dose change, until a desired stable lithium level is achieved.17 Levels should
then be measured every six months and more frequently if the patient’s sodium or fluid intake changes or they develop
a concurrent illness.17 Placing a patient recall in the Practice Management System (PMS) will automatically
generate reminders. Patients should be educated to maintain adequate fluid intake, particularly during summer or during
periods of physical exertion, or febrile illness. A serum lithium level > 1.2 mmol/L is usually considered to be toxic.
A level > 2 mmol/L is a medical emergency.17
Monitor for adverse effects: Fine tremor and nausea are common dose-dependent adverse effects of lithium
treatment, but often pass after one to two days. Coarse tremor, general fatigue, vomiting, diarrhoea, a metallic taste
in the mouth, and a reduction in the sensitivity of the abdomen (central obtunding) indicate toxicity.16, 17 Adverse
effects mostly occur when lithium plasma levels change rapidly and should be anticipated when doses are increased.16
Lithium
overdose can cause chronic neural toxicity and may even be fatal.16 Lithium reduces the ability of the kidneys
to concentrate urine causing polyuria and increased thirst; it is reported that 10% of patients taking lithium long-term
will develop reversible diabetes insipidus.16 The dose of lithium will need to be reviewed in older patients
and patients with renal impairment to avoid serum lithium reaching toxic levels.
Some patients will experience weight gain of as much as 10 kg after lithium treatment is started and this can affect
treatment adherence. Hypothyroidism is reported to be six times more prevalent in patients taking lithium.16
Patients
taking lithium may develop hypercalcaemia due to elevated parathyroid concentrations.16 If hypercalcaemia
is significant then lithium treatment may need to be withdrawn.16 Lithium should be avoided where possible
during pregnancy and breast-feeding.16
If lithium is withdrawn abruptly there is an increased risk of manic relapse. When lithium treatment is ceased doses
should be reduced over a period of at least four weeks, and preferably over a period of three months.17
Monitor other laboratory parameters: Local guidelines vary for the frequency of monitoring of other
parameters and this is likely to be directed by a Psychiatrist. Table 2 provides a reasonable approach
to monitoring patients taking lithium long-term.
Medicine interactions: Angiotensin converting enzyme (ACE) inhibitors, angiotensin receptor-II antagonists
(ARBs), diuretics (particularly thiazide diuretics, e.g. bendrofluazide, hydrochlorothiazide) and non-steroidal anti-inflammatory
drugs (NSAIDs) can reduce the renal clearance of lithium and result in increased serum lithium levels.22 Where
possible the combination of any of these medicines with lithium should be avoided. If combination treatment is required
the medicines should be prescribed at a stable, rather than variable dose. Patients should be aware of the potential risk
of over-the-counter NSAIDs and advised to avoid these. Regular monitoring of renal function is recommended if medicines
which can affect renal function are taken concurrently with lithium. Medicines that affect serotonin, e.g. SSRIs, clomipramine,
tramadol and venlafaxine, can cause serotonin syndrome when taken in combination with lithium.22 Sodium restriction
can result in lithium toxicity and excess sodium, e.g. in patients taking sodium bicarbonate, can cause lithium serum
levels to fall.17
Table 2: Recommended baseline and follow-up monitoring for patients taking lithium long-term16, 17
Test |
Baseline and follow-up |
Rationale |
Serum lithium |
Five to seven days after first dose, then weekly, until stable, then every six months |
Lithium has a narrow therapeutic window |
Serum creatinine |
Baseline and every six months |
Lithium is excreted by the kidneys, therefore there is risk of reduced renal function with long-term use |
Serum electrolytes (sodium) |
Baseline and then every six months |
Sodium levels influence lithium levels |
Thyroid function (TSH) |
Baseline and then every six months. More frequently if clinically indicated |
Hypothyroidism and rarely hyperthyroidism is increased with the long-term use of lithium |
ECG in patients aged over 45 years or with cardiac problems, including hypertension |
Baseline and then yearly (if cardiac risk)22 |
Lithium can cause sick sinus syndrome and QT prolongation and baseline ECG is useful if future complications develop,
or if other medicines are added that have cardiac conduction effects |
Serum calcium |
Baseline and then yearly22 |
Lithium can cause hypercalcaemia secondary to elevated parathyroid concentrations |