Pain is an individual experience influenced by the patient’s perception, history and expression of pain, e.g.
ability to cope, mental wellbeing, previous experience of pain, communication skills, family or cultural background.
Key questions for the patient when assessing pain are:
- How severe is the pain and what does it feel like?
- Where does the pain occur, how often is it occurring, and is it radiating?
- When did the pain start?
- What alleviates the pain?
- What makes the pain worse?
A verbal descriptor, e.g. none, mild, moderate, severe or excruciating, or a numerical scale, e.g. zero (none) to ten
(worst pain imaginable), are useful methods to quantify the level of pain, and how it is progressing. A visual tool such
as the Faces Pain Scale may be more appropriate for children, people with cognitive difficulties and people who do not
speak English.1
The Faces Pain Scale for children is available from:
https://www.iasp-pain.org/Education/Content.aspx?ItemNumber=1519
The primary aim of acute pain management* is to provide treatment that reduces the patient’s pain, with minimal adverse
effects, while allowing them to maintain function.
A secondary aim is to prevent acute pain from progressing to chronic pain.
* After treating the underlying cause of the pain, where possible
It is important that patients have a realistic expectation of what their pain management strategy will achieve – an
analgesic regimen that removes all experience of pain is usually not possible. Discuss with the patient that analgesic
medicines will reduce their amount of pain to a manageable level, although it may take some time initially to get the
dose right. The effectiveness of an analgesic regimen can be attributed to not only the pharmacological effects of the
medicine, but also to the awareness that pain is being treated and the routine of taking medicines (a placebo component).1
Patients can be reassured that their pain is expected to improve with time (try to give a likely duration for this)
and their requirements for medicines will decrease. Explaining that medicines for acute pain are for short-term use only
and setting a plan for decreasing doses and strengths can help to avoid inappropriate use of opioids and acute pain becoming
chronic.
Anxiety, depression, stress, insomnia and catastrophising increase the likelihood that acute pain will become chronic,
particularly post-surgery; patients who display any of these features will require additional reassurance that their pain
is being managed and is expected to resolve. For patients with acute low back pain in particular, psychosocial and occupational
factors, e.g. dissatisfaction with their job, are associated with progression from acute to chronic pain; identify factors
early for intervention.
Regular assessment of pain improves management and outcomes
Patients prescribed analgesics for acute pain should be followed up regularly to ensure that their pain is resolving and their
medicine requirements are diminishing. Pain that is unable to be managed or that increases in intensity warrants consideration
of other causes, e.g. surgical complication, infection or an alternative diagnosis, e.g. neuropathic pain.
A pharmacological treatment regimen for acute pain can be based on the WHO analgesic ladder
The World Health Organisation (WHO) analgesic ladder is widely accepted for the management of nociceptive pain.2 In
patients with acute pain the ladder is generally used in reverse, e.g. in severe acute pain, begin with morphine at Step
3, then as the pain resolves, reduce to codeine at Step 2, and continue with paracetamol at Step 1 until pain is negligible
(Figure 1).3 Adjuvant treatments, e.g. physiotherapy or non-analgesic medicines, are continued throughout
treatment, as appropriate.
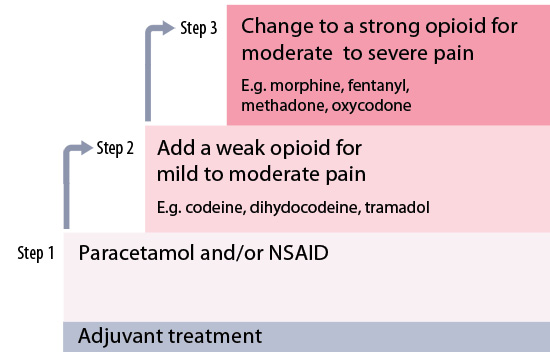
Figure 1: The WHO analgesic ladder of medicines
Response to analgesia is variable, so an analgesic regimen needs to be individualised
There are many reasons why individual patients will respond differently to a standard dose of an opioid, including their
level of pain, renal function, co-morbidities, co-prescribed medicines and genetics. CYP2D6 polymorphisms, i.e. people
who are fast or slow metabolisers of CYP2D6 enzymes, affect plasma concentrations of codeine and tramadol (and to a lesser
extent, oxycodone) and either increase adverse effects or decrease effectiveness.
Therefore, doses of opioids should be individualised, within recommended ranges, according to the patient’s particular
clinical circumstances. In a primary care setting, oral forms of analgesia are preferred and it is usually recommended
to begin with regular use of short-acting preparations, while establishing opioid requirements, then consider switching
to a controlled release formulation.3, 4
Consider appropriate dose reductions in elderly or frail patients, but do not under treat pain.
Multi-modal analgesia improves acute pain management
Multi-modal analgesia refers to the concurrent use of analgesics with different modes of action, e.g. paracetamol or
a NSAID used with an opioid. Multi-modal regimens result in improved pain relief, compared to monotherapy, and consequently
a reduction in the opioid dose required, as well as a reduced risk of adverse effects.1, 5 Multi-modal analgesia
also provides patients with reassurance that they will have pain relief as treatment is de-escalated. For example, a patient
is initially prescribed codeine, paracetamol and ibuprofen; they are advised to continue treatment with paracetamol and
ibuprofen while the dose of codeine is reduced and then withdrawn, then the dose of the NSAID is reduced and withdrawn,
and finally, when the pain is considered to be negligible the paracetamol is withdrawn.
Consider the need for additional medicines such as laxatives, anti-nausea and gastro-protection
A laxative should almost always be prescribed if a patient is going to be taking opioids for more than a few days.
Nausea and vomiting associated with opioids is usually dose-related. If adverse effects are intolerable, and pain relief
is not adequate if the dose of opioid is lowered or the patient is switched to a different opioid, then consider adding
an anti-nausea medicine such as prochlorperazine, cyclizine or metoclopramide.
A proton pump inhibitor may be required for patients prescribed a NSAID who are at risk of gastrointestinal complications.
Additional medicines may be required if there is a neuropathic component to the patient’s pain, e.g. tricyclic antidepressants
(TCAs), gabapentin or pregabalin.
For further information see: “Managing patients with neuropathic pain” www.bpac.org.nz/BPJ/2016/May/pain.aspx
Provide patients with a written analgesia plan, accompanied by a verbal explanation of the instructions.
A pain management regimen often consists of multiple medicines that have to be administered at different times and at
different doses. Patients or their caregivers need to be able to clearly understand their plan, keep track of their medicines
and know what they have taken, when they can take the next dose, and when to stop.
A written analgesia plan ensures that patients know their medicine regimen, and it can help to minimise medicine errors
and optimise pain management with regular, adequate dosing.
The most important aspects to include in an analgesia plan are:
- The regular dose, frequency and dosing interval for each medicine, including extra doses that could be taken for breakthrough
pain
- Adverse effects that may occur and how these should be managed, e.g. reducing the dose, taking with food or seeking
medical advice
- The likely timeframe for pain resolution and instructions on how to reduce the dose and stop medicines as pain improves
Depending on the specific clinical circumstances, non-pharmacological treatments, e.g. elevation of an injured leg,
and treatment goals, e.g. walking to the letterbox at the end of the first week following surgery, could also be included
in the patient’s plan.
An example of an analgesic plan is available here:
www.guild.org.au/__data/assets/pdf_file/0017/6209/patient-resource-my-pain-management-plan-nps-medicines-wise4e0a9a33c06d6d6b9691ff000026bd16.pdf
Depending on the cause for the pain, physical interventions such as exercise, physiotherapy and heat application
may be appropriate alongside the pharmacological regimen
A variety of non-pharmacological interventions may be beneficial for patients with acute pain, depending on the cause.
For example:1
- Referral to a physiotherapist following a soft tissue helps to maintain movement, slow muscle de-conditioning and
may avoid further injury
- Exercise, staying active and application of heat can improve outcomes in acute low back pain
- Yoga may improve back pain and enhance mindfulness6
- Massage may improve sleep in patients with musculoskeletal pain
- A heat pack on the lateral abdomen or lower back may provide relief for patients with renal colic7
There is limited evidence to support the use of transcutaneous electrical nerve stimulation (TENS) or acupuncture in
the management of acute pain, however, as there are significant placebo affects associated with pain interventions some
patients may find these to be effective.8
Psychological distraction techniques such as listening to music can lead to better pain management outcomes
There is a significant psychological component to managing pain. Patients who are able to maintain a positive attitude
towards recovery and are proactive in achieving treatment goals are likely to have better outcomes, and less likely to
progress to chronic pain.
An important aspect of managing pain is to avoid a constant focus on its presence. Distraction techniques include listening
to music, reading, meditation or mindfulness exercises or any other activity that is enjoyable, but does not exacerbate
pain.
