In this article 
View
/ Download pdf version of this article
Key messages
- PSA is present in the benign and malignant prostate
- There is currently no national screening programme for prostate cancer in New Zealand
- It is recommended that every man has the right to decide for himself whether or not to be tested, guided by health
professionals providing adequate information
- There is no PSA level below which a man can be completely reassured he does not have prostate cancer. A significant
number of men with prostate cancer will have a normal PSA
- The use of the PSA test for screening asymptomatic men for prostate cancer remains controversial
Prostate specific antigen (PSA) is a glycoprotein produced by the prostate gland, responsible for liquefying seminal
fluid. PSA is usually present in small quantities in serum. Changes to the prostate from normal and non-cancerous conditions
as well as prostate cancer, can lead to increased levels of PSA in the blood stream (see sidebar: “Non-cancerous
causes of elevated PSA”).
Prostate cancer is the most commonly diagnosed cancer in New Zealand men, and is the third highest cause of male cancer
deaths. The lifetime risk of death from prostate cancer is about 3%.1 Approximately 2,500 new cases of prostate
cancer are detected each year, and almost 600 men die per year of prostate cancer (this is similar to the number of deaths
due to breast cancer in women). The registration rate for prostate cancer for Maori males is lower than for the non-Maori
population, but the mortality rate for Maori males is higher.2
PSA testing in New Zealand
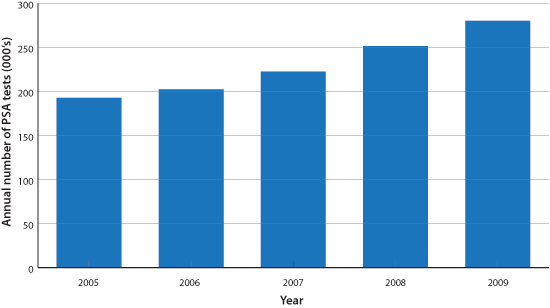
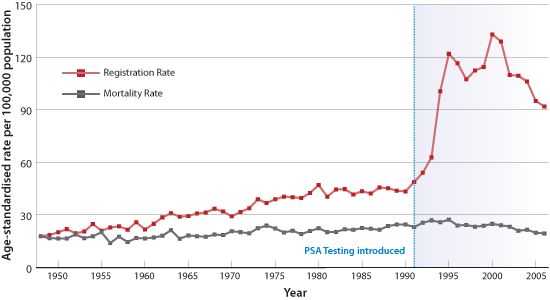
PSA testing has been available in New Zealand since 1991. The number of PSA tests performed has increased almost 50%
over the last five years (Figure 1). Not surprisingly prostate cancer registrations in New Zealand increased dramatically,
over this time, in line with many other developed countries. However, the number of registrations has declined over recent
years. The New Zealand mortality rate, due to prostate cancer, has remained static for approximately 50 years (Figure
2).3
| Figure 1: Annual totals for PSA tests requested by GPs in New Zealand7 |
 |
| Figure 2: New Zealand prostate cancer registration and mortality rates3 |
 |
The GPs role
GPs are the “gate-keepers” for PSA testing – they influence who does and doesn’t get tested.
It is currently recommended by NZGG4 that every man has the right to decide for himself whether or not to be
tested. This decision making is to be guided by doctors and other practitioners who have a duty under the Code for Health
and Disability Services Consumers’ Rights Regulations 1996,5 to provide good, balanced information on
prostate cancer and the possible benefits and harms of testing and treatment.4
Screening for prostate cancer
Prostate cancer screening in asymptomatic men is a controversial public health issue generating much debate with polarised
views around the appropriate use of PSA, both internationally and within New Zealand.
Currently in New Zealand, a national screening programme has not been recommended, as there is a lack of consensus as
to whether the benefit of screening outweighs the harms. The issue of prostate cancer screening is currently being considered
by a Parliamentary Health Select Committee.6
Despite New Zealand not having a formal screening programme for prostate cancer, PSA testing is already widely used
in primary care. In 2009, for example, GPs performed on average 74 PSA tests each per year.7
Approaches to testing
At present, NZGG does not support population screening with PSA for asymptomatic men, but they do recommend GPs advise
patients of the risks and benefits of testing, as well as the likelihood of them developing prostate cancer.
The Urological Society of Australia and New Zealand (USANZ)8 however, encourages all men who are interested
in their prostate health to have a single PSA test and digital rectal exam (DRE) performed at, or beyond, age 40 years.
What is the risk of developing prostate cancer4
Age
Risk of prostate cancer increases with age.
| What is the chance of diagnosis/death for prostate cancer? |
|
Diagnosis |
Death |
| For a man in his 40s |
1 in 500 men |
< 1 in 1000 men |
| For a man in his 50s |
1 in 50 men |
1 in 1000 men |
| For a man in his 60s |
1 in 14 men |
1 in 67 men |
| For a man in his 70s |
1 in 9 men |
1 in 43 men |
Family history
Risk of diagnosis increases with a positive family history. The risk is higher if a close relative is diagnosed before
65 years, or more than one close relative is affected.
| ONE relative (father, brother) diagnosed |
Risk is about 2 and a half times higher |
| TWO relatives (father, brothers) diagnosed |
Risk is about 4 to 5 times higher |
Interpreting PSA results
Results and laboratory terms
PSA results: Normal levels usually range from 0 to 4 μg/L, although age-specific values (upper limit of normal) are
frequently reported as follows:
Non-cancerous causes of elevated PSA1,9
- Daily biological/ laboratory variability of PSA
- Benign prostatic enlargement
- Urinary infection
- Urinary retention
- Prostatitis or sub-clinical prostate inflammation
- Ejaculation
- Digital rectal exam (DRE)
- Prostatic massage
|
- 40 – 49 years 2.5 μg/L
- 50 – 59 years 3.5 μg/L
- 60 – 69 years 4.5 μg/L
- 70 – 79 years 6.5 μg/L
PSA results between 4 and 10 μg/L are considered mildly to moderately elevated, while levels over 10 are considered
high.
The higher the PSA, the more likely the presence of prostate cancer. However, there is no PSA level that below which
a man can be reassured he definitely does not have prostate cancer.
As there are a number of non-cancerous contributors to an increased PSA (see side bar), it is generally prudent to repeat
any initial high result. Care should be taken when interpreting trends, particularly being careful not to over interpret
small changes.9
Effect of ejaculation and DRE have historically been thought to increase the PSA level temporarily. This effect is variable
and in most patients insignificant (about 5% rise over several days for DRE). While PSA can usually be performed after
DRE, it is probably better, if practical, to either collect the PSA sample beforehand or delay collection for up to a
week.1
If there is concern at the current level of PSA, or an increase of the PSA level, referral to a specialist is recommended.1,10
The European Randomised Study of Screening for Prostate cancer (ERSPC)11 was
designed to evaluate the effect of screening with PSA on mortality from prostate cancer. The study took place between
1997 and 2006, and involved 162,387 men, aged 55 – 69 years. Men were randomly assigned either 4 yearly screening
or not offered PSA testing. During a mean follow-up of 9 years, fewer prostate cancer–related deaths occurred
in the screened group than in the control group. |
The Prostate, Lung, Colon and Ovary trial (PLCO)12 was also designed
to evaluate the effect of annual PSA and DRE on mortality rate from prostate cancer. This study included 76,693 men
(aged 55 to 74 years). Men were randomly assigned to either annual screening (annual PSA for 6 years and annual DRE
for 4 years) or usual care (from GP). During 10 years of follow-up, researchers found no difference in prostate cancer–related
deaths (roughly 85 in each group). |
More good than harm?
There has been much controversy around prostate screening both in New Zealand and internationally. There remains a lack
of consensus as to whether the benefits of detecting early disease by screening asymptomatic men outweigh the potential
harms.
Recent trial data
It was anticipated that the long awaited results from two randomised trials (see sidebar opposite) would tell us, once
and for all, whether PSA screening is beneficial. Unfortunately, there is lack of agreement on the interpretation of the
results, leading to continued debate about the use of PSA testing for screening.
Both studies have been criticised for a number of reasons:
Significant contamination of the control group: The PLCO trial was performed in the USA, which has
a high level of PSA testing performed by GPs in usual day-to-day practice. As a result about 38% of the control patients
had PSA testing and 44% had been tested before entry into the study. Therefore, it could be considered this was not a
trial of screening versus no screening, but rather screening versus some screening. There was also some contamination
of the ERSPC trial, but it was less than the PLCO trial and the trial was designed to cope with a contamination rate of
20%.
Short follow-up time: Prostate cancer is usually a slowly progressing condition, therefore the effect
on the mortality rate may not be clear for several more years. At this stage, some believe the reported reduction in mortality
is negligible, while others are surprised it is so high already, considering prostate cancer predominantly progresses
slowly.13
Over-detection and over-treatment
One of the arguments against PSA screening is that it leads to over-diagnosis of prostate cancer (i.e. would not have
been detected, was it not for screening). It is suggested that over-diagnosis leads to over-treatment. It has been estimated
that at age 55 years, PSA testing results in an over detection rate of 27%, by age 75, this is estimated to be 56%.1
Most men with an elevated PSA will proceed to biopsy. One in four prostate biopsies will find prostate cancer,1 while
the risk of significant bleeding or infection is 1 to 4% of patients. For those diagnosed with prostate cancer, approximately
90% will elect to have some sort of intervention. This includes surgery, radiation therapy, or androgen deprivation. All
of these treatments may be associated with adverse effects, such as urinary, bowel and erectile dysfunction.
Many patients may consider the adverse effects to be acceptable trade-offs for a procedure they regard as “life
saving”. There is also the argument, that any morbidity associated with intervention, is better than the morbidity
from metastasised prostate cancer.
Others argue that up to 50% of the prostate cancers detected would not have caused illness in the man’s lifetime.14 Therefore,
for 50% of men any adverse effects from any intervention can be considered a harm.
Acknowledgement
Thanks to Professor Brett Delahunt, Pathology and Molecular Medicine, Wellington School of Medicine,
Wellington, for his expert guidance in developing this article.
References
- Greene KL, Albertsen PC, Richard J. Babaian RJ, et al. Prostate Specific Antigen Best Practice Statement: 2009 Update.
J Urol 2009;182(5):2232-2241. Available from: http://www.jurology.com/article/S0022-5347(09)01955-7/fulltext
- New Zealand Health information service. Cancer: New registrations and deaths 2004. Available from http://www.nzhis.govt.nz/moh.nsf/pagesns/500/$File/Cancer04.pdf
- Cancer Society. Submission To Health Select Committee: Early Detection and Treatment of Prostate Cancer. Available
from : http://www.cancernz.org.nz/
- New Zealand Guidelines Group. Testing for prostate cancer: a consultation resource. Wellington: New Zealand Guidelines
Group, 2008. Available from: http://www.moh.govt.nz/
- Health and Disability Commissioner (Code of Health and Disability Services Consumers’ Rights) Regulations 1996.
Available from: http://www.legislation.govt.nz/regulation/public/1996/0078/latest/DLM209080.html
- New Zealand Parliament. Select committee business summary: Inquiry into early detection and treatment of prostate
cancer. Available from: http://www.parliament.nz/
- Best Practice Advocacy Centre (BPAC). Annual Pharmaceutical & Laboratory Report 2009.
- The Urologoical Society of Australia and New Zealand (USANZ). Media release 15 March 2010. Urologists reassure Australian
men PSA test is best indicator for prostate cancer. Available from: http://www.usanz.org.au/
- Kyle C (Ed), A Handbook for the Interpretation of Laboratory tests. 4th Edition, 2008, Diagnostic Medlab
- D’Amico AV et al. Preoperative PSA velocity and the risk of death from prostate cancer after radical prostatectomy.
N Engl J Med 2004; 351: 125-135.
- Schröder FH, Hugosson J, Roobol MJ, et al. Screening and prostate-cancer mortality in a randomized European
study. N Engl J Med 2009;360:1320-1328.
- Andriole GL, Crawford ED, Grubb RL III, et al. Mortality results from a randomized prostate-cancer screening trial.
N Engl J Med 2009;360:1310-1319.
- Lamb DS, Belahunt B, Denham J, Slaney D. Letter: Survival benefit confirmed for prostate cancers diagnosed by PSA
testing. N Z Med J 2009;122,67-70. Available from: http://www.nzma.org.nz/
- New Zealnd Parliament. Health Select Committee. Submission on the early detection and treatment of prostate cancer.
August 2009. Available from: http://www.parliament.nz/