Key concepts
- Thrombophilia testing is rarely indicated
- Thrombophila testing should only be performed in specific situations when the results will alter management
- Situations in which thrombophilia testing may be appropriate include; people presenting at a young age with an unprovoked
venous thrombosis and a positive family history, children with purpura fulminans and some pregnant women
Thrombophilia is the increased tendency for a person to develop blood clots. There are a number of factors that contribute
to increased thrombotic risk, many of which are well recognised and some of which are unknown. In most cases, the presence
of one or more risk factors is thought to contribute to a thrombotic event. However, in some cases, described as idiopathic
or unprovoked, a patient has no clear triggering event. Although over the last few years there has been increased interest
in laboratory tests for investigating thrombophilia, their role in general practice is limited, their use is controversial
and the results in most cases will not influence management. Testing may also lead to unnecessary anxiety and psychological
distress, given that some inherited thrombophilic traits are very common but are of limited clinical significance.
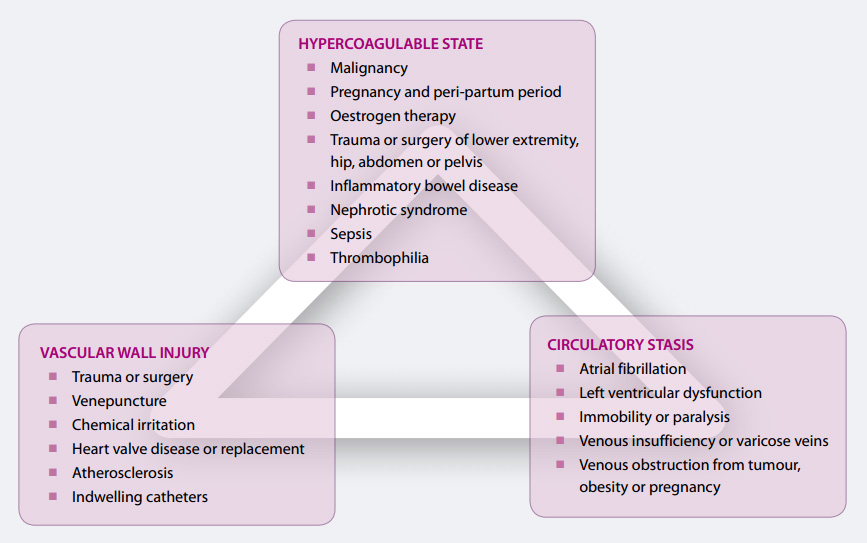
Thrombotic risk is an accumulation of a number of factors. Virchow’s triad demonstrates this risk in terms of physiological
states that promote thrombosis, including; circulatory stasis, hypercoagulability and vascular wall injury (Figure 1).
Predisposing factors or current health status can alter one or more components of this triad. Most patients presenting
with venous thromboembolism (VTE), will have more than one recognised risk factor, with overall risk increasing as the
number of risk factors increase.1 Risk factors for VTE are listed in Table 1.
Figure 1: Virchow’s triad (Adapted from Merli, 2006)2
Clinical assessment of patients at increased thrombotic risk
When a patient presents to primary care with a VTE or a family history of VTE, it is important to perform a thorough
clinical assessment to determine the presence of risk factors (Table 1), and to collect a personal and family medical
history. This assessment can help to determine if the event was provoked, i.e. whether risk was exacerbated by external
risk factors, or unprovoked, i.e. occurred for no apparent reason. The thrombotic load (large or small thrombosis) and
the site (proximal or distal) should also be noted.
| Table 1: Risk factors for VTE1 |
Strong risk factors (odds ratio > 10)
- Fracture (hip or leg)
- Hip or knee replacement
- Major general surgery
- Major trauma
- Spinal cord injury
Moderate risk factors (odds ratio 2–9)
- Arthroscopic knee surgery
- Central venous lines
- Chemotherapy
- Congestive heart or respiratory failure
- Hormone replacement therapy
- Malignancy
- Oral contraceptive therapy
- Paralytic stroke
- Pregnancy/postpartum
- Previous venous thromboembolism
- Inherited thrombophilia
Weak risk factors (odds ratio < 2)
- Bed rest > 3 days
- Immobility due to sitting, e.g. prolonged car or air travel
- Increasing age
- Laparoscopic surgery, e.g. cholecystectomy
- Obesity
- Pregnancy/antepartum
- Varicose veins
|
What is included in a “thrombophilia screen?”
The tests included in a thrombophilia screen generally include:
- Factor V Leiden
- Prothrombin gene mutation
- Antithrombin
- Protein C and Protein S
- A lupus anticoagulant screen will sometimes be included
It is recommended that all requests for thrombophilia tests are first discussed with a haematologist. In addition, requests
should be accompanied by all relevant clinical information. Laboratories may reject the specimen unless there is sufficient
clinical information to justify testing.
The choice of tests will depend on clinical information. For example, antithrombin, Protein C or Protein S deficiency
is more likely in a younger person with a spontaneous VTE, and less likely in an older person with other risk factors
for a VTE.3
Testing principles
Thrombophilia testing should only be performed when the test results will alter management. In most cases management
will be determined by clinical presentation, rather than test results. There is a lack of evidence for indiscriminate
screening,4 and instead it is recommended that careful and selective testing should be done only if the results
would affect the patient’s medical management or provide useful information for the health care of the family.5
Although Factor V Leiden (3–7%) and Prothrombin gene (1–3%) are the most prevalent mutations,6 they only
increase an individual’s risk of a first VTE by approximately five-fold and have little effect on the risk of recurrence
after a first VTE. Antithrombin, Protein C and Protein S are relatively rare mutations, but the presence of these mutations
increases an individual’s risk of a first VTE by approximately ten-fold and risk of recurrence by approximately two-fold.6
There are a number of other markers that may be implicated in increasing risk of VTE, however, they have currently not
been demonstrated to be independent risk factors.7 In addition, it is likely that a number of other yet to
be identified mutations exist.
Who should be tested?
Although there has been increased interest in thrombophilia testing over the last few years, the role of testing for
determining thrombotic risk is likely to have been overstated. Recent guidelines indicate that in most cases thrombophilia
testing will not influence management or determine individual risk.8
Thrombophilia testing is therefore only recommended in specific situations for selected patients where the results will
influence management. These situations include:
- People presenting with unprovoked venous thrombosis at an early age (<40 years), with a family history
of thrombosis (more than two other symptomatic first degree family members). The yield of testing and the significance
of positive results are likely to be increased in this group of patients. However, strong clinical history should be
taken into account when making future decisions such as contraceptive options, pregnancy management and prophylaxis
in high-risk situations, irrespective of the results of thrombophilia testing. Negative results in an individual with
a strong personal or family history of VTE does not necessarily mean that they are at low risk of VTE.
- Children with purpura fulminans. This is a rare condition presenting as a progressive haemorrhagic
skin necrosis. It may be either inherited (as congenital Protein C deficiency) or acquired (Protein S deficiency). All
infants and children with purpua fulminans should be tested urgently for Protein C and S deficiency,8 since
this result will alter management in this situation.
- Pregnant women at risk of venous thrombosis. Pregnant women who have had a previous VTE due to a
minor provoking factor, i.e. a less significant risk factor, or who have a first degree relative with a previous VTE
due to minor provoking factor, should be tested.8 Most pregnant women with a previous unprovoked VTE will be given anticoagulation
treatment based on clinical risk alone, and testing is not required.
Who should not be tested?
Anticoagulation following acute VTE
Thrombophilia testing is not recommended in the acute phase of a thrombotic event, or in patients on anticoagulant treatment.
The intensity and duration of anticoagulation following a diagnosis of VTE is most often initially determined in secondary
care, but it is usually the same in patients with or without an inherited thrombophilia. Decisions regarding duration
of anticoagulation are based on whether the first event was provoked, what other risk factors are present and the risk
of anticoagulation, regardless of whether the patient has an inherited thrombophilia.8
Family history for thrombosis
Factor V Leiden and Prothrombin gene mutation are considered low risk thrombophilias, and case finding in asymptomatic
relatives is not indicated.8
Antithrombin, Protein C and Protein S deficiencies are considered high risk thrombophilias, but testing should only
be considered in thrombosis-prone families after careful explanation of inheritance and disease risk.8
Oestrogen containing hormone preparations and thrombosis
If a patient has a history of VTE, or a current VTE, then oestrogen-containing hormonal preparations should not be prescribed.
If there is a family history of VTE in a first degree relative under 45 years of age, the use of such preparations is
not usually recommended unless other methods are not available or not acceptable.9
For patients with known thrombogenic mutations (e.g. Factor V Leiden, Prothrombin mutation, Protein C, Protein S and
Antithrombin deficiencies) oestrogen containing preparations should be avoided. However routine screening is not appropriate.9
Thrombophilia and flying
VTE is a relatively uncommon event among healthy travellers on long-haul flights, with approximately one event occurring
per 4500 flights. Thrombophilia testing is unhelpful and, instead, risk should be assessed based on the presence of clinical
risk factors.10 Those at particular risk include people with a history of VTE, active cancer or recent surgery,
especially orthopaedic surgery to the lower limbs. It is recommended that air travellers with a high risk of DVT be considered
for prophylaxis with knee-length compression stockings.10
Case studies
Case 1: A well-informed, intelligent 22-year-old female has been on the combined oral contraceptive
(COC) pill since age 18 years. She is a smoker. There is no significant past medical or family history of VTE. She has
read that she is at risk of DVT being on the COC and asks to be tested for thrombophilia. Is testing indicated?
There is no indication to request thrombophilia tests for this patient. There is a slightly increased risk for women
on COC, although the fact that she has been on the COC for more than a year without incident puts her in a lower risk
group as patients with thrombophilia who develop DVT tend to do so in the first year. Any perceived risk would be best
managed by reducing other contributing factors such as obesity, and recommending smoking cessation, if relevant.
Case 2: A 50-year-old male presents prior to a long distance flight. His mother died from a PE two
years ago. He is very worried because he had a spontaneous DVT himself several years ago. He is also obese and has very
bad varicose veins. Is testing indicated?
This patient has a strong personal and family history of VTE and testing is not going to determine management. Prophylaxis
is advisable in view of the patient’s risk factors and the patient’s anxiety about his mother’s death.
Case 3: A healthy 33-year-old female presents in her first pregnancy. She tells you she had previously
had VTE when she flew to England ten years ago. Is testing for hereditary thrombophilia indicated?
Recent clinical guidelines recommend that this patient should have thrombophilia testing.8 Travel is considered
a minor risk factor for VTE, and on its own would be unlikely to contribute to the thrombotic event. Therefore, it is
likely there are other provoking factors present. If clinical assessment does not identify any other contributing factors,
thrombophilia testing would be indicated.
Acute presentation of venous thromboembolism (VTE)
Although patients may present with the classic symptoms of deep vein thrombosis (DVT) or pulmonary embolism (PE), they
can also pose a diagnostic challenge if the classic signs and symptoms are absent. In patients with symptomatic VTE, PE
manifests in one-third and DVT alone in two-thirds.
The most common symptoms of PE are dyspnoea (73%), pleuritic pain (66%) and cough (37%), and the most common signs are
tachypnoea (70%), lung crepitation (51%) and tachycardia (30%).11 Patients with DVT commonly present with pain,
erythema, warmth and swelling of the affected limb.11
The incidence of VTE in the general population is approximately ten cases per 10 000 people, per year. However, this
estimate is dependent on age as there is a significant increase in VTE incidence particularly after age 40 years. The
risk of VTE for a person aged 25–35 years is approximately three cases per 10 000 people, whereas for a person aged in
their 70’s the risk is more than ten times higher than this (30–50 cases per 10 000 people).12
D-dimer can be used to confirm absence of VTE
D-dimer is a fibrin degradation product, and is elevated in nearly all patients with VTE, but can also be elevated in
patients with infection, malignancy or recent surgery. Because of the low specificity of D-dimer for VTE, its key role
is as a negative predictor of VTE, i.e. a low or normal D-dimer level with a low pre-test probability makes VTE an unlikely
diagnosis.
D-dimer can be used in conjunction with the Wells Rule or the Primary Care Rule (Table 2)13 to determine
the probability of a DVT. Historically, the Wells Rule has predominantly been used in New Zealand, but more recently the
Primary Care Rule has become popular. Both rules can be safely used to reduce unnecessary referrals for compression ultrasonography,
although the Primary Care Rule reduces unnecessary referrals slightly more.13
Patients with a high probability of DVT should be referred for ultrasound irrespective of the results of the D-dimer
test. Using this approach, only approximately 0.5% of patients with an initially negative assessment, i.e. a low Clinical
Probability Score and negative D-dimer, are likely to be later diagnosed with DVT.3
Variables
|
Wells Rule |
Primary Care Rule |
Male gender
|
n/a |
1 |
Oral contraceptive use
|
n/a |
1 |
| Presence of active malignancy (within last 6 months) |
1 |
1 |
| Immobilisation paresis/plaster lower extremities |
1 |
n/a |
| Major surgery (within last 3 months) |
1 |
1 |
| Absence of leg trauma |
n/a |
1 |
| Localised tenderness of deep venous system |
1 |
n/a |
| Dilated collateral veins (not varicose) |
1 |
1 |
| Swelling, whole leg |
1 |
n/a |
| Calf swelling > 3 cm |
1 |
2 |
| Pitting oedema confined to the symptomatic leg |
1 |
n/a |
| Previously documented DVT |
1 |
n/a |
| Alternative diagnosis at least as likely as DVT |
-2 |
n/a |
| Positive D-dimer result |
n/a |
6 |
| Cut-off scores for considering DVT as absent |
≤1 |
≤3 |
Differentiating between DVT and SVT
It can sometimes be difficult to differentiate between DVT and superficial vein thrombosis (SVT). SVT or superficial
thrombophlebitis, is often associated with conditions that increase thrombotic risk, e.g. surgery or trauma, immobilisation,
malignancy. A patient with SVT will often present complaining of a painful, red, firm lump in the lower leg. Clinical
examination will usually confirm the diagnosis, but in some cases further investigation may be required as SVT and DVT
can co-exist (because a superficial thrombus can move into the deep veins).
The presence of clot within a vein may be palpable as an indurated (hardened) nodular cord, however in some cases the
clot may only be accurately diagnosed with ultrasound.
DVT should be suspected if:14
-
* When SVT occurs close (within 3 cm) to the sapheno-femoral there is an increased
risk of DVT (+/- PE) therefore treatment should be as for DVT.14,15
The superficial thrombosis is in the upper medial third of the thigh*
- The swelling in the lower leg is more than would be expected with SVT alone
- The SVT is extending
- The diagnosis of SVT is uncertain
- There are risk factors for DVT, e.g. history of DVT, malignancy, oestrogen therapy or thrombophilia
N.B. Clots that occur in the main deep vein of the thigh (“superficial” femoral vein) should be classified and treated
as a DVT as the femoral vein is part of the proximal deep venous system.