Fungal infections of the skin, nails and hair are caused by dermatophytes. In many cases, diagnosis of infection is made by clinical appearance alone, but laboratory examination of skin scrapings, nail cuttings and hair can be requested if the diagnosis is uncertain.
In this article 
View
/ Download pdf version of this article
Fungal infections are caused by dermatophytes
Fungal infections of the skin, nails and hair are caused by dermatophytes, which require keratin for nutrition. The
estimated lifetime risk of acquiring a superficial fungal infection is between 10 – 20%,1 although these are
rarely, if ever, invasive.
Organisms involved in fungal infections
Superficial fungal infections may be caused by one of over forty different species of dermatophytes, belonging to the
following three genera;
- Trichophyton spp – found in hair, nails and skin, transmitted by soil, animals or humans
- Microsporum spp – common cause of scalp ringworm in children, usually transmitted by animals
- Epidermophyton spp – most commonly affects the groin, transmitted from person to person
Fungal infections are named according to the site affected rather than the causative agent (Table 1).
Table 1: Classifications of superficial fungal infections.
2
Classification
|
Affected site |
Notes |
Tinea pedis
“athelete’s foot”
|
Feet |
The most common fungal infection. Initial infection can be dry and scaly, however secondary bacterial
infection and accumulation of soggy debris can commonly occur. |
| Tinea capitis |
Scalp |
More common in children.
Infected hair can break leaving a bald area.
|
| Tinea barbae |
Beard |
Common among men that work with animals, e.g. agricultural workers, due to animal to human transmission.
May be accompanied by bacterial folliculitis, secondary to ingrown hairs.
|
Tinea corporis
“ring worm” |
Skin other than bearded area, scalp, groin, hands or feet |
Tends to present as irregular expanding rings with a raised border.
|
Tinea cruris
“jock itch” |
Groin, perineum and perianal areas |
Lesions may be on the inner thighs, pubic, inguinal region or scrotum. Yeast infections (usually
Candida albicans) are also commonly found in these areas.
|
Tinea manuum
Tinea pedis –
“moccasin-type” |
Hands
Soles of feet |
Can be asymptomatic and is characterised by dryness and increased skin markings. Often only one
hand or one foot is affected.
|
| Tinea unguium |
Nails |
Also known as onychomycosis. Most fungal nail infections are caused by spreading of Tinea pedis.
Toenails are much more commonly affected than fingernails.
|
Investigating fungal infections
Diagnosis of a fungal infection is often made by clinical appearance alone, but sometimes laboratory examination of
skin scrapings, hair or nail cuttings can help when the diagnosis is uncertain.
When do fungal specimens need to be collected?
Minor localised infections can be treated topically without the need for fungal testing.
Specimens should be sent to confirm disease when the infection is chronic, severe or when considering systemic therapy.
Laboratory fungal testing is also justifiable in the following circumstances:3
- To confirm fungal infection before starting on oral treatment, e.g. if the patient has been treating the lesion with
topical steroids or a fungal infection involving the hair, palms of the hands or soles of the feet
- To determine the species of fungus to allow targeted oral treatment
- On epidemiological grounds, e.g. people in contact with an animal in cases of animal ringworm
How to collect a suitable specimens
In most cases, collection of fungal specimens is performed at the laboratory. If this is not possible, or if the clinician
wishes to collect the sample themselves, the following guidance may be helpful.
- Ensure that the patient has not used anti-fungal medications for the previous three days.
- If collection of the specimen is proving difficult, then consider asking the patient to do it themselves, under supervision.
Patients are often more aggressive at getting a good sample than a collector who is trying to be gentle.
Skin scrapings
To optimise skin scraping specimens:
- Prepare the skin for scrapings – remove any traces of skin products or medications with an alcohol wipe
- Scrape the skin using a scalpel (held at a blunt angle)
- Choose the best area to scrape – if multiple lesions are present choose the most recent for scrapings as old loose
scale is often not satisfactory. Ensure that the leading edge of a rash is sampled (this is where fungal growth is most
likely to be active).
- The skin scrapings should then be gently removed from the skin surface and placed into a laboratory specimen container
Quantity is crucial – the greater the amount of specimen, the better the result. If it is difficult to get sufficient
scrapings it may help to ask the patient to stop applying creams and to avoid scrubbing the affected area for a few days
and then try again.
Nail cuttings/scrapings
To optimise nail cuttings/scraping specimens:
- Clean the nail with an alcohol wipe
- Use the blunt end of a lancet or other instrument and firmly scrape under the nail plate until the crumbling white
degenerating portion is reached
- Collect any white keratin debris beneath the nail directly into the specimen container
- Nail clippings should also be collected
Again, quantity is crucial – the greater the amount of specimen, the better the result.
Having the specimen taken should be painless apart from occasional slight discomfort when subungual specimens are taken.
Figure 1 shows the appropriate sites from which nail specimens should be obtained.3
Figure 1: Recommended sites for nail specimens (adapted from Denning et al, 1995).3
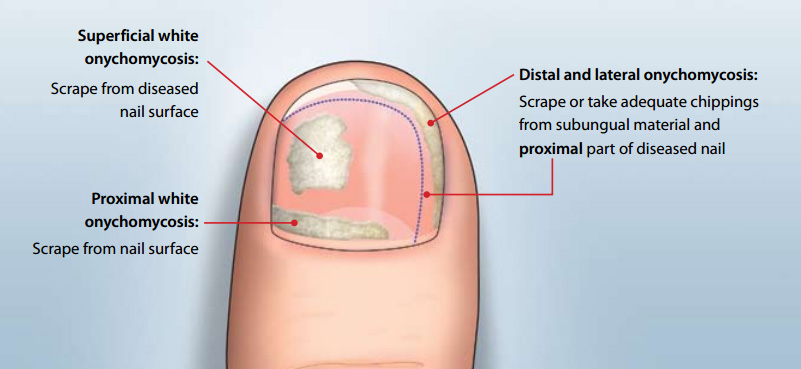
N.B. proximal white onychomycosis is rare and only seen in immunocompromised patients. Full clinical review would be
indicated for a person presenting with these symptoms.
Hair specimens
To optimise hair specimens:
- Pluck hairs from the affected area using tweezers
- Scrape the affected area using a scalpel (held on a blunt angle), on to a piece of paper
- If available, examination of the scalp with a Wood’s lamp can guide the collection of samples from affected areas
Negative results do not necessarily rule out fungal infection
A negative culture result may arise due to:
4,5
- Feature of methodology
- Incorrect initial clinical diagnosis
- Sampling errors associated with poor collection technique
- Sampling errors associated with inadequate specimen
- The presence of non-viable hyphae elements in the distal region of a nail
- An uneven colonisation of a nail with the fungus
- Overgrowth by contaminant saprophytic fungi
- Anti-fungal treatment used prior to collection of the specimen
- A delay in the specimen reaching the laboratory
- Incorrect laboratory procedures
- Slow growth of the organism
Laboratory analysis
At the laboratory, specimens are first examined under the microscope. Fungal elements are sometimes difficult to find,
especially if the tissue is very inflamed, so a negative result does not rule out fungal infection.
A sample is then cultured for approximately three weeks, although most positives are reported after one to two weeks.2 Testing
has a reasonably low level of sensitivity, so a negative result still does not exclude the presence of a fungal infection.
Specimen collection should be repeated after a negative result if fungal infection still appears likely, preferably
prior to treatment.
N.B. Consider a wide differential diagnosis as there are some other explanations for ring-shaped or
scaly rashes, e.g. pityriasis rosea, discoid eczema.
Acknowledgement
Thank you to Dr Rosemary Ikram, Clinical Microbiologist, MedLab South, for expert guidance in developing
this article.
References
- Noble S, Forbes R, Stamm P. Diagnosis and Management of common tinea infections. Am Fam Physician 1998;58(1):163-74,
177-8.
- Kyle C (ed). A handbook for the interpretation of laboratory tests. 4th Ed. Auckland: Diagnostic Medlab; 2008.
- Denning D, Evans E, Kibbler C, et al. Fungal nail disease: a guide to good practice (report of a working group of
the British Society for Medical Mycology). BMJ 1995;311:1277.
- DermNet NZ. Mycology. New Zealand Dermatological Society Inc. Available from:
www.dermnetnz.org/doctors/fungal-infections/mycology.html (Accessed
March, 2011).
- IMVS Pathology. Newsletter Issue 72. Onychomycosis: sample collection made easy. IMVS, Australia, 2009. Available
from:
www.imvs.sa.gov.au (Accessed
March, 2011).