In this article 
View / Download
pdf version of this article
Practical tips and information for prescribing statins
Statins are one of the most frequently prescribed medicines in New Zealand each year (Table
1). Alongside lifestyle modifications, statins are the mainstay of lipid management. New Zealand and international
guidelines recommend statins for the primary prevention of cardiovascular disease.
Liver dysfunction and muscle problems such as pain (myalgia) and weakness can be experienced by up
to 10% of patients taking statins. However, myalgia is commonly experienced by all people at some stage in their life,
regardless of statin use. Risk factors for statin-associated myalgia include pre-existing muscle, liver
or kidney disease, high-dose statin treatment, concomitant interacting medicines, intercurrent illness, frailty and advanced
age.
It is no longer considered necessary to routinely monitor liver (alanine aminotransferase [ALT]) and
muscle (creatine kinase [CK]) biochemistry unless the patient has specific risk factors or develops symptoms or signs
of liver dysfunction or muscle problems.
When should lipid-modifying treatment be stopped or the dose reduced?
- Statins should be used with caution in patients with ALT more than three times normal levels
- Either a statin dose reduction or discontinuation should be considered if CK is between three to ten times the normal
level
- Statins should be discontinued immediately if CK is more than ten times the normal level
- Patients with persistent unexplained muscle pain may require a dose reduction or discontinuation
Statin Use in New Zealand
Statins are commonly used medicines in New Zealand, with approximately 16% of the adult population (≥18 years
of age) dispensed a statin in the last 12 months (Table 1).
Table 1: Number of registered patients dispensed any statin in New Zealand and in your
practice between Jul 2013 – Jun 2014
| |
National |
Sample Practice |
| Medicine Name |
Number of patients |
% of population |
Number of patients |
% of population |
| Atorvastatin |
284,262 |
8.9% |
470 |
4.7% |
| Simvastatin |
226,984 |
7.1% |
929 |
9.2% |
| Pravastatin |
12,626 |
0.4% |
9 |
0.1% |
| Ezetimibe with Simvastatin |
1,900 |
0.1% |
9 |
0.1% |
| TOTAL |
525,772 |
16.5% |
1,417 |
14.0% |
Doses of simvastatin over 40 mg should only be considered for patients who have not achieved treatment goals at lower
doses, as these doses only produce a slight additional reduction in LDL but greatly increase the risk of myopathy.2 In
patients taking 80 mg simvastatin, consider switching to atorvastatin 40 mg daily, which is an equivalent dose. In addition,
consider that the benefits of statin treatment for elderly people are less clear than in younger populations, therefore
older patients may benefit more from a reduction in dose. Table 2 shows the proportion of all statin patients who are
taking high-dose simvastatin, nationally and for your practice, this dose increases myopathy risk.1,2
Table 2: The number of patients dispensed high-dose simvastatin in New Zealand and in your
practice between Jul 2013 – Jun 2014
| |
National |
Sample Practice |
| Medicine Name |
Number of patients |
% of population |
Number of patients |
% of population |
| Simvastatin 80mg |
8,636 |
1.6% |
17 |
1.2% |
Monitoring statin safety is not routinely required
Baseline testing of muscle enzymes prior to statin treatment is unnecessary unless the patient has risk factors. Once
treatment has started, monitoring of alanine aminotransferase (ALT) or creatine kinase (CK) is unnecessary unless clinically
indicated i.e. the patient is symptomatic or has specific risk factors. Figure 1 below shows that nationally these guidelines
are being followed with a reduction in testing over the last three years. Between Jul 2013 – Jun 2014, 5.5% of
patients dispensed a statin had a CK test and 3% an ALT test.
Sample Practice |
National |
Between Jul 2013 – Jun 2014 for the patients registered to Sample Medical who were
dispensed a statin*
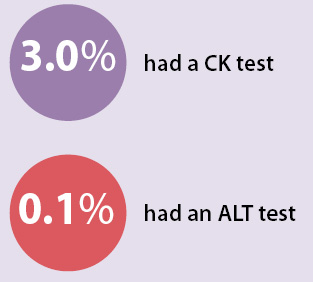
|
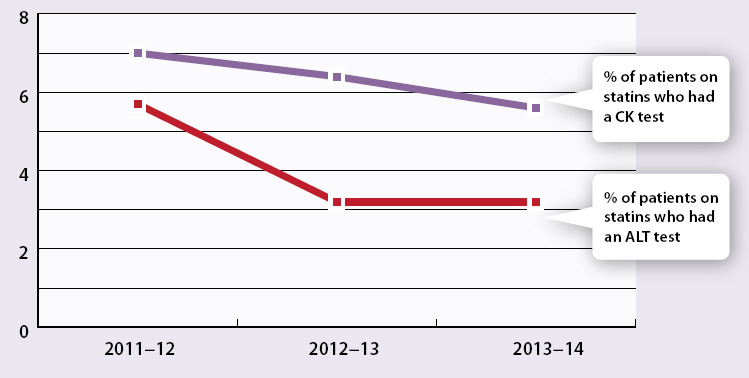
Figure 1: The percentage of patients in New Zealand who were dispensed a statin and received monitoring tests between
2011/12 – 2013/14 |
- 1. Best Tests, August 2014. Available at www.bpac.org.nz (Accessed Oct, 2014).
- 2. New Zealand Formulary 2014. Available at www.nzf.org.nz/nzf_1618 (Accessed Oct, 2014).
- * These tests may have been ordered by someone at your practice or by other health practitioners