Module 3: Early surgical abortion theory
3. Support staff, equipment and medicines used in early surgical abortion
Support staff requirements
At least one other qualified health practitioner is required to work alongside the main abortion provider to assist them in providing the abortion. There also needs to be a separate qualified health practitioner to manage the sedation and the airway during an early surgical abortion.
Equipment requirements
In general, the equipment required to perform an early surgical abortion includes:
- An appropriate bed with leg supports
- An appropriate covering/drape for the person
- Speculum – The optimal type is person, operator and equipment dependant

- Tenaculum

- Ringed forceps

- Sterile gauze (e.g. 4 × 4’s) with radio-opaque strip

- Betadine or chlorhexidine without alcohol
- Anaesthetic (e.g. 10 – 20 mL of 1% lidocaine; optional to dilute with NaCl or add sodium bicarbonate)
- 22g 1 ½″ or longer needle to attach to syringe or 21g spinal needle with taper tip

- Syringe for local anaesthetic
- Manual vacuum aspirator (MVA)*
 or electric vacuum aspirator (EVA)†
or electric vacuum aspirator (EVA)†
- Range of dilators (multiple sizes above and below gestational age)

- Cannulae (multiple sizes above and below gestational age)

- Forceps for removing tissue obstructing canula

- Correct sized tubing (if using EVA) or MVA
- Strainer (optional)
- Dish to collect and examine products of conception in (if not using point of care ultrasound)
- An appropriate light source
Note: Some of the items in this list are present in the equipment trays in Figure 1 (circled numbers in list correspond to numbered items in panel A). Additional equipment examples are depicted in Figures 2 – 5.
*MVA are recommended for use in patients up to 12 weeks gestation in Aotearoa and are available from ISTAR Ltd. A product description for the Ipas MVA Plus® Aspirator is linked here.
†For gestations over 12 weeks there is a larger suction tube size required for EVA. Surgical abortions > 14 weeks are performed via dilatation and evacuation which is a different procedure to early surgical abortion with aspiration.
| A |
B |
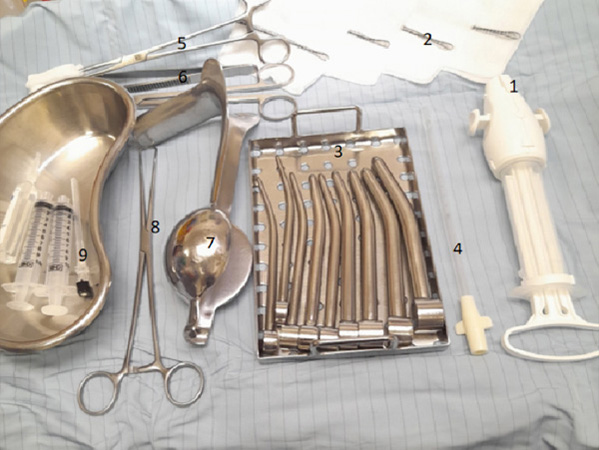 |
 |
Figure 1. Equipment used for early surgical abortion using manual vacuum aspiration.

Figure 2. Tubing Medline product TB29494CE.
Figure 3. MedGyn disposable collection set half inch packaging.

Figure 4. Hawkin-ambler single ended tapered dilator.
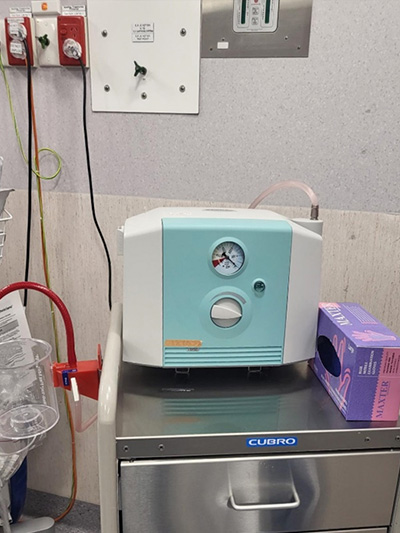
Figure 5. Versa brand EVA machine
In addition to the equipment listed above, appropriate equipment to manage safe analgesia/sedation should be available as per the Australian and New Zealand College of Anaesthetists & Faculty of Pain Medicine (ANZCA) PS09(G) guidelines.
Medicines used in early surgical abortion
Antibiotic prophylaxis
New Zealand Aotearoa Abortion Clinical Guideline 2021, recommendation 3.1.5 states: “Recommend routine antibiotic prophylaxis to reduce the risk of post-abortion upper genital tract infection”
Recommendation 3.1.6 is “Consider metronidazole 1 g per rectum at end of procedure for antibiotic prophylaxis. Alternatively, consider oral doxycycline 100 mg twice a day for 3 days for antibiotic prophylaxis. Do not routinely offer metronidazole in combination with another broad-spectrum antibiotic such as doxycycline.”
There is strong evidence that antibiotic prophylaxis reduces the risk of upper genital tract infection following an early surgical abortion (for further information see this 2019 NICE evidence review and this 2012 Cochrane review). The New Zealand Aotearoa Abortion Clinical Guideline 2021 suggests 1 g of metronidazole should be given rectally immediately following the early surgical abortion. Metronidazole is a more effective treatment for a broader range of infections than doxycycline or azithromycin and is effective against anaerobic bacteria. An alternative (but not additional) recommended prophylactic treatment is to prescribe a short course of oral doxycycline (100 mg, twice daily, for three days) to be started immediately following the abortion.
Anti-D prophylaxis
New Zealand Aotearoa Abortion Clinical Guideline 2021:
- Recommendation 1.3.6: “Recommend testing of rhesus status for people having medical abortion > 10 weeks’ gestation, or surgical abortion at any stage of pregnancy.”
- Recommendation 5.1.2: “Consider anti-D prophylaxis for people who are rhesus D negative and are having a surgical abortion up to and including 10+0 weeks’ gestation.”
- Recommendation 5.1.3: “Offer anti-D prophylaxis to people who are rhesus D negative and are having a medical or surgical abortion after 10+0 weeks’ gestation.”
- Recommendation 5.1.4: “Anti-D prophylaxis supply should not cause delay to providing timely abortion care.”
Administering anti-D immunoglobulins to rhesus D negative pregnant patients can lower their risk of becoming sensitised to the rhesus D antigen if it is passed into their bloodstream from a rhesus positive fetus, embryo or baby. In subsequent pregnancies this could result in haemolytic disease of the newborn, where parental immunoglobulins crossing the placenta can target the rhesus D positive erythrocytes. However, there is no high-quality evidence surrounding the use of anti-D prophylaxis for early surgical abortion under 10 weeks of pregnancy. The New Zealand Aotearoa Abortion Clinical Guideline 2021 recommends testing rhesus status for people having an early surgical abortion and offering anti-D prophylaxis to rhesus D negative patients after ten weeks gestation. In gestations under ten weeks, health practitioners should consider offering anti-D treatment to rhesus negative patients having an early surgical abortion.
Pain relief – analgesia, anaesthetic and sedation
For a video discussing pain during early surgical abortion, click here
New Zealand Aotearoa Abortion Clinical Guideline 2021:
- Recommendation 3.5.1: “Recommend pre-operative analgesia with non-steroidal anti-inflammatory drugs (NSAIDs).”
- Recommendation 3.5.2: “For people who are having surgical abortion, consider local anaesthesia alone, procedural sedation with local anaesthesia, deep sedation or general anaesthesia.”
- Recommendation 3.5.3: “When using procedural sedation for a surgical abortion, use intravenous rather than oral sedation.”
- Recommendation 3.5.4: “Offer supportive methods to reduce pain and anxiety, including empathetic staff, gentle technique, music and verbal reassurance.”
- Recommendation 3.5.5: “When using general anaesthesia for a surgical abortion, consider intravenous propofol and a short-acting opioid (such as fentanyl) rather than inhalational anaesthesia.”
There are three main options for providing pain relief during an early surgical abortion:
- Local anaesthetic (paracervical block) and simple analgesics - non-steroidal anti-inflammatory drugs (NSAIDs)
- Procedural sedation (see ANZCA PS09(G) Guidelines 2014, definition 1.1 ) with local anaesthesia (paracervical block) and NSAIDs
- Deep sedation (see ANZCA PS09(G) Guidelines 2014, definition 1.2 ) or general anaesthesia and NSAIDs
Ideally, the choice of analgesia/sedation/anaesthesia will be up to the person seeking abortion care. However, it is common that the skill of the practitioners or the capacity of the facility impacts on this choice. If a provider is unable to offer the person’s preferred care choice, it is critical that they offer to refer them to another service to access this care. Examples of people who may request or require an early surgical abortion under general anaesthetic can include tamariki/young people under 15 years seeking abortion care and people with a history of sexual assault. In reality, many people seeking abortion care will choose the option most easily accessible to them, however, this should not be the default approach.
There are various factors that may influence the pain experienced by patients receiving an early surgical abortion (Table 1). It is important to develop gentle physical skills and effective social skills as an abortion provider. Encouraging and reassuring communication, including the “vocal local” technique, can help to reduce anxiety and pain, as can the support of a whānau member or friend. Guiding patients to take slow, deep, regular breaths may also assist in relaxation and help in avoiding hyperventilation.
Table 1. Factors associated with pain experienced during early surgical abortion.
| Increased pain
|
Decreased pain
|
Conflicting results
|
Not strongly associated
|
- Anxiety/depression
- Ambivalence
- Expectation of pain
- Younger patient age
- Dysmenorrhea
- Fewer pregnancies
|
- Previous vaginal delivery
- Older patient age
- More pregnancies
- Shorter operative time
- Participation in the choice of anaesthesia
|
- Gestational age
- Maximum cervical dilation
- Comfort with decision
- Provider experience
|
- Prior pelvic exam
- Prior uterine aspiration
- Prior caesarean section
- MVA vs EVA
|
Non-steroidal anti-inflammatory drugs
Table 2 outlines pre-procedural analgesic options for patients receiving an early surgical abortion. It is recommended to give non-steroidal anti-inflammatory drugs (NSAIDs), at least 30 minutes prior to an early surgical abortion. This reduces cramp pre- and post-procedure. Consider anti emetics as required by patients.
Table 2. Pre-procedure analgesic options for early surgical abortion.
| Medicine
|
Dose
|
Comments
|
Ibuprofen* |
600 – 800 mg PO |
Not available on PSO |
Naproxen* |
250 – 500 mg PO |
Not available on PSO |
Diclofenac |
50 – 100 mg PO* or PR |
Oral form not available on PSO |
Paracetamol |
1 g – 2 g PO |
Poor evidence. May be suitable for patients who cannot tolerate NSAIDs. |
*Some medicines are available on practitioner supply order (PSO). Medicines marked with an asterisk are recommended but not available on PSO.
Medicines for cervical priming
The New Zealand Aotearoa Abortion Guideline 2021 recommendation 3.2.1 states “Recommend cervical priming prior to surgical abortion before 14 weeks’ gestation, to reduce the risk of incomplete abortion and make the procedure easier to perform.”
Options for cervical priming in the first trimester include misoprostol or mifepristone.
The New Zealand Aotearoa Abortion Guideline 2021 recommendation 3.2.2 states “For people having surgical abortion prior to 14 weeks’ gestation, offer cervical priming with 400 micrograms misoprostol, administered sublingual 1 hour prior, buccal 1–3 hours prior or vaginal 3 hours prior”
Recommendation 3.2.3 is “For people having surgical abortion prior to 14 weeks’ gestation where misoprostol is contraindicated, consider cervical priming with 200 mg oral mifepristone 24–48 hours prior, to make the procedure easier to perform”.
Misoprostol (e.g. Cytotec®) is a synthetic prostaglandin E1 analogue which induces contractions of the smooth muscle fibres in the myometrium and relaxation of the cervix. Each Cytotec® tablet is 200 micrograms.
Misoprostol is recommended for cervical priming at a dose of 400 micrograms. The wait time before proceeding with the early surgical abortion procedure differs depending on parity and on the route the misoprostol is taken. The onset of action is:
- 1 hour for the sublingual route
- 1 – 3 hours for the buccal route
- 3 hours for the vaginal route
Multiparous people who have previously laboured may respond more quickly to misoprostol. This
should be taken into consideration when planning the order of a list of procedures. Staff in the
facility should be aware there may be a need to change the patient order if someone shows signs of
a medical abortion beginning and the person does not want a medical abortion, or staff are not
trained to manage medical abortion.
There are a number of situations where misoprostol is either contraindicated or where mifepristone may be easier for the person seeking the abortion. These include known hypersensitivity to misoprostol or any other ingredient of the product, or to other prostaglandins. In the situation of uncontrolled asthma (where the abortion cannot be delayed) or severe inflammatory bowel disease consideration should be given to using mifepristone due to the risk of bronchospasm and diarrhoea respectively with misoprostol. Prostaglandins are not recommended for people with moderate/severe cardiac disease and mifepristone may be an alternative option for cervical priming.
Mifepristone (e.g. Mifegyne®) is a synthetic steroid with anti-progestational properties as a result of competition with progesterone for progesterone receptors. In people at doses of ≥ 1 mg/kg, mifepristone antagonises the endometrial and myometrial effects of progesterone. There is a longer interval of 24 – 36 hours needed between taking mifepristone and the abortion procedure (compared with the shorter onset of action associated with misoprostol use).
Other reasons to consider mifepristone may include a history of multiple caesarean sections with a more advanced gestational age, or practical reasons such as if the patient prefers the convenience of taking it at an appointment 24 hours prior to the procedure (rather than one to three hours before with misoprostol).
Practice point: The use of misoprostol for cervical priming is an example of an unapproved use of medicine. Unapproved medicines have not been assessed by Medsafe for efficacy or safety of use for this specific therapeutic indication. However, under Section 25 of the Medicines Act 1981, they are able to be prescribed by authorised prescribers in New Zealand provided the Code of Health and Disability Services Consumers’ Rights 1996 has been applied. Patients have the right to be fully informed about unapproved medicines and any safety concerns, including in writing (if requested), prior to consenting to their use for early surgical abortion. Verbal informed consent from the patient is sufficient and this should be documented in the patient notes. It is not necessary to obtain written consent.
Follow this link to watch the presentation on Unapproved use of medicines (section 25) in Module 1
Local anaesthetic – paracervical block
A local anaesthetic is injected into the cervix using a technique known as the paracervical block.
For a video explaining this procedure, click here.
Care must be taken to ensure that the local anaesthetic dose does not exceed that recommended level (maximum 4.5 mg/kg) due to the risk of local anaesthetic toxicity. This may present as peri-oral numbness, tinnitus or a metallic taste in the mouth. At higher concentrations, muscular twitching, convulsions, cardiac arrhythmias and a loss of consciousness may occur.
There are various mechanisms for carrying out a paracervical block. All include insertion of local anaesthetic into the cervix at the “12 o’clock point” to decrease the discomfort of tenaculum placement (N.B. a “clock face” description is commonly used to identify locations for injections, when looking at the cervix of a person lying on their back; Figure 6). A 2012 random controlled trial (RCT) using a five site injection at 12, 2, 4, 8, and 10 o’clock demonstrated the benefit in terms of pain reduction in comparison to sham treatment. Alternatively, there are blocks using only three sites: 12, 4 and 8 o’clock.
The RCT confirmed that the paracervical block itself is painful and patients should be informed of this. Slow administration of local anaesthetic may reduce the pain associated with the paracervical block (Table 3). Use of buffering with bicarbonate can also reduce pain. One suggested regime is 20 ml paracervical block, 18 mL of 1% lignocaine buffered with 2 mL of 8.4% bicarbonate.
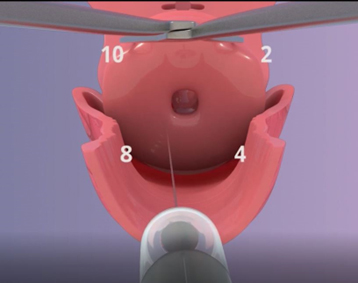
Figure 6. Cervix showing four paracervical block injection sites.
NB. This is a still from the “Early surgical abortion – Uterine aspiration procedure” video.
Table 3. Local anaesthesia options and additives for early surgical abortion.
| Drug (Class)
|
Dose Range
|
Comment
|
Lidocaine
(1% or 2%) |
Up to 200 mg
(20 mL 1% or 10 mL 2%) |
Lower concentration is as effective. |
Bicarbonate Buffer |
5 mL / 50 mL anaesthetic |
Less injection pain |
Sedation
ANZCA background paper for the PS09BP guideline, section 3.4 states: “The continuum of sedative/hypnotic drug effect extends from conscious sedation through deeper sedation to general anaesthesia. Regardless of the sedative and/or analgesic agent used, PS09 specifically limits the practice of medical and dental practitioners who are not anaesthetists, or other trained and credentialed medical practitioners practising within their scope of practice, to conscious sedation in healthy patients, because of the inherent risks in deeper sedation and general anaesthesia. These risks include airway obstruction, respiratory depression and cardiovascular instability. If deep sedation or general anaesthesia is desired or required, then an anaesthetist, or another appropriately trained and credentialed medical specialist within his/her scope of practice, must be present.”
There are multiple different levels and options for sedation in abortion care. abortion providers must receive training in sedation, airway and resuscitation skills appropriate to the care they are providing. This training in early surgical abortion by aspiration is not adequate to be considered sedation training. At least one assistant with training in monitoring sedation must also be present during the procedure. An early surgical abortion carried out using any degree of sedation beyond conscious sedation requires the services of a trained anaesthetist, or other trained and credentialed medical practitioner working within their scope of practice to monitor the patient during the procedure.
Medicines that may be used for early surgical abortion sedation are detailed in Table 4. In New Zealand the range of practice is wide with some providers using simple analgesia and paracervical block only, many using a range of oral or intravenous (IV) benzodiazepines with IV fentanyl (in addition to NSAIDs and paracervical block) and some centres that use general anaesthetic. If benzodiazepines are used, flumazenil must be available for reversal and if opioids are used, naloxone must be available.
Oxygen should be available for resuscitation and for routine use as indicated dependant on sedation.
Table 4. Recommended medicines for early surgical abortion sedation.
| Sedative
|
Dose
|
Comments
|
Midazolam |
1 – 2 mg IV or 7.5 mg oral* |
Give over 2 minutes. Oral formulation not available on PSO. Antidote is flumazenil (also not available on PSO). |
Lorazepam* |
0.5 – 1 mg SL or 1 –2 mg PO or IV |
Shorter acting benzodiazepine. Not available on PSO. Antidote is flumazenil* (also not available on PSO). |
Fentanyl* |
Up to 100 microgram IV |
Give over 30 – 60 seconds. Not available on PSO. Titrate by weight and pain. Antidote is naloxone |
Penthrox* |
One bottle of Penthrox® (1.5 mL or 3 mL) |
To be vaporised in a Penthrox® inhaler. |
*Some medicines are available on PSO. Medicines marked with an asterisk are recommended but not available on PSO.
