Introduction
Mihi / Acknowledgements
The New Zealand College of Sexual and Reproductive Health thanks the participants in our surveys, focus
groups, talanoa and hui whose perspectives and comments inform and improve our training content. This lived
experience, whether recent or historical, as patient, whānau or a whakatahe abortion* provider is a taonga to our collective knowledge.
We acknowledge the researchers whose qualitative and quantitative data paints a picture of where we have been and where we need to go. We appreciate the spheres you work in have never been easy and that many barriers remain to conducting the ongoing research needed. We are grateful to Alison Green and Te Whāriki Takapou, for sharing their knowledge of pre-colonial abortion and to the Bixby Center for Global Reproductive Health, and the Department of Family and Community Medicine, at the University of California, San Francisco, for their permission to use and adapt resources from their TEACH programme and Innovating Education in Reproductive Health.
We thank the subject matter experts who reviewed these modules, for their time and dedication to improving all aspects of abortion in Aotearoa New Zealand.
The New Zealand College of Sexual and Reproductive Health thank Ministry of Health - Manatū Hauora for funding the project to produce this training and look forward to working together to enhance access, equity, services, and mātauranga in the provision of abortion care in Aotearoa New Zealand.
* We have used the term ‘whakatahe abortion’ here but note that the terms ‘whakatahe’ and ‘tahe’ have other meanings in other contexts. For example, whakatahe can mean ‘fast flowing liquid’, which may apply to things other than blood. Whakatahe can also mean miscarriage and menstruation. Understanding of the meaning comes from the context of the whole sentence. There are a number of words in te reo that may be used for abortion. Patients in your area may prefer a different term and this should be used instead.
1. About NZCSRH
Nau mai haere mai, talofa lava and welcome to the New Zealand College of Sexual and Reproductive Health (NZCSRH) Online Training Environment. The NZCSRH started as The New Zealand Sexual and Reproductive Health Educational Charitable Trust in 2002, providing an advanced training pathway for doctors with a special interest in sexual and reproductive health. Now as NZCSRH, a new advanced training programme has been developed and is currently being reviewed by the Medical Council of New Zealand (MCNZ).
NZCSRH is focused on providing advice and support for all health professionals with a special interest in sexual and reproductive health. We have an associate membership for health professionals working in sexual and reproductive health including abortion care. NZCSRH are developing courses aimed at health providers with an interest in sexual and reproductive health who want to develop their practice, without becoming a specialist.
We welcome you to our abortion training package. If you have any feedback, ideas or would like to discuss this training further, please contact us: administration@nzcsrh.org.nz.
Joining NZCSRH and the Abortion Providers Group Aotearoa New Zealand (APGANZ)
We recommend that abortion service providers consider joining NZCSRH and APGANZ.
Benefits of NZCSRH membership (https://nzcsrh.org.nz/Associate/10914/) include:
- Monthly contraception and abortion peer review meetings
- Online educational resources
- Reduced conference/training course fees
- Regular training webinars and panel presentations by multidisciplinary experts in sexual and reproductive health (SRH)
- Becoming a trainer in SRH
The cost for associate membership is a yearly fee of $150 (including GST) which is subject to annual review.
The Abortion Providers Group Aotearoa New Zealand (APGANZ) is a group of professionals who work or have worked in New Zealand providing safe legal abortions. Members of the group are doctors (referring doctors and abortion providers), nurses and midwives, counsellors, social workers, managers, administrators and researchers.
New members are welcome. Benefits of membership include:
- Reduced rates for APGANZ educational meetings
- Access to the APGANZ Google discussion forum
- Updates on abortion related research
- APGANZ represents abortion providers views on important national issues
The APGANZ membership fee (2022–2023) is $100 for doctors and $40 for non-doctors. Student membership is free.
Continuing Professional Development
NZCSRH recommends that qualified health practitioners ensure they participate in continuing education in line with their vocational educational advisory body and that for health professionals involved in abortion care this includes continuing education and development in abortion care.
2. Introduction to abortion in Aotearoa New Zealand
Te Ao Māori in sexual and reproductive health
In the following presentation Dr Jo Lambert, Ngāti Maniapoto, Te Ati Awa, and a Fellow of the NZCSRH, presents an overview of Te Ao Māori in sexual and reproductive health.
Abortion overview
Following the changes to our abortion laws in March, 2020, pregnant people in Aotearoa New Zealand have the right to self-refer to an abortion service provider for an abortion up to 20 weeks gestation. After 20 weeks gestation the health practitioner involved is required to consult a second health practitioner and decide whether an abortion is clinically appropriate.
Abortion care providers need to support and communicate effectively with the pregnant person throughout the decision-making and abortion process, enabling them to make their own informed decisions with clear understanding and expectations. Ideally if there are no contraindications, people should be given a choice of how, where and by whom they receive abortion care including options of medical or surgical abortion. In reality, care options are often limited by gestational age, location and practitioner skill sets.
Early medical abortion (EMA) is technically simple to provide; the important elements are in the assessment, communication with the patient, and evaluation of success. Mifepristone 200 mg is taken orally first, followed 24 to 48 hours later by misoprostol 800 micrograms (taken buccally, sublingually or vaginally). This combined regimen is more effective than misoprostol alone and is safe and successful >95% of the time, meaning no further intervention is required to complete the abortion.
In New Zealand, mifepristone is licensed for use up until 63 days (nine weeks). There are some studies of EMA provided from 64–70 days, suggesting 91–93% success rates, and use at this gestational age is approved by the US Food and Drug Administration. The World Health Organization Abortion Care Guideline (2022) supports medical abortion in primary care until 12 weeks. Outside of the 63 day approved gestation in New Zealand, mifepristone for EMA can be prescribed for patients under Section 25 of the Medicines Act 1981, and the New Zealand Aotearoa Clinical Guideline recommends its use for EMA up to 10+0 weeks’ gestation.
EMA can be offered in an outpatient setting in the community, or with the support of a primary care provider, an EMA can take place at a person’s home. It is important to have good communication between patients and primary care providers, between patients and the abortion service, amongst abortion providers, and between the abortion service and local gynaecology services in case of complications. EMA can be easily integrated into primary care and other clinical services and allows providers to play an important role in expanding access for patients.
Early surgical abortion using vacuum aspiration is usually a technically straightforward procedure that can be performed with manual or electric vacuum. Procedures can be done under local anaesthetic with or without analgesia and/or mild sedation, in an outpatient setting in the community.
After a bimanual examination to assess the size and shape of the uterus, the procedure is: insert the speculum, administer the paracervical block, dilate the cervix, and aspirate the pregnancy tissue. Ensuring the procedure is complete can be achieved by routine inspection of the aspirated tissue for products of conception or with an ultrasound scan. The use of gentle, neutral language and avoidance of words associated with pain may decrease pain perception during the procedure.
Early surgical abortion is safe with a 99% success rate. Fewer than 1% of patients have a complication requiring hospitalisation and fewer than 1% experience an ongoing pregnancy).
Second and third trimester abortion can be either surgical (dilatation and evacuation, preceded by cervical priming) or medical (taking medicines to induce a miscarriage). These procedures are usually performed in a hospital setting and are not included in this training.
Confusion between Early Medical Abortion (EMA) and the Emergency Contraception pill (ECP)
Early medical abortion (EMA) is sometimes confused with emergency contraception, including in news reports and in television shows. EMA is the process of taking pills to cause a pregnancy to stop growing and to be expelled. The Emergency contraception pill (ECP) used in New Zealand is POSTINOR®-1. This contains a high dose of levonorgestrel that works by preventing or delaying ovulation. Therefore it does not work once a pregnancy is established.
The two main forms of emergency contraception used in New Zealand are the Emergency Contraceptive Pill and a Copper IUC.
Table 1. Differences between medical abortion and emergency contraception
| Medical Abortion |
Emergency Contraception |
Ends an early pregnancy and causes it to expel |
Delays or prevents ovulation.
Prevents implantation. |
Pills are taken in first - 10 week of pregnancy |
Pills are taken or a copper IUC used within days of unprotected sex. Further information |
Usually causes heavy bleeding and cramps |
Mild side effects, if any |
Stops pregnancy about 98% of the time |
Pills prevent 92% of pregnancies. Copper IUD prevents 99.9% of pregnancies. |
Other considerations in providing abortion
Although much of this training is based on the clinical aspects of providing an abortion, it is extremely important to consider the patient as a whole, including social and cultural impacts.
Intersectionality recognises that individuals may face multiple and intersecting forms of structural discrimination, due to sexual orientation and identity, gender and gender identity, ethnicity, disability, or other aspects of their identity, and that this systemic discrimination can impact on their access to, and experiences of health care.
This should be a key consideration when setting up new health services and when addressing the needs of individual patients. It is also important to allow the time and space for people to make decisions; for instance, clinicians need to be prepared for a consultation to last up to an hour or more.
Abortion in precolonial Aotearoa New Zealand
By Dr Alison Green, Te Whāriki Takapou
Knowledge about precolonial Māori understandings of fertility, birth and what is referred to today as abortion was subjugated following the arrival of colonial settlers to Aotearoa. Although some of the early knowledge was recorded in writing by Pākehā male ethnographers, it was interpreted through a colonial lens that was strongly influenced by Christian and patriarchal ideologies. This resulted in misrepresentations of Māori customary practices, traditional values and principles that led, in particular, to the marginalisation of the role and authority of women as ‘whare tangata’ or the bearers of future generations.
A range of Māori terms for the loss or removal of a pregnancy are recorded in Māori dictionaries, mōteatea (song chants), pūrākau (origin stories) and tribal narratives. Understandings of these terms encapsulate broad concepts, connotations and referents: for example, whakatahe can refer to ‘abortion’, as well as ‘the clearing of obstructions’, and ‘sacred food offered to atua’. The Māori language does not distinguish between miscarriage and abortion: materoto can refer to ‘miscarriage’, ‘abortion’ or ‘stillbirth’; tahe can refer to ‘miscarriage’, ‘abortion’ or ‘menstruation’; and whakatahe refers to both ‘miscarriage’ and ‘abortion’. There is evidence in tribal narrative accounts of Māori in precolonial Aotearoa having effected the removal of a pregnancy, as well as records of certain plants or leaves used for medicinal purposes (rongoā) being known to have contraceptive or ‘abortifacient’ properties.
Further reading on the history of abortion in Aotearoa NZ
Te Ara – the Encyclopedia of New Zealand has a story by Megan Cook (published 5, May, 2011, reviewed & revised 8, Nov, 2018) describing the history of abortion in New Zealand, which includes several images and film clips. Available at this link: https://teara.govt.nz/en/abortion
Stuff Circuit has an interactive webpage ‘Your Decision’ with 21 reader submissions of abortion experiences contributed in 2019 (prior to the change in law), as part of their ‘Big Decision’ investigation into the abortion law reform debate. Stuff Circuit is Stuff’s video-led, longform investigative unit and is funded by NZ On Air and is created in partnership with Māori Television. Available at this link: https://interactives.stuff.co.nz/2019/circuit/your-decision/
Le Grice, J. and Braun V. ‘Indigenous (Māori) perspectives on abortion in New Zealand’ Feminism & Psychology 2017: 0(0) 1–19.
Le Grice, J. ‘Māori and abortion: an ‘impossible’ choice?’ Women's Health Update 2014: 18:3.
This video shows the situation prior to the recent abortion law reforms from the perspective of a patient accessing services:
How to get an abortion in New Zealand | On the Rag: Abortion
Aotearoa New Zealand abortion statistics
Abortion statistics prior to 2020 are available on the NZ Stats website, and annual reports (2012-2020) by the Abortion Supervisory Committee can be downloaded from the Ministry of Justice website. Annual abortion services reports from 2020 are now published by the Ministry of Health, and can be accessed through their publications webpage. The annual reports collate and summarise information collected through the abortion reporting process.
Useful information in planning abortion services:
- The abortion rate is slowly decreasing
- Approximately 19% of known pregnancies (excluding miscarried pregnancies) end in an abortion
- The mean age of those having an abortion is about 28 years old, with 40% aged 30 or over
- 59% of people having an abortion had had at least one previous live birth
- The percentage of abortions accessed before 8 weeks gestation is increasing (45% in 2020) and the rate of early medical abortion has increased significantly
The information above is from Ministry of Health. 2021. Abortion Services Aotearoa New Zealand: Annual report. Wellington: Ministry of Health. ISBN 978-1-99-100761-2 (online). Licensed under the Creative Commons Attribution 4.0 International licence. Available from: https://www.health.govt.nz/system/files/documents/publications/abortion_services_aotearoa_new_zealand_annual_report_2021_8_oct.pdf
3. Becoming an abortion service provider
Requirements to become an abortion service provider
Prior to the 2020 legislation, only a medical doctor was able to be an abortion service provider. The Abortion Legislation Act 2020 enabled a qualified health practitioner to provide abortion services (Part 1, Amendments to Contraception, Sterilisation, and Abortion Act 1977, section 8). Registered health practitioners can perform surgical abortions or prescribe medicines for medical abortions if it is a health service permitted within their scope of practice and the practitioner holds a current practicing certificate. Abortion is within scope of practice for doctors, midwives, nurse practitioners and registered nurses.
A Cochrane review showed no statistically significant difference in the risk of failure for medical abortions performed by mid-level providers (such as nurses and midwives) compared with doctors.
Assessment and certification
The NZCSRH recommends that you have the following skills prior to commencing abortion training:
Qualified health practitioners who wish to provide abortion services must successfully complete Module 1 Consultation – communication and decision making, before proceeding to the other modules. After completing the first module, participants’ knowledge is assessed through an online quiz, and once this is successfully completed, a certificate can be downloaded. The EMA training unit (Module 2) is also assessed by an online quiz. There are theory assessments and practical competency tests for the early surgical abortion and point of care ultrasound units (Modules 3 and 4).
Notification of new services to Manatū Hauora
All abortion service providers are required to inform Manatū Hauora that they will be providing a new service. This notification
can be sent by email to abortionservices@health.govt.nz. Further information can be accessed at the Manatū Hauora abortion
services website.
Referral process and onwards pathways
People seeking an abortion may self-refer or be referred by another health practitioner. It is essential that abortion providers have a process for managing referrals including self-referrals to them. New abortion providers should review the support services in their communities, including local hospitals, early pregnancy clinics, counselling services, sexual health services, and family violence services, to establish contacts and referral pathways.
Prior to providing abortion care, qualified health practitioners must ensure they have developed referral pathways in their region for the management of complications associated with abortion provision including surgical abortion and emergency care.
Availability of service
Abortion services are recommended to provide access to 24-hour support of the patient. The Ministry of Health has contracted Family Planning and Magma Healthcare to establish and provide a National Abortion Telehealth Service (DECIDE). It is intended that this service will help to support primary care practitioners to provide abortion services through access to virtual counselling and 24/7 clinical support for primary care providers.
Professional support
We recommend that new abortion providers identify a mentor for guidance and advice who is experienced in providing abortion care. Ideally this would be someone in your community, however, if you are not able to find someone, you can contact NZCSRH (https://www.nzcsrh.org.nz/) for help in linking you with a mentor. Another good place to gain continuing education and contacts/mentors is through the Abortion Providers Group Aotearoa New Zealand (APGANZ).
Telehealth option
Telehealth is the use of information and video conferencing technologies to deliver health services to patients. The Medical Council of New Zealand (MCNZ) published an updated statement on the use of telehealth in October, 2020. We recommend applying these principles if you intend to provide abortion care via telehealth. Note if a patient requests a complete telehealth abortion service (i.e., no in person visit) and is assessed as suitable for telehealth EMA, we recommend they use the DECIDE nation telehealth service. More information.
The required standards of care for telehealth are the same as those for in-person consultations. This should include 24-hour support of the patient and confirmed availability of local support and emergency services. Providing abortion care by telehealth is discussed in further detail in Module 2: Early Medical Abortion.
Abortion Reporting
To comply with the Contraception, Sterilisation, and Abortion Act abortion service providers must submit a notification of abortion to the Ministry of Health (the Ministry) for every abortion provided within one month of the procedure. The reporting form can be accessed via this link: https://www.alrnotifications.health.govt.nz/
There is also a requirement for abortion service providers to submit an annual report to the Ministry by 31 March each year. Annual reporting forms are submitted to abortionservices@health.govt.nz. Forms will be send to all abortion providers, but if you haven’t received a form, please contact the Ministry via the abortion services email.
The ‘Abortion reporting’ webpage at the Ministry of Health website link provides further guidance on abortion notification and annual service reporting.
The Ministry collates the national data on abortions and reports upon this annually. The data is also used for the five yearly periodic review of timely and equitable access to abortion services, abortion related counselling services, pregnancy options information, contraception and sterilisation services.
Staffing and equipment
EMA can be provided within a community setting or by telemedicine with minimal physical requirements. The process, including consultation and decision-making, and explanation of how and when to take the medicine with the patient, is estimated to take about an hour. It is critical to provide a welcoming space – all staff need to be part of the abortion care service creating a safe environment for people seeking an abortion. Confirming a pregnancy using a high sensitivity urine test is an important first step, and we suggest that abortion care providers ensure that tests are freely available on request.
Early surgical abortion requires specifically trained staff for provision and management of analgesia/sedation and spaces that are safe to provide early surgical abortion. These requirements are described in detail in Module 3.
Providing a high quality service and auditing your practice
Ngā Paerewa Health and Disability Service Standard (nz-81342021) along with the Aotearoa NZ Abortion Clinical Guidelines replaced the Interim Standards for Abortion Services in New Zealand.
Ngā Paerewa sets out the standard for health and disability service providers. Ngā Paerewa clearly sets out which sections of the standard apply to abortion service providers. Te Tiriti obligations and International Human Rights legislation underpin the standard and are evident throughout providing clear guidance on the expected standard of care service users should be receiving.
Note that while only hospital-based abortion service providers will be formally audited against Ngā Paerewa, but it is recommended that all health practitioners and providers apply Ngā Paerewa within their service and undertake self-audits to ensure their service provides a high standard of patient focused care.
All health practitioners providing abortion services should be following the Abortion Clinical Guidelines as the accepted standard for best clinical practice.
The Ministry of Health as the system steward and regulators of abortion services use service reporting and other mechanisms, including audits and complaints to monitor abortion service providers.
Values clarification and talking about abortion
Discussion groups that were used in developing this training have clearly identified that when it comes to abortion, the manner in which the service is delivered, for example with cultural and spiritual (Taha wairua) safety, manaakitanga (respect), kindness and without judgement, is just as important to people receiving care as clinical competence. (Figure 1).
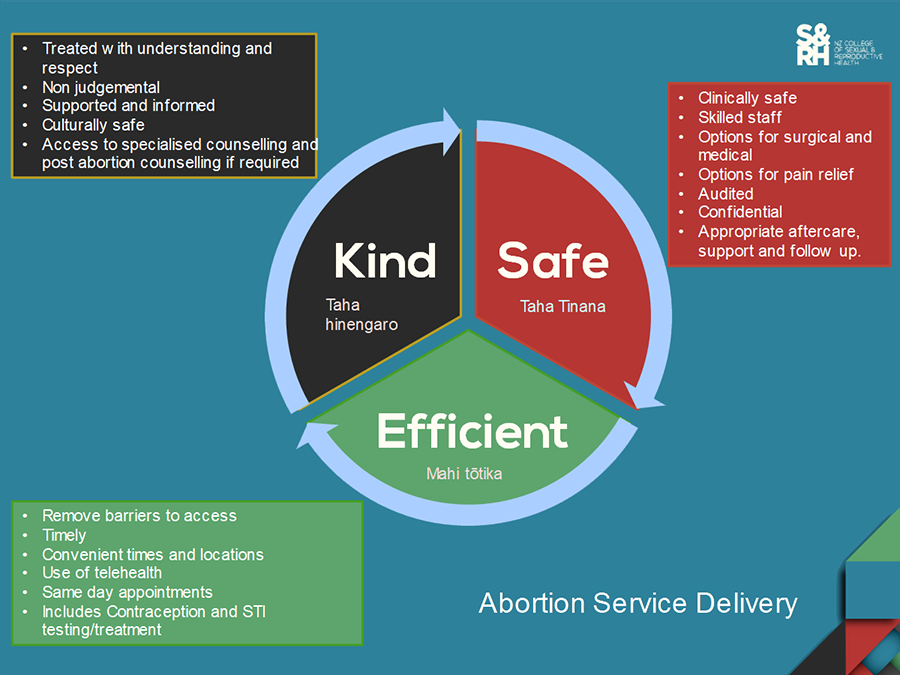
Figure 1. Aspects of abortion service delivery
In order to ensure that you are aware of your bias to ensure it is not impacting safe patient care, it is useful to undertake a values clarification exercise, to better understand your personal beliefs and values and where the gaps may exist, so you know in which areas you need to increase your cultural competence.
Current issues relating to providing abortion services in Aotearoa New Zealand
Abortion services and related counselling services are free in New Zealand to any pregnant person eligible for publicly funded health care, however, there is often a fee for an ultrasound scan. Additional barriers to access might also be present due to factors such as contextual circumstances, transport, distance, perceived cost, relational matters and childcare.
It is essential for abortion providers to know what abortion services are available for people in their area, so that if they are not able to provide the care people need or choose, for example an early surgical abortion rather than an EMA, they can refer them to an abortion service which can provide this care.
At present the DECIDE website is the website recognised by the Ministry as the recommended source of consumer information on where people requiring abortion services can go to get an abortion and what types of services are available based on gestational age.
Improved access is important to achieving earlier treatment. For instance, access may be improved through:
- Access to pregnancy tests to identify pregnancy at earliest opportunity
- Self-referral
- Ease of booking an appointment
- Services available locally
- Requiring only one in person service visit where this is appropriate
- Full range of sexual and reproductive services available during the in person visit, including provision of more effective forms of contraception such as long-acting reversable contraceptives (LARC)
- Good service information including service accessibility, information on what to expect, choices, effectiveness and complication rates and information on whanau attending with the patient
Improved abortion services in New Zealand will lead to:
- Better health outcomes – improved access to a culturally and clinically safe services leading to better health outcomes
- Earlier gestation at time of treatment. Abortion is safer and better for patients the earlier it is performed.
- Better contraception – improved access to LARC contraception.
- Greater treatment choice - local services offering medical and surgical options.
4. Overview of the training modules
There are four online theory modules available:
- Consultation – Communication and decision making
- Early medical abortion (EMA)
- Early surgical abortion (ESA)
- Point of care ultrasound in first trimester abortion (POCUS)
The online training incorporates video, animations, presentations with voiceover and downloadable documents. All trainees must complete the Consultation module before proceeding to the EMA, ESA or POCUS modules (a detailed list of contents for each module is listed below). Each module finishes with a quiz to assess understanding and knowledge of the key points of the module. Participants must answer all of these quiz questions correctly to complete the module and are able to repeat the quiz as many times as needed to achieve this.
Summary of training requirements
| Abortion service you wish to provide |
Compulsory modules |
Optional modules |
| Early Medical Abortion |
1 and 2 |
4* |
| Early Surgical Abortion (ESA) |
1 and 3* |
4* |
| EMA and ESA |
1, 2 and 3* |
4* |
*NB modules 3 and 4 have additional practical requirements (supervised practice) that must be completed and practitioner competency signed off by an appropriately qualified supervisor BEFORE a health practitioner is able to start providing surgical abortion or point of care ultrasound without supervision The practical competency requirements are outlined within the theoretical ESA and POCUS modules.
5. Registration
Before commencing training
There are four online theory modules available at:
Prior to commencing this NZCSRH module in abortion care participants should download personal copies of:
These standards and guidelines will be referred to throughout the training with regards to how they apply to the provision of abortion care.
It is recommended that you have the following skills prior to commencing abortion training:
It is also vital that you know how to access and refer people to social support services including violence intervention, addiction, youth support mental health and other health and social services following a positive risk screen. Your organisation should have screening tools to assist in identifying these issues.
Having access to interpreting services and cultural support services is also useful to support your service being accessible and safe for a range of cultures.
All people requesting abortion MUST be offered the option of having pre-abortion counselling so you need to know how to access abortion counselling services. The DECIDE national telehealth service offers virtual abortion counselling for patients accessing abortion via a primary care based abortion service provider. Hospital based abortion providers typically link to appropriately trained social workers within the hospital workforce to provide both abortion counselling and referrals for health and social support services when required.
Providing feedback on training
Your feedback is invaluable to us to assist in improving the course. We would appreciate your assistance by completing the following short form.
6. Abbreviations
ANZCA |
The Australian and New Zealand College of Anaesthetists |
ASC |
Abortion Supervisory Committee |
APGANZ |
Abortion Providers Group Aotearoa New Zealand |
βhCG |
beta human chorionic gonadotropin |
CMT |
cervical motion tenderness |
COCP |
combined oral contraceptive pill |
CRL |
crown-rump length |
ECP |
emergency contraception pill |
ED |
emergency department |
EDD |
estimated date of delivery |
EMA |
early medical abortion |
EVA |
electric vacuum aspirator |
IM |
intramuscular |
IPV |
intimate partner violence |
IUC |
intrauterine contraception |
IUP |
intrauterine pregnancy |
IUS |
intrauterine system |
IV |
intravenous |
LARC |
long-acting reversible contraception |
LGBTQI+ |
lesbian, gay, bisexual, transgender, queer, intersex, + |
LMC |
lead maternity carer |
LMP |
last menstrual period |
MCNZ |
Medical Council of New Zealand |
MOH |
Ministry of Health |
MSD |
mean sac diameter |
MVA |
manual vacuum aspirator |
NAAT |
nuclear acid amplification test |
NSAID |
nonsteroidal anti-inflammatory drug |
NZCSRH |
New Zealand College of Sexual & Reproductive Health |
OCP |
oral contraceptive pill |
PID |
pelvic inflammatory disease |
PO |
per oral |
POCUS |
point of care ultrasound |
POP |
progesterone only contraceptive pill |
PPE |
personal protective equipment |
PR |
per rectum |
PSO |
practitioner supply order |
PUL |
pregnancy of unknown location |
PV |
per vagina |
RPOC |
retained products of conception |
SL |
sublingual |
SOGIESC |
sexual orientation, gender identity, gender expression and sex characteristics |
SRH |
Sexual and reproductive health |
STI |
sexually transmitted infection |
TV |
transvaginal |
TVUS |
transvaginal ultrasound |
US |
ultrasound |
WHO |
World Health Organization |
7. Glossary of Te Reo Terms
Aotearoa |
Indigenous name for New Zealand |
Awa |
river, rivers |
Atua |
god/godess, deity, supernatural being, menstrual blood |
Hākari |
feast, gift, entertainment |
Hapū |
to be pregnant, subtribe |
Harakeke |
flax |
Hine |
girl, daughter |
Hine-ahu-one |
the first woman |
Hine-nui-te-pō |
goddess of stardust and sunlight, also known as the goddess who receives the dead |
Hina-te-iwa-iwa |
goddess of the moon and reproductive cycle of women, goddess who resides over the women’s esoteric knowledge and ceremonial arts |
Hine-tītama |
daughter of Hine-ahu-one, goddess of the dawn, binding night and day |
Hinengaro |
psychological, the hidden maiden |
Ia |
he/she, him/her |
Ipu |
container, bowl, vessel |
Ipu Whenua |
container to hold placenta or pregnancy tissue (preferably bio friendly to break down once buried) |
Iwi |
tribe, tribal nation, collection of families related through a common ancestor, human bone |
Kai |
food, to eat |
Kaimoana |
seafood |
Kāinga |
house |
Kaitiaki |
guardian, caretaker |
Karakia |
chant, incantation |
Kāwanatanga |
governance, government |
Kaumātua |
elder |
Kaupapa |
topic, subject, theme |
Kaupapa Māori |
living through tikanga |
Kete |
basket, kit |
Koha |
donation or gift |
Kohukohu |
sphagnum moss |
Kōrero |
talk, to speak, narrative |
Kuia |
elderly woman |
Kuka |
dry flax leaves, abortion |
Mahi |
work |
Mana |
prestige, authority, control |
Mana Wahine |
power and authority of Māori women |
Manaakitanga |
to support, give hospitality, show respect and generosity to others |
Manuhiri |
visitor, guests |
Materoto |
miscarriage, abortion, spontaneous abortion, stillbirth, to be stillborn |
Marae |
open area in front if meeting house, also refers to general complex of buildings and land |
Mātauranga Māori |
education, wisdom and knowledge skill pertaining to Māori |
Maui |
Polynesian cultural hero and demigod |
Maunga |
mountain |
Mihi |
acknowledge, greeting |
Moana |
sea |
Moko |
print, tattoo |
Mokopuna |
grandchild, grandchildren |
Ngahere |
forest |
Noa |
to be free from the restrictions on tapu, unrestricted |
Oranga |
wellbeing, health, living |
Pākehā |
non Māori, European settlers |
Papatūānuku |
earth mother |
Pōwhiri |
ceremonial welcome |
Puna |
a well, spring |
Pūrākau |
origin stories |
Rangatahi |
young person, adolescent |
Rangatira |
chief (male and female) |
Raranga |
to weave |
Ranginui |
Sky Father, God of the Sky |
Tāne |
male, man |
Tāne-Mahuta |
atua of forests, trees and birds |
Te Taiao |
the environment |
Te taha hinengaro |
the psychological side |
Te taha tinana |
the physical side |
Te taha wairua |
the spiritual side |
Te taha whānau |
family wellbeing |
Tara |
vagina |
Tahe |
Menstrual blood, abortion, menstruation, exude, drop, flow |
Tangata |
people |
Tangata whenua |
people of the land |
Taonga |
treasure, possession |
Tapu |
to be sacred, set apart, under atua protection, restricted |
Te Ao Māori |
the Māori world, Māori worldview |
Te Ao Mārama |
the world of life, light, the physical world |
Te Kore |
the void, the primordial womb-space at the beginning of the world |
Te Reo Māori |
the Māori language |
Te Tiriti o Waitangi |
Māori version of the Treaty of Waitangi |
Tikanga |
correct procedure, custom, practice, habit |
Tinana |
body, physical |
Tino rangatiratanga |
political, social, cultural and economic autonomy |
Tipuna/Tupuna |
ancestor |
Tīpuna/Tūpuna |
ancestors |
Toto |
blood |
Uha |
vulva, female genitals, femaleness |
Ure |
penis |
Wā |
time, season |
Wahine |
woman |
Wāhine |
women |
Waiata |
song |
Wairua |
spirit, soul |
Wairuatanga |
spirituality |
Waka |
canoe |
Wānanga |
learning, series of discussions |
Whaea |
mother, aunt, female relative |
Wahakura |
woven harakeke (flax) bassinet for infants |
Whaiora |
seeker of wellbeing, client, patient |
Whakaaro |
thoughts |
Whakairo |
carving |
Whakamana |
to authority or prestige to, to enhance the mana of another/others |
Whakapapa |
geneology, descent lines, to layer , past influences |
Whakataukī |
proverb, saying |
Whakawhanaungatanga |
to make relationships |
Whare |
house |
Whānau |
family, to be born, to give birth |
Whare Tangata |
house of humanity, womb |
Whenua |
land, placenta, pregnancy tissue |
Whenua ki te whenua |
returning the placenta to the land |
