Management of parasomnias consists of identifying and resolving any underlying causes, providing reassurance and advice
on optimal sleeping practices (sleep hygiene), and where necessary, modification of the sleeping environment. In severe
cases, pharmacological treatment may be considered.
Exclusion of underlying causes may include investigation of:3,4
- Use of medicines with CNS-related adverse effects, e.g. sedative hypnotics, SSRIs, beta-blockers and tricyclic antidepressants
- Use of non-pharmacological drugs with CNS-related adverse effects, e.g. caffeine, nicotine, alcohol, illicit drugs
- Anxiety or stress
- Depression or other mental illness
- Dementia or confusion in older people
- Other sleep disorders, e.g. restless leg syndrome, sleep apnoea, narcolepsy
Reassurance that parasomnias are common, usually without any specific cause and generally resolve over time may be helpful.
Household members should be advised that during parasomnia episodes, the person should not be woken as this may increase
disturbance or lead to violent behaviour.3 If they have left their bed, the person should be gently redirected
back to bed without waking, or if there is a history of violence, observed but left alone.
Sleep hygiene is the term used to describe a set of structured practices and habits that can help to maximise the quality
and duration of sleep, and therefore minimise the occurrence of parasomnias. Sleep hygiene advice includes:5
- Go to bed when sleepy, and get up at the same time each day
- Avoid daytime napping (except in young children), especially after 2 pm
- Avoid excessive light exposure prior to bed, e.g. computer screens, cell phones
- Ensure that sleep and sex are the only uses of the bed
- Get regular exercise, ideally mid to late afternoon
- Limit caffeine, alcohol and tobacco intake, particularly at night
- Have a hot drink, e.g. milk, prior to bed
- Avoid doing school-work or work prior to bed
- Get out of bed if sleep onset does not occur within 20 minutes, perform a relaxing activity such as listening to music
or reading for a short time and then return to bed
Making the sleep environment safe may be necessary if the parasomnia behaviour involves leaving the bed. For example,
place locks on second story windows, remove furniture, including mats and electrical cords, from around the bed, secure
dangerous items such as knives or matches and secure exits to prevent wandering.
Scheduled waking may help to reduce the incidence of episodes of non-REM parasomnias such as somnambulism (sleep walking).
The patient is gently and briefly woken 15 - 30 minutes prior to the normal episode time.5,6 The procedure
is repeated nightly for up to one month, and then a trial without waking is done to assess whether there is a continued
response.
Pharmacological treatment (Table 1) may be considered when parasomnias become frequent, cause extreme anxiety or there
is potential for harm to the person or household members. The use of medicines to treat parasomnias is complex and rarely
evidence based.4 There are no medicines currently approved for use for parasomnias in New Zealand. Medicine
should only be prescribed after exclusion of reversible underlying causes and all non-pharmacological options have been
trialled.6 Pharmacological treatment is rarely recommended for children with parasomnias, and at present, the
evidence is limited.5 Where pharmacological treatment is considered for a child, it should be discussed first
with a paediatrician, sleep physician or psychiatrist.
Psychotherapy, particularly relaxation and cognitive behaviour therapy, where available, may be useful for some people
with parasomnias.6
Referral to a sleep physician is recommended if treatment is ineffective, the risk of harm is significant, the symptoms
are atypical or the diagnosis is unclear.
The architecture of sleep
Sleep occurs in a complex cycle, which is essential for physiological regulation, function and overall health. An individual's
sleep architecture, i.e. the structure and pattern of their sleep, can have a significant effect on their quality of
life, day-time function and health.
The 24-hour sleep cycle is divided into three broad stages; non-rapid eye movement (non-REM), rapid eye movement (REM)
and wakefulness. Sleep duration is the total time in a 24 hour period that a person sleeps, and is divided into non-REM
and REM sleep stages (Figure 1). Non-REM sleep is further divided into stages, with "deepest" sleep occurring in Stage
Four.
Quality of sleep is dependent on sleep duration, along with time of sleep onset and length of time spent in each stage
of sleep.
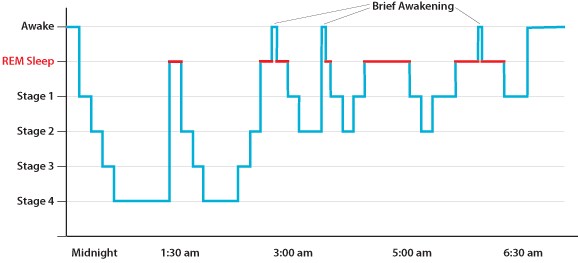
Figure 1: Human sleep architecture, showing deep sleep (Stage 4) early in the night and multiple
REM stages |