Module 3: Early surgical abortion theory
5. The early surgical abortion by aspiration procedure
For another video explaining early surgical abortion, click here.
New Zealand Aotearoa Abortion Clinical Guideline 2021:
- Recommendation 3.1.3: “Perform a pre-procedure bimanual examination.”
- Recommendation 3.1.2: “Venous access should be in place prior to the procedure taking place.”
- Recommendation 3.4.2: “Consider using intra-procedure ultrasonography to aid in:
- visualising instruments
- locating fetal parts
- verifying an empty uterus
- reducing the risk of uterine perforation
- shortening the procedure.”
Follow all principles of informed consent at all times, including if requested having a karakia performed prior to and after the procedure. Consent must be in writing if the early surgical abortion is performed under general anaesthetic.
1. Before the procedure
Check that all the necessary equipment is available and sterile and that all necessary staff and support people are present. Ensure you have clean gloves and appropriate personal protective equipment (PPE). Perform a suitable pre procedure checklist including antibiotic prophylaxis, contraception and anti-D plans and perform or facilitate a karakia if this has been planned. Administer oral analgesics and medicine for cervical priming.
2. Bimanual examination
Make sure the person is optimally positioned and covered on a bed with their legs supported and able to relax their pelvic muscles and that venous access is in place.
A bimanual examination must be performed, to assess the uterine size and position and correlate this to the preprocedural estimated gestation. Note that the presence of fibroids or other anomalies may affect this. If the findings suggest a difference of gestation to that expected, then a point of care ultrasound may be used to confirm gestation. If the uterus is estimated to be a greater size than first trimester and point of care ultrasound is not available to confirm the gestational age, then stop the procedure until gestation can be confirmed.
The uterine position and the estimated direction of the cervical canal must be noted.
If there is cervical motion tenderness reconsider your antibiotic management to include treatment of pelvic inflammatory disease and note not to insert an intrauterine contraceptive (IUC) if this was planned. Consider the possibility of an ectopic pregnancy.
3. Cervical cleansing and paracervical block procedure
Insert a speculum gently and open to visualise the cervix. Cleanse the cervix with an antiseptic solution (consider allergies). Warming the solution may improve the person’s comfort. An early surgical abortion using aspiration is a no touch aseptic procedure; as the vagina is not made sterile prior to the procedure it is important not to touch the vagina when placing the dilators and canulae into the cervical canal.
Insert 2 mL of local anaesthetic at 12 o’clock (or at six o’clock in a severely retroverted uterus) and place a tenaculum. Perform a paracervical block if indicated.
4. Cannula placement and cervical dilatation
Cannula come in two varieties: flexible or rigid (Figure 7). MVA cannula are available from ISTAR. They are sized by diameter, and most clinicians choose a diameter equal to the number of weeks gestation or one size smaller.
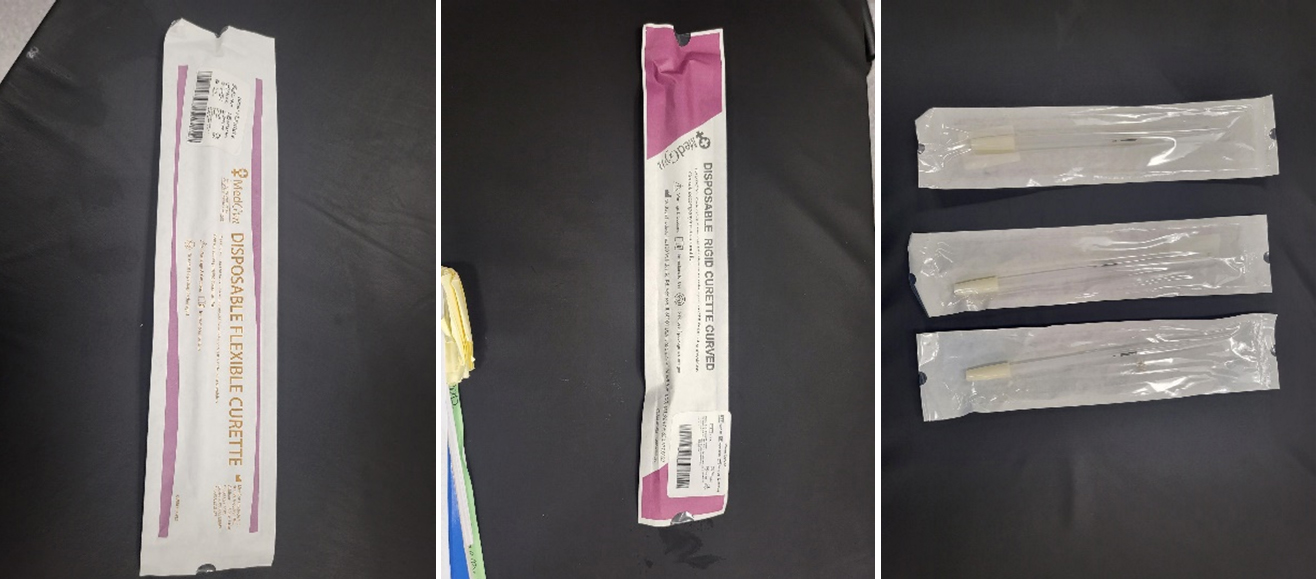
Figure 7. MedGyn cannula. From left to right, the images depict flexible packaging, rigid packaging, and three individual curettes in packaging.
If the os is already open to allow the size of the cannula required to enter there is no need to perform additional dilatation.
Pull with gentle traction on the tenaculum to straighten the cervical uterine angle, before trying to pass the cannula through the os and advance it to the fundus. DO NOT USE A UTERINE SOUND IN A PREGNANT UTERUS.
If the canula does not pass through the internal os you will need to dilate the cervix.
There are a number of cervical dilators: Hawkin-ambler dilators (Figure 8A) are tapered and create progressive dilation; double ended dilators (Figure 8B) must be held in the middle to achieve a no touch technique. Slowly increase the dilation up to that required to pass the canula, ensure you know the correlation between the size of your dilators and your cannula. The aim is to dilate the internal os; you do not need to pass the dilator into the upper uterine cavity. It is important to follow the cervical canal and not create a false passage, this is done by not forcing the dilator. If there is a difficulty with dilation, then consider: dilating the external os first especially if you do not have Pratt dilators; using an os finder; using ultrasound to assist; stopping the procedure and giving more time or an alternative cervical priming preparation.
| A |
B |

Figure 8. A) Hawkin-ambler dilators
|
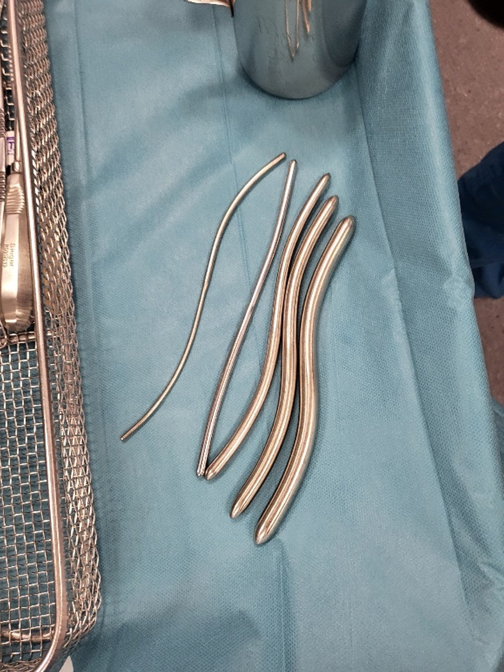
Figure 8. B) Double-ended dilators (which are held at the midpoint)
|
5. Aspiration of uterine contents
Once the cannula of the appropriate size passes through the internal os and is located at the fundus the cannula suction can be applied with either the MVA or the EVA tubing.
You must be familiar with the MVA or EVA equipment you are using before commencing abortion training. We recommend that you arrange a PAPAYA workshop with your supervisor to become comfortable with the equipment you will be using in your environment. To review the skills health practitioners need to demonstrate, and the training required to provide culturally safe, consistent, high-quality early surgical abortion care, click here
Once the vacuum is activated, the cannula is manoeuvred in the uterus with a combination of rotation and in and out movements between the fundus and internal os. Avoid suction movement along the endocervical canal.
When the syringe fills or tissue stops entering the syringe or tubing, remove the cannula to empty the syringe and reactivate the suction. Earlier gestations ≤ 8 weeks have less tissue and may only require one pass. You can leave the cannula in the uterus whilst emptying the MVA. Sometimes a small amount of tissue can block suction by clogging the cannula opening. Often this tissue is a gestational sac. A sterile gauze or forceps can be used to wipe the cannula clean keeping the tissue for evaluation.
Ensure you keep the end of the cannula sterile.
Once the uterus is empty, you will feel a gritty texture when moving the cannula, along with the feeling that the uterus is contracting resulting in the cannula becoming harder to move. It may become more uncomfortable for the person at this time. Avoid unnecessary passes with the cannula once you think the cavity is empty. If you use point of care ultrasound it may be used at this time to confirm the cavity is empty.
If the texture feels smooth, it may be that the uterus is not yet empty or that the cannula is clogged. In this circumstance it is important to look at the end of the cannula to remove possible clogging. You may need forceps to remove this.
Once the aspiration is felt to be complete turn off the suction before removing the cannula, this avoids a sucking sound that can be distressing for people. Remove the tenaculum and examine the cervix for bleeding and trauma. A small amount of bleeding at the tenaculum site is normal and usually resolves with pressure, either bimanual or it can be compressed with sponge forceps.
Before finishing check your plan for antibiotic prophylaxis, contraception and anti-D and perform or facilitate a karakia if this has been planned.
All people having an abortion should be offered contraception and this should have been planned during the consultation and decision-making process. All long-acting reversible contraceptives (LARCs) can be fitted at the time of the early surgical abortion except intrauterine pregnancy (IUC) in the situation of active intrauterine infection. There is a reported increase in expulsion with IUC insertion at the time of an abortion; this is within acceptable limits to recommend not delaying insertion. Medroxyprogesterone acetate (Depo-Provera) injection can be given immediately and Combined Oral Contraceptive Pill (COCP)/Progesterone-only Contraceptive Pill (POP) should be started within 5 days of the procedure (ideally the next day).
6. Ensure that the abortion is complete
New Zealand Aotearoa Abortion Clinical Guideline 2021 recommendation 3.1.4 states “Ensure that every abortion is complete. This can be done by clinical assessment of the uterus, visual inspection of products of conception or ultrasound scan.
- If the gestation is < 7 weeks, visually inspect the aspirated tissue; if there is doubt that the gestational sac and chorionic villi are clearly visualised, ensure follow-up with serum β-hCG or ultrasound scan to exclude ongoing pregnancy or ectopic pregnancy.”
You can ensure the abortion is complete in a number of ways:
- By use of point of care ultrasound confirming the gestational sac has been evacuated
- By clinical assessment of the uterus, with visual inspection of the aspirated tissue under 7 weeks
- It may be necessary in early gestations < 7 weeks to perform a serum β-hCG follow up especially if no gestational sac was seen on ultrasound prior to the procedure i.e. there was a pregnancy of unknown location (for further information, click here)
Visual inspection of the tissue is done by floating the evacuated tissue in saline in a clear dish over a light box (Figure 9).
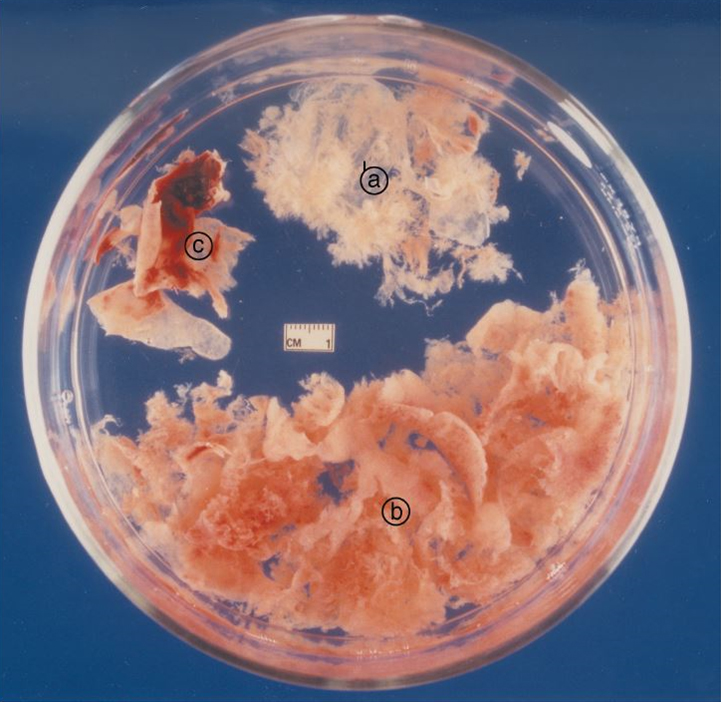
Figure 9. Products of conception aspirated from an 8-week gestation pregnancy. A) thin gestational sac tissue with villi, B) heavier, reddish-brown or grey decidual tissue and C) decidua capsularis, an opaque sheet with haemorrhagic areas.
Treat all products of conception with respect and ensure that for those people who have requested it that their tissue is returned to them. Ideally, we would have culturally safe waterproof containers that decompose when returned to the ground available for the products of conception. It is critical to use a suitable container and to ensure that people know what to expect if they look inside. DO NOT USE FOOD CONTAINERS. Sometimes people will change their mind and ask to have tissue returned after the procedure – be prepared and label all tissue in a confidential and secure manner.
7. Report the abortion
To comply with the Contraception, Sterilisation, and Abortion Act 1977 abortion service providers must submit a notification to the Ministry of Health within one month of an abortion. The Ministry of Health collates the national data on abortions and uses this to report on issues such as timely and equitable access to abortion services.
There is a guide provided on the Ministry of Health Abortion reporting webpage to completing and submitting the notification report, via an online form. A PDF version of the form is also available on request.
