Published: 26th April 2022 | Updated: 9th February 2024 |
What's changed?
9th February 2024 Revised management figure and added update box based on 2023 ACC concussion guidelines for community sport
Key practice points:
- Recognising concussion in primary care can be challenging as symptoms and signs are often subtle, non-specific, and can progress over time
- Initial loss of consciousness only occurs in one in ten people with concussion
- The Brain Injury Screening Tool (BIST) is a standardised and validated assessment tool to evaluate patients with suspected concussion; this is specifically tailored for use in time-limited clinical consultations
- Initial management of patients with concussion involves physical and mental rest for 24 – 48 hours; in most cases patients should then progressively re-engage in normal activities after this rest period, assuming the degree of engagement does not significantly worsen symptoms – excessive rest can prolong recovery.
- Patients who have sustained a sports-related concussion should be immediately removed from play, and not return until they have been medically cleared after completing a graduated return-to-play protocol
- Patients can be reassured that most people who experience a concussion will fully recover within two to four weeks. However, recovery is strongly influenced by the timeliness of clinical review and follow-up, effective education delivered at an appropriate level of health literacy (and whether the advice given is culturally appropriate/relevant), as well as other patient-specific factors, e.g. initial symptom burden, pre-existing mental health conditions, willingness, motivation and support to engage in their recovery.
- Some patients may continue to experience persistent concussion symptoms lasting longer than three months; addressing these symptoms can be challenging and may involve reconsidering differential diagnoses, reviewing medicine use and assessing mental health status, other stressors and social support
- International diagnostic classification systems no longer recognise “post-concussion syndrome” as a diagnostic entity, and the Accident Compensation Corporation (ACC) no longer accepts this as a diagnosis for brain injury or its subsequent symptoms (see main text for more details on this)
Concussion is defined as “the acute neurophysiological event related to blunt impact or other mechanical energy applied to the head, neck or body […] which results in a transient disturbance of neurological function”.1 This term is often used interchangeably with mild traumatic brain injury (mTBI) in the medical literature, however, it more specifically describes a pattern of symptoms and signs that a person may experience following mTBI (see: “Recognising the symptoms and signs of concussion”).1 As such, while all concussions are mTBIs, not all mTBIs are concussions.
The most commonly reported causes of concussion in New Zealand are falls, colliding with an object, being struck by a person (or animal) and driving-related accidents (including bike accidents; Figure 1A).2, 3 Although people often associate concussions with sporting accidents, this only accounts for 20 – 30% of events overall.2, 3 Approximately one-third of sports-related concussions involve people playing rugby union.3
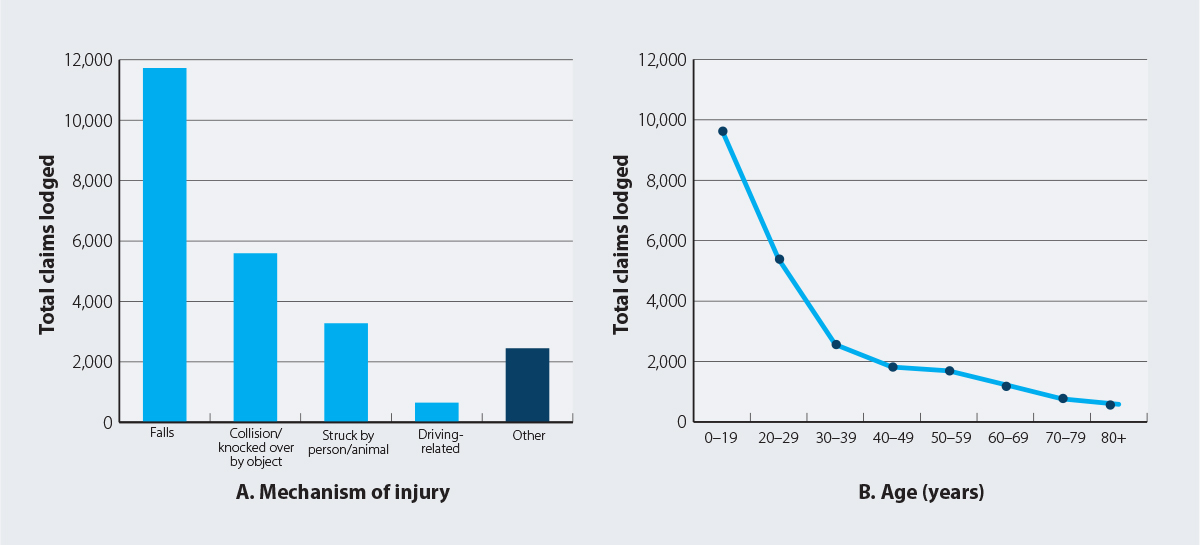
Figure 1. New concussion injury claims made to ACC between 1 July 2020 – 30 June 2021 by (A) mechanism of injury and (B) age group in New Zealand.3
N.B. This time period falls between the first and second nationwide lockdowns associated with the COVID-19 pandemic, and therefore data is not expected to be significantly affected by corresponding restrictions on people’s activities and daily living. The data and associated trends for this period are similar to observations for previous years.
A closer look at the demographic trends
It is estimated that 36,000 people in New Zealand sustain a traumatic brain injury (TBI) each year, 95% of which are mild in severity.2 Many of these people do not seek medical evaluation after sustaining a concussion.2 Between 2016 – 2021, an average of approximately 21,000 new concussion-related claims per year were lodged with the Accident Compensation Corporation (ACC)/Te Kaporeihana Āwhina Hunga Whara.3
Younger people have the highest risk of concussion
The population sustaining concussions is unique with respect to many other medical conditions in that they are typically active and otherwise healthy.4 Groups at increased risk of concussion in New Zealand include:2, 3, 5, 6
- Younger people – Between 2020 and 2021, people aged less than 30 years accounted for 63% of ACC concussion claims (Figure 1B)
- Males – Who are almost twice as likely to experience a concussion compared with females
- Māori and Pacific peoples – Māori have a 23% higher risk of concussion compared with Europeans. The incidence of all TBIs for Pacific peoples is 1,242 per 100,000 person-years, compared with 842 per 100,000 person-years for Europeans.
Pathophysiology associated with concussion
The pathophysiology associated with concussion is complex and not fully understood.7, 8 However, the current international consensus is that concussion occurs as a result of functional disturbances rather than macrostructural damage, e.g. bruising, bleeding, swelling.8 As a result, imaging is not required to diagnose concussion, and should only be requested if a more severe TBI is suspected (see: “Diagnose concussion based on clinical judgement”).
A concussion injury to the brain occurs either as a result of a direct impact to the head, or via “impulsive” force being indirectly transmitted to the head.8 The associated biomechanical forces (e.g. rapid acceleration/deceleration, rotational forces) disrupt cell membrane and axonal integrity, which triggers an acute cascade of significant neurometabolic changes.7, 8 During this process the indiscriminate release of glutamate from cells, in addition to changes in ionic flux (e.g. potassium efflux, sodium and calcium influx) triggers “spreading waves” of depolarisation which cause many of the acute symptoms and contributes to inflammation within the brain.7, 8 Cerebral blood flow is also reduced following a concussion event, which reduces the energy available to the brain for repair.8 Neurometabolic changes may also induce secondary injuries that can progress as the brain attempts to compensate and re-establish normal functioning.7, 8
The minimum threshold of force required to cause a concussion is unknown and it is difficult to quantify as the injury depends on a range of confounding variables, e.g. whether the person was able to brace themselves before impact or if they have had previous concussions. A study of impacts sustained by high school-aged American Football players* demonstrated that most concussions occurred when the head reached an acceleration value of approximately 90 – 100 g-force.9 Notably, the magnitude of impact did not consistently predict the severity of symptoms, supporting the theory that force is not the only factor associated with this type of injury.9
*Force was measured using a wireless accelerometer integrated into the player’s helmet (The Head Impact Telemetry [HIT] System).
People with suspected concussion will often seek immediate review at a hospital emergency department or urgent care clinic. However, others will initially present at their community general practice, sometimes several days to weeks after injury, particularly if they have mild or delayed symptoms.10 In some cases, the patient may not have considered that their symptoms could be indicative of a concussion, and therefore do not immediately report an accident or injury as having occurred.
Concussions can be challenging to recognise as the symptoms and signs are often subtle, non-specific, and the combination of features can vary substantially.11 In general, concussion symptoms/signs can be divided into three main categories: physical, cognitive and behavioural/emotional (Table 1).11 However, no features alone, or in combination, are specific for concussion, and many overlap with those seen in other conditions or scenarios, e.g. hypoglycaemia, alcohol or drug intoxication.
 Loss of consciousness does not usually occur. While people commonly associate concussion with loss of consciousness, this occurs in fewer than 10% of cases.11, 12 However, loss of consciousness means that a concussion is more likely, and prolonged loss of consciousness should raise suspicion of more serious injury.11
Loss of consciousness does not usually occur. While people commonly associate concussion with loss of consciousness, this occurs in fewer than 10% of cases.11, 12 However, loss of consciousness means that a concussion is more likely, and prolonged loss of consciousness should raise suspicion of more serious injury.11
Table 1. Symptoms and signs associated with concussion.1, 11, 13
|
Symptoms and signs indicating possible concussion |
|
Physical |
Cognitive |
Behavioural/emotional |
| Common |
- Headache
- Neck pain or tenderness (mild-moderate)
- Nausea/vomiting
- Tinnitus
- Taste/smell impairment
- Dizziness/vertigo
- Photosensitivity or sensitivity to noise
- Transient diplopia (double vision)
- Balance or motor inco-ordination
|
- Confusion/disorientation
- Brief loss of consciousness (< 2 minutes)
- Difficulty concentrating
- Difficulty remembering things
- Feelings of being “slowed down” or “in a fog”
- Witness reports person was slow to get up after injury
|
- Irritability and other transient personality changes, e.g. disinhibition
- Emotional lability
- Psychological adjustment problems and depressive/anxious symptoms
- Difficulty attending work or school
- Fatigue, drowsiness and sleep disturbances (including insomnia) or sleeping more than usual
|
| Red flags to consider for emergency referral |
- Worsening of initial symptoms
- Severe or increasing headache
- Severe neck pain
- Repeated vomiting (as a general guide, more than one vomit in an adult or any vomiting in a child)
- Seizures or convulsion
- Ongoing diplopia or other significant visual disturbances
- Weakness, tingling or a burning sensation in the arms or legs
- Ongoing or severe dizziness/vertigo
|
- Prolonged loss of consciousness (≥ 2 minutes), or deteriorating conscious state
- Inability to recognise people or places
- Dysarthria (slurred speech)
- Prolonged post-traumatic amnesia (> 12 hours)
|
- Increasing restlessness, agitation, confusion or combative behaviours
- Significantly unusual/inappropriate behaviours or personality changes
|
Digging deeper to support suspicions
Ask questions about any recent accidents or injuries
If a concussion is suspected, a plausible mechanism of injury needs to be established. Patients should be asked to describe any recent accidents or injuries in as much detail as possible, including when/where it occurred, details about the event itself, and what happened directly afterwards up until the time of the appointment.10 Given that confusion and short-term memory impairment are common features of concussion, this information may be derived from a witness account of the event, via a caregiver or video footage. Concussion should be strongly suspected if there is documented evidence or report of direct trauma to the head/body or exposure to acceleration of deceleration forces.11
Examples of questions include:10
- Do you remember what you were doing when the accident occurred, or were you told this information?
- Did you hit your head, or did your head jolt back and forth? If so, how hard?
- Did anyone say you were lying still or were unresponsive directly after the accident?
- Were you able to answer questions from people, talk coherently and think clearly afterwards?
- Have you previously had a concussion?
Neurocognitive and physical testing
Sometimes the features of concussion only become apparent when a patient is asked to complete certain tasks that challenge their neurocognitive or physical abilities, e.g. immediate and delayed word recall, reciting a sequence of numbers or months in reverse order or balance testing.14 However, no single test is validated for assessing patients with suspected concussion in the absence of a baseline score; instead, a variety of tests usually form part of multifaceted screening assessment to identify any additional clinical deficits.14 Examples include Vestibular Ocular Motor Screening (VOMS; includes balance, vision and movement tests) and the Standardised Assessment of Concussion (SAC; includes questions relating to memory and cognitive function).
Red flags for emergency assessment
During the evaluation, identify if there are clinical features present that may be associated with more serious structural head or cervical spinal injuries or events (e.g. intracranial bleeding), which may require referral for emergency hospital assessment (Table 1).11, 13 A targeted clinical examination should be performed in all patients with suspected concussion in primary care, including assessment for:10
- Neurological abnormalities – primarily looking for marked motor or sensory deficits associated with cranial nerves C1 – C8
- Cervical spine tenderness on palpation and assess range of motion
- Skull fracture – a patient with an obvious scalp wound will usually have already sought medical attention, however, consider palpation to detect skull fracture, particularly depressed fractures
The comparative significance of red flags will likely depend on the patient’s specific characteristics, e.g. people aged ≥ 65 years or taking an anticoagulant are at elevated risk of intracranial bleeding.10 Any person who is not lucid or fully conscious should be assumed to have a more severe TBI or cervical spine injury until proven otherwise.13 While vestibular-dominant symptoms (e.g. dizziness and vertigo) commonly occur in people with concussion, benign paroxysmal positional vertigo (BPPV) should be considered as a differential diagnosis (or co-morbidity) if these symptoms are persistent.10 BPPV can be assessed using evaluations such as the Dix-Hallpike test or supine roll test.10
For further information on vertigo, see: “A delicate balance: managing vertigo in general practice”
Presentation may be delayed in some patients
A common misconception regarding concussion is that it always has an acute or early onset, with symptoms emerging minutes to hours after the causative event. However, concussion can sometimes present as an evolving injury with clinical features that change over time, e.g. symptoms may be more subtle or absent at first but develop or worsen after 48 – 72 hours.4 Delayed symptom reporting can sometimes occur if the person experienced other injuries during the incident (e.g. fractured shoulder) meaning that they were not engaging in daily activities and therefore were unaware of concussion symptoms until they returned to activity.
Given the range of factors that need to be considered, time can be a major limiting factor within a primary care consultation. BIST is a concussion screening tool developed by a group of New Zealand clinical experts, for use in people aged eight years and older when they present for medical care.15 This tool is designed to be completed in six minutes, and encompasses:
- Patient details and the injury context, e.g. date, time and mechanism of injury
- Ten key prognostic questions relating to clinical indicators that may suggest the person is at high risk of complications and requires hospital evaluation
- A 16-item symptom severity checklist, with associated recommendations for referral (e.g. to a specialist concussion service or physiotherapist), or primary care follow-up based on the cumulative score in accordance with threshold cut-offs.
 Practice point: Baseline scoring data obtained from an initial BIST assessment can be used to facilitate patient monitoring for improvement over time.
Practice point: Baseline scoring data obtained from an initial BIST assessment can be used to facilitate patient monitoring for improvement over time.
- An evaluation of the overall impact of the injury on the patient’s quality of life
To access BIST and a video walkthrough, visit: tbin.aut.ac.nz/support-and-resources/brain-injury-screening-tool-bist
Read the evidence supporting BIST
BIST was initially validated in a retrospective survey of 114 patients who had experienced a concussion, that demonstrated there was a strong correlation between the performance of BIST and other existing tools such as the Sports Concussion Assessment Tool-Fifth Edition (SCAT-5) and the Rivermead Post-Concussion Symptom Questionnaire (RPQ).16 Feedback from participants indicated that questions were straightforward to understand and allowed for further modifications to optimise readability for patients/caregivers.16 A subsequent analysis supported the findings that BIST is a psychometrically reliable measure of symptom burden following a concussion, and that raw scores can be used to inform clinical decisions.17
Why use BIST over other tools such as SCAT-5 and RPQ?
Prior to development of BIST, the most widely used clinical assessment tools in primary care included the SCAT-5 and the RPQ.16 Both encompass symptom scoring, neurocognitive and physical assessments, and red flag questions.16 However, neither tool provides guidance on health care pathway decision making. SCAT-5 is specifically designed for assessing sport-related concussion,* and RPQ is primarily intended for use in a research setting.16 In addition, the SCAT-5 tool cannot be performed correctly in less than ten minutes,13 and in some cases a comprehensive concussion assessment using either tool may take up to 30 minutes. Therefore, the SCAT-5 and RPQ tools are not ideally suited to the needs of clinicians in the context of a standard 15-minute appointment.
*SCAT-5 should still be used on the side-line for concussions sustained while playing sport if professional medical support is available. This tool is designed for use in people aged ≥ 13 years. For children aged < 13 years, the Child SCAT-5 should be used.
Diagnose concussion based on clinical judgement
Assessments such as BIST should be applied as support tools; they are not a replacement for clinical judgement, and should ideally be used together with other relevant questions and neurocognitive or physical assessments (as required).15 After more serious structural or brain injuries have been ruled out, a diagnosis of concussion can be made clinically, supported by evidence of a plausible mechanism of injury and symptoms/signs relating to altered brain functioning.10, 18 Ultimately, a diagnosis of concussion may not always be clear, regardless of the examiner’s skill or experience.18 N.B. Laboratory investigation or imaging is not indicated unless differential diagnoses are suspected.
Once a diagnosis has been made, clinicians should provide patients or parents/caregivers with education using language and examples that are understandable for their level of health literacy and culturally appropriate, including:10
- An explanation of what concussion is
- How concussion should be managed
- Expectations for the recovery timeframe and realistic functional goals
- Reassurance and information on the next follow-up step
Encourage patients to take an active role in self-management and recovery
It is essential that patients and their whānau/family have a suitable level of understanding about concussion so they can appreciate the importance of reporting emerging or worsening symptoms, and the value of adhering to the “rest to re-engagement” process (see: “Management centres around rest followed by re-engagement”).10 This is particularly important for athletes as surveys have shown that, despite having a baseline knowledge of the risks of playing sport with a concussion, some young adults will still display a willingness to do so.10 Providing written or printed recommendations is often a pragmatic strategy, particularly for patients experiencing short-term memory impairment.
For patient-specific online concussion resources, see:
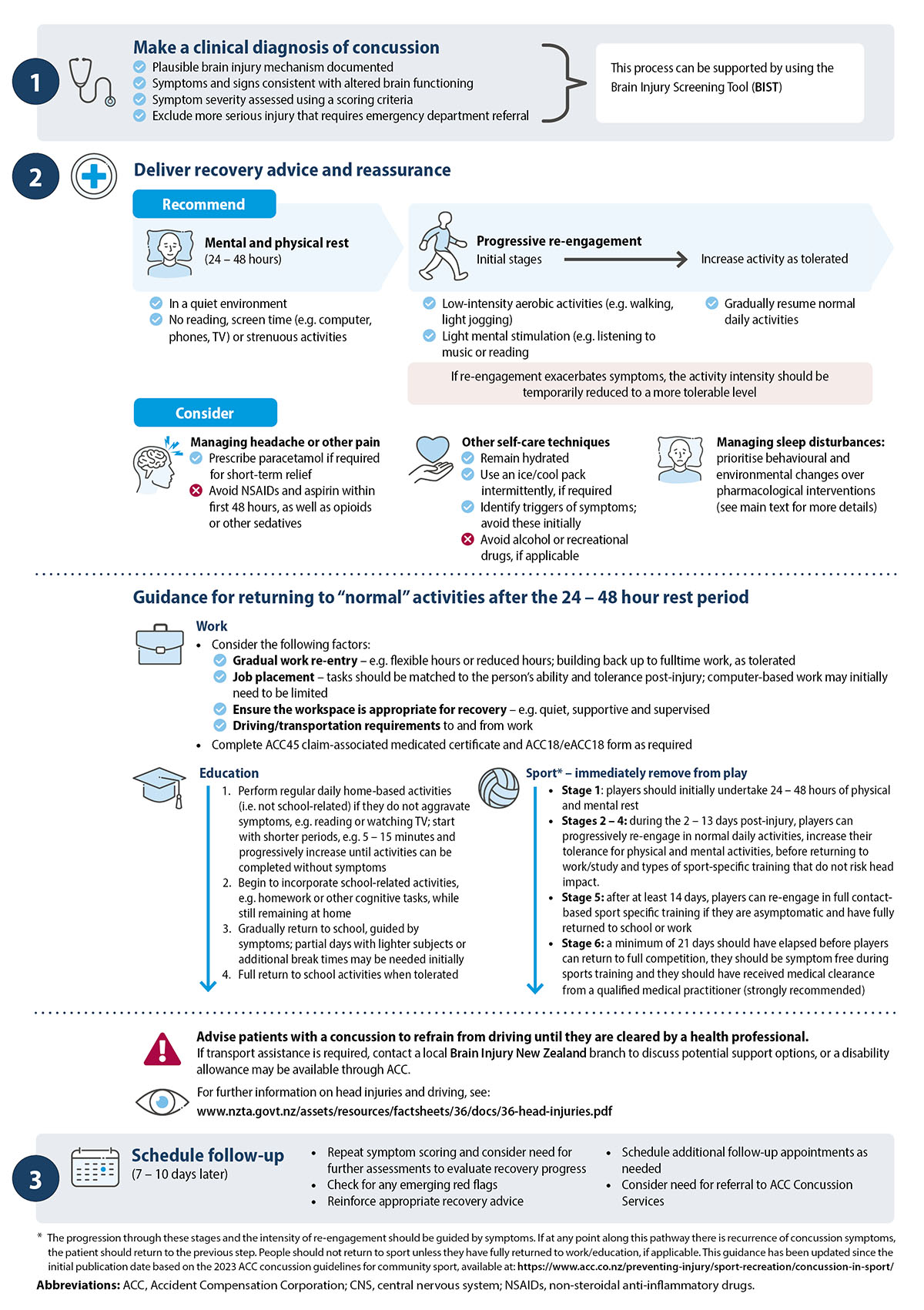
An overview of the specific recommendations and considerations relating to concussion management are detailed in Figure 2.
Immediate mental and physical rest (i.e. no reading, listening to music, watching TV) is essential after a concussion occurs to minimise brain energy demands and to allow time for functional recovery to begin.1 However, it is now accepted that excessive rest can impair recovery, and patients should be encouraged to gradually and progressively resume normal activities following an initial rest period assuming it is done in a way that does not cause or worsen symptoms (see Figure 2 and “Expert advice: the “+3 rule” for activity re-engagement” for more details).1, 10, 11 Randomised controlled trial (RCT) data has demonstrated that patients who undertake prolonged and strict rest for five days following a concussion recover more slowly than those who engage in some form of physical activity after 24 – 48 hours.11, 20
Progressive engagement in exercise following an initial rest period is proposed to help recovery through several mechanisms, such as:21
- Improving cerebral blood flow – this helps increase oxygen and glucose (energy) delivery to the brain for cellular repair
- Promoting the production of brain-derived neurotrophic factor (BDNF) – this is a protein that functions to support the survival of existing neurons and encourages the growth and differentiation of new neurons; the expression of BDNF is exercise-dependent, i.e. increasing the intensity of exercise (according to symptom tolerance) increases BDNF production
Expert advice: the “+3 rule” for activity re-engagement
A general approach for guiding activity re-engagement is to use the “+3 rule”. First ask the patient to give themselves a baseline symptom severity scoring on a 0 – 10 scale. After engaging in an activity, the patient should then rate their score again; if the severity of symptoms increases by three or more points compared with their baseline score, then the intensity of the activity should be temporarily decreased (or duration if already light intensity). If the activity can be completed without increasing symptom severity by three or more points, the level of challenge can be gradually increased on subsequent days and the rule applied again.
For example: if a patient with a baseline headache severity score of four takes a 20-minute walk and their perceived score changes to:
- Seven or more – they should decrease the intensity of their walk the next day or if it was already low intensity, reduce the duration, e.g. to 15 minutes, and then try to increase the intensity and/or duration on subsequent days, as tolerated (i.e. provided the symptom severity does not increase by ≥ +3)
- Six or less – they should increase the intensity of their walk the next day and continue to increase the intensity of their activity on subsequent days, as tolerated
Managing specific symptoms
Headache or other pain
Concussion symptoms should be expected to resolve without pharmacological intervention.11 If analgesia is required, prescribe paracetamol for short-term relief but warn patients that analgesic overuse can prolong or worsen concussion-associated headaches.1, 11 Recommend that patients avoid non-steroidal anti-inflammatory drugs (NSAIDs) including aspirin for at least the first 48 hours (due to bleeding risk) and opioids or other sedatives (due to masking central nervous system effects).1, 11
Sleep disturbances
Sleep disturbances are common in patients who have sustained a concussion, including both hypersomnia (more common in initial stages) and insomnia (more common in later stages).24, 25 Behavioural and environmental changes are recommended first-line, e.g. establishing a regular bedtime, avoiding prolonged daytime naps* and not consuming foods or drinks with stimulating effects prior to bedtime.25 If sleep disturbances persist for several weeks, further consultations as part of an overall cognitive behavioural therapy approach is preferred before considering short-term pharmacological options.24, 25
*Expert advice: daytime naps with a duration of < 40 minutes are acceptable in the early stages of recovery.
For further information on the management of sleep disturbances and insomnia, see:
Patients can be reassured that almost all people who experience a concussion fully recover. Data from New Zealand show that approximately half of people recover within two weeks of the injury, and almost all recover within two months.26 Good adherence to management advice and effective education about concussion enhances recovery time.1
Read the evidence
Until recently, international consensus statements consistently reported that most people display symptom resolution within 7 – 14 days.11, 22, 26. However, a 2020 prospective analysis of New Zealand data obtained over two years from 594 people with a sports-related concussion (mean age 20.2 ± 8.7 years), found that 45% exhibited clinical recovery within two weeks of the injury, 77% within four weeks and 94% within eight weeks.26 This analysis defined clinical recovery as being when the participant’s SCAT-5 symptom score/severity score was below a certain threshold.26 Further investigation is required to assess clinical recovery times in patients with concussion that are not sports-related.
What constitutes “clinical recovery” in primary care?
Differences in the estimates for recovery time between clinical studies is likely dependent on the criteria they use and population assessed.10, 26 In a general practice setting, clinical recovery from concussion can be defined as the patient having:
- Minimal symptoms that do not worsen with activity
- Resolution of any abnormal findings on clinical examination
- Exercise tolerance, e.g. the patient can exercise at 85% of their maximum heart rate* without exacerbating their symptoms
- Re-integration into “normal” activities (see: “Guidance for returning to “normal” activities”)
* This can be estimated by using the formula: maximum heart rate = 220 – patient age. For example, a 50-year-old patient would have an estimated maximum heart rate of 170 beats per minute (bpm); to demonstrate exercise tolerance, they would need to be able to exercise at approximately 145 bpm without their symptoms worsening.
Risk factors associated with prolonged recovery
Time to recovery varies between patients depending on a number of risk factors (many of which are pre-injury factors), including:10, 26–29
- Initial symptom burden (strong predictor), i.e. more severe acute symptoms correlate with a prolonged recovery.
- Previous concussions (strong predictor). Having a previous concussion increases the risk of sustaining future concussions and may be associated with more severe and protracted cognitive deficits if a subsequent one occurs. However, this may be influenced by whether the patient had not fully recovered from the previous concussion before experiencing the next.
- Pre-existing mental health conditions (strong predictor), e.g. anxiety, depression, Attention deficit hyperactivity disorder (ADHD). Pre-existing mood disorders may influence the evaluation of baseline cognitive functioning and make the interpretation of persistent concussion symptoms more difficult, leading to a prolonged recovery period.
- Being female. Females generally present with a greater cognitive deficit and overall symptom severity than males and longer time for recovery. The underlying reason for this is unknown.
- The presence of migraine-like symptoms or a history of migraine
- Younger and older age groups. There is inconsistent evidence to support age-dependent recovery times, however, some studies how shown that younger people (e.g. aged < 18 years) or older people (e.g. > 65 years) have a longer concussion recovery duration.
- People with alcohol and substance abuse issues
- Predominance of vestibular symptoms, e.g. dizziness and balance difficulties. This has been associated with poorer long-term outcomes in patients with concussion.
N.B. The mechanism of injury has not been demonstrated to be predictive of recovery time.10
Providing culturally appropriate care for Māori
Strategies relating to concussion management do not have to follow a “one-size-fits-all” approach. Education, management and service provision should be culturally responsive and for Māori patients in particular, focus on the Whānau Ora model, i.e. addressing individual needs in the context of their whānau as a whole.2 For example, consider how the concussion management advice of “rest to re-engagement” will impact on the role and responsibilities of the patient within their whānau and conversely, the important role that whānau has in providing strength and support for their recovery. This process may be aided by involving a Māori health provider in the care plan, and including relevant cultural practices into a tailored rehabilitation strategy (e.g. Rongoā Māori).2
ACC now funds Rongoā Māori30
Rongoā Māori is a term encompassing a range of techniques related to the traditional Māori approach to care and healing. Examples includes mirimiri (traditional massage/bodywork), rākau rongoā (native flora herbal preparations) and karakia (spirituality and prayer). The techniques associated with Rongoā Māori place a strong emphasis on spirituality and whānau connection, and can help promote restoration of hauora (wellbeing) and recovery through mana motuhake (self-determination).
ACC now funds Rongoā Māori in conjunction with other treatment or rehabilitation approaches, depending on a patient’s needs. This is funded under the social rehabilitation category, which is considered separate from treatment, and directed at helping patients return to independence in activities meaningful to their life/wellbeing. Clinicians wanting to personally deliver Rongoā Māori services must register with ACC as a vendor; a list of ACC-registered Rongoā Māori practitioners is available on the ACC website.
For further information on accessing Rongoā Māori services, see: www.acc.co.nz/im-injured/what-we-cover/using-rongoaa-maaori-services/ or discuss this process with the ACC Recovery team member managing the particular claim.
After diagnosing concussion and establishing a recovery plan (see: Guidance for return to “normal” activities), it is recommended that patients should be followed up in primary care within 7 – 10 days to re-evaluate their clinical status and adjust their rehabilitation protocol if necessary (Figure 2).1 This process should ideally involve repeating the use of a symptom scoring tool (e.g. BIST) to quantify any changes against their baseline level, continued guidance relating to the management of specific ongoing symptoms and assessment for the emergence of red flags.1 Further follow-up consultations can then be scheduled as needed depending on recovery progress.
ACC Concussion Service Referral
The ACC Concussion Service is intended for people with mild to moderate traumatic brain injuries who are not recovering as expected following an accident and have risk factors predictive of a prolonged recovery.
Assuming a patient presents within the first few days of their injury to primary care, they should generally not be referred to ACC Concussion Services at the first assessment as symptoms will often resolve after 7 – 14 days. There are risks associated with early referral and escalation of treatment; in particular, this course of action may worsen a patient’s perception of concussion and therefore create mental barriers to recovery.1 However, referral should be considered if:
- Symptoms have not improved at follow-up appointments and are impacting on the person’s ability to do everyday activities e.g. impacting return to school or work
- More than 14 days has passed since the injury when the patient first presents to primary care and symptoms have not improved
As of 1st July, 2023, primary care clinicians (and other providers) referring patients to ACC Concussion Services no longer have to seek prior approval from ACC. The referral can be sent directly to a concussion provider of choice. For a list of providers in your area, click here.19 ACC and Service providers are responsible for co-ordinating interdisciplinary management, which can be tailored to a patient’s specific symptom profile, and may include behavioural, vestibular, vision-oculomotor and cognitive rehabilitation interventions.10, 19
After sustaining a concussion, a significant concern for many people is “when can I return to my normal routine?”. While this question sounds simple, the answer is complex as it depends on what their normal activities involve, the degree of physical, cognitive and emotional impairment caused by the concussion, and their adherence to recovery advice.1 One of the main priorities when considering a return to work, education, sport or general independence is avoiding any additional brain injury events; these may be tolerated in people without a previous concussion but even minor accidents can exacerbate the already vulnerable neuronal tissue in people with a history of concussion.1 As such, any safe return to “normality” should involve appropriate restrictions and limitations, which are progressively withdrawn in accordance with documented symptomatic improvement.1 This journey will be unique for each person, and the way with which health professionals engage in this conversation can have a significant impact on the rehabilitation outcome.1
Return to work
People with concussion who return to work have an improved recovery, social integration, financial stability and overall quality of life compared with those who remain out of work.31 Therefore, an early return to some form of vocational engagement following the compulsory 24 – 48 hour rest period should be a priority for most employed people who have a concussion, assuming the work environment or duties does not put them or others at risk of injury.1 Those with jobs that exclusively involve driving (e.g. courier drivers, truck drivers) are likely be fully unfit for work following a concussion while they have any ongoing symptoms that affect their vision, ability to promptly make decisions or react.23
There can be various barriers to a successful return to work plan. In particular, fatigue and residual concentration or memory problems are common concussion-related symptoms that can limit vocational engagement; finding the right balance between beneficial and detrimental mental stimulation can be challenging.1 Factors to consider when discussing a return to work are detailed in Figure 2, but each plan needs to be individualised depending on the type of work and the support provided by employers.1 Patients who have been referred to ACC concussion services may be eligible for assistance from an occupational therapist who can help to identify suitable duties and workplace modifications.
A module on certifying work capacity after injury is available from: https://www.goodfellowunit.org/group/76
Medical certificates
General practitioners and nurse practitioners can provide patients with a medical certificate as part of an ACC45 injury claim to cover the initial 24 – 48 hours rest period when they are fully unfit for work, up to a maximum of 14 days, as needed. An ACC18/eACC18 form can also be submitted at the initial consultation to state whether a patient needs to reduce their hours or change the type of activities they in engage in upon their return to work as part of their rehabilitation for up to 14 days. If the patient is still recovering and continued limitations are required beyond this initial timeframe, another ACC18/eACC18 form should be completed to confirm they are still only fit for selected work, and ideally include a specified timeframe for further review or return to normal duties.
For further information, see: www.acc.co.nz/for-providers/treatment-recovery/medical-certificates-return-to-work/
Return to education
While early mental overexertion can worsen symptoms in people with concussion and potentially prolong recovery, a return to studies should not be excessively delayed.32 Most students should be able to return to study within two to four days following the strict rest period,10 however, the timeframe will be variable depending on individual factors, and activity restrictions will likely be required initially (detailed in Figure 2).22, 32
Return to sport
People with a suspected or confirmed sports-related concussion should be immediately removed from play (regardless of their level of participation) and must complete a 24 – 48 hour physical and mental rest period before commencing a graduated return to play protocol.11, 33 Individual sporting authorities have different regulations for timeframes and criteria for a graduated return to sport (see below), however, most advise avoidance of contact sports for at least two to three weeks, with some recommending a longer duration, e.g. Rugby. Return to sport should not occur until a person has been medically cleared as being asymptomatic, and has fully returned to work/education, if applicable.22
A generalised graduated return to play protocol is detailed in Figure 2.11, 33
For sport-specific return to play guidance, refer to individual sporting bodies, e.g.:
Update: 2023 ACC concussion guidelines for community sport now available
In late 2023, ACC, in partnership with seven national sporting organisations, released new guidelines on the recognition and treatment of concussion for people participating in community sport. This framework is intended to help foster a consistent standard of care, irrespective of the sporting discipline.
The guidelines include a six-stage graduated return to education/work and sport protocol, recommending that:
- Stage 1: players should initially undertake 24 – 48 hours of physical and mental rest
- Stages 2 – 4: during the 2 – 13 days post-injury, players can progressively re-engage in normal daily activities, increase their tolerance for physical and mental activities, before returning to work/study and types of sport-specific training that do not risk head impact. The progression through these stages and the intensity of re-engagement should be guided by symptoms.
- Stage 5: after at least 14 days, players can re-engage in full contact-based sport specific training if they are asymptomatic. Players must have fully returned to school or work before returning to contact-based training.
- Stage 6: a minimum of 21 days should have elapsed before players can return to full competition, they should be symptom free during sports training and they should have received medical clearance from a qualified medical practitioner (strongly recommended)
For the full ACC guidelines, see: https://www.acc.co.nz/preventing-injury/sport-recreation/concussion-in-sport/
Full recovery can be expected in the majority of patients who sustain a concussion, however, a small number report continuing symptoms that impair their daily functioning and quality of life.34
The phrase “persistent concussion symptoms” is preferred to describe symptoms that are present beyond three months of a patient sustaining a concussion, e.g. fatigue, headache, concentration/memory impairment.34 Estimates of the prevalence of persistent-concussion symptoms vary substantially in the literature depending on the diagnostic criteria, population and timing of assessment;34 in some cases, patients may have displayed initial clinical recovery and returned to their “normal” routine, yet report persistent concussion symptoms at a later date.
Historically, the persistence of symptoms for longer than three months was referred to as “post-concussion syndrome”.34 However, the use of this term is controversial, particularly because:34
- The symptoms do not always cluster in a predictable pattern; persisting individual symptoms are more commonly reported than combinations, and there are no universally accepted criteria for a diagnosis
- The symptoms are not specific to concussion, and are also reported in more severe TBIs, other non-brain injured patients and in otherwise healthy people*
- This term implies a mechanism of persisting neuronal damage, however, the pathophysiology is debated and not strongly supported in the literature
- Reporting may be influenced by a number of factors, such as recall bias, misattribution of pre-existing symptoms, personal beliefs about the injury, malingering and exaggeration
*It has been reported that if the pre-requisite of having actually experienced a concussion event is excluded, up to half of all people in general, and 70 – 80% of people with depression or chronic pain, would meet the definition of “post-concussion syndrome”.34
As a result of these limitations, the Diagnostic and Statistical Manual (DSM-5) of the American Psychiatric Association (APA) and International Classification of Diseases 11th Revision (ICD-11) no longer recognise post-concussion syndrome as a diagnostic entity. Consistent with this stance, ACC no longer accepts post-concussion syndrome as a diagnosis for brain injury or its subsequent symptoms. If a Read Code is required for patients with persistent concussion symptoms, use either the “concussion” (S60..) or “head injury” codes (S646.). For further information on Read Codes, see: www.acc.co.nz/for-providers/lodging-claims/read-codes/.
To read the ACC position statement on post-concussion syndrome/persistent concussion symptoms, see: https://www.acc.co.nz/assets/Uploads/Post-concussion-syndrome-ACC-position-statement.pdf
Addressing persistent concussion symptoms
The presence of persistent concussion symptoms is likely dependent on a complex interplay of biological, psychological and social factors, and the evidence for effective treatment is limited.34
In patients with symptoms that persist for longer than three months:1, 19
- Discuss social support mechanisms and potential stressors in the environment in which the patient is recovering, i.e. unstructured household, unsupportive workplace, financial stress
- Reconsider differential diagnoses outside of the injury-context; symptoms may be occurring independently of the concussion or worsen due to its presence, e.g. chronic pain, anxiety and depression disorders, sleep disorders and other psychiatric conditions
- Assess current medicine use, including prescription, over-the-counter medicines or supplements, as well as alcohol or recreational drug use
Further assessment may be warranted. If this process does not uncover a potential cause, an additional and more comprehensive neuropsychological and/or neurological assessment(s) is generally indicated for patients with persistent concussion symptoms.19, 22, 34 This differs from the brief neuropsychological assessment used in evaluation tools, and will likely require an interdisciplinary approach (e.g. with a clinical neuropsychologist) to address the more complex aetiology underpinning the patient’s condition.19, 22
Neuropsychological assessments through ACC: For patients who have been referred to ACC concussion services, neuropsychological screening is included as part of the management pathway.19 When conducted, a brief summary (including recommendations) must be shared with the interdisciplinary team and ACC.19
Recurrent concussions and the risk of future cognitive or neuropsychological deficits
While concussions have traditionally been thought to cause only limited and transient behavioural changes, there is increasing evidence of an association between sustaining multiple concussions and having cognitive or neuropsychological deficits later in life.11 When neurodegenerative changes occur in a specific progressive pattern, it is termed chronic traumatic encephalopathy (CTE).35 However, a confirmed link between concussion and CTE has not been established.11
Read the evidence
Investigations into the relationship between multiple concussions and cognitive or neuropsychological deficits later in life are ongoing. An analysis of 2,552 retired professional American football players found that those who had sustained more than three concussions had a five-fold higher prevalence of diagnosed mild cognitive impairment and a three-fold higher prevalence of reported significant memory problems compared with those without a history of concussion.36 While an increased rate of Alzheimer’s disease was not identified, an earlier onset was reported among former players with recurrent concussions.36 In addition, a prospective analysis of > 350,000 United States Military Veterans demonstrated those who had sustained one or more concussion (with or without loss of consciousness) had more than a two-fold higher risk of being diagnosed with dementia.37 The risk was higher in those who had sustained multiple concussions, and the association was present even after adjusting for medical and psychiatric co-morbidities.37
There is currently insufficient evidence to define a causal relationship between multiple concussions and CTE. CTE can only be diagnosed according to specific pathology criteria detected in autopsied brains; there is no validated clinical criteria for diagnosing CTE in a living person.35 While there is a correlation between sustaining multiple concussions and an increased risk of developing CTE, most studies involve post-mortem study of professional athletes who regularly engaged in high impact activities throughout their life, e.g. American Football players.35 Further investigation is warranted to understand this potential relationship further, e.g. whether it is a causative association and, if so, to quantify the relative contribution of concussion in the context of other modifiable risk factors.
For further information on concussion:
