Published: July, 2023 | Review date: July, 2026
This audit helps primary care health professionals optimise
the management of patients prescribed opioid medicines
in their practice. The aim is to ensure that patients who have
been using these medicines long-term for the treatment
of non-cancer pain have their medicine regimen regularly
reviewed, in order to determine if ongoing use is appropriate;
withdrawal can be discussed with patients for whom ongoing
use is not indicated. Patients using these medicines for the
management of pain associated with cancer or other palliative
care conditions are not covered by this audit. Clinicians could
also use the audit to assess other medicines used long-term
for the management of chronic pain, such as gabapentin.
Strong opioid medicines are recommended at Step Three of
the World Health Organisation pain ladder, and are typically
reserved for the treatment of severe acute pain or moderate
to severe chronic pain, depending on a patient’s response
to other analgesics. There are few situations when a strong
opioid would be initiated for acute pain in primary care. More
common scenarios for general practitioners are renewing
a prescription of a strong opioid medicine for patients
discharged from hospital, renewing prescriptions of strong
opioids for patients with chronic pain managed in primary
care or initiating or renewing prescriptions of weaker opioids
such as tramadol or codeine.
Opioid medicines are potentially addictive. Dispensing data
from New Zealand show that between 2017 and 2021, almost
one-fifth of the population received an opioid medicine each
year. Discussions regarding addiction to opioid medicines
are often focused on strong opioids such as oxycodone,
however, the same prescribing cautions should be applied
to weaker opioids, such as tramadol, to minimise the risk of
inappropriate use. Dispensing data from New Zealand show
that while weaker opioid use declined slightly between 2017
and 2020, there was an increase in dispensings in 2021.1
For further information on New Zealand trends in opioid
use, see: bpac.org.nz/2022/opioids.aspx
Patients using opioid medicines should be encouraged to
adopt and continue with non-pharmacological approaches
to managing pain, such as exercise, physiotherapy and
relaxation/behavioural techniques. Clinicians can consider
the use of multimodal analgesia, such as using paracetamol
in combination with an opioid medicine, in order to reduce
the dose of opioid medicines required and therefore reduce
a patient’s risk of adverse effects, as well as provide analgesia
when the opioid medicine is withdrawn.
Clinical guidelines recommend that patients should be
reviewed within one to four weeks of initiating an opioid
medicine or increasing dose, as patients can become
dependent as early as one month after initiating opioid
medicines.2, 3 For patients using these medicines longterm, review on a three-monthly basis is recommended (or
more often if required).3
Reviewing patients using opioids
long-term can ensure that the medicines and doses they
are prescribed are still appropriate for their underlying
condition and degree of pain they experience, as well as
allowing the opportunity to assess for the development of
potential adverse effects.
Withdrawing patients who have become dependent on
opioid medicines can be a difficult process, particularly if this
is being managed in primary care without the patient having
access to additional support from addiction services or a pain
clinic in secondary care. The focus of this audit is on identifying
patients who are using opioids long-term and ensuring they
are reviewed. Withdrawing patients from opioid medicines is
not included in the audit process.
For further information on withdrawing patients who are
dependent on opioid medicines, see: bpac.org.nz/BPJ/2014/
October/opioid-addiction.aspx
Summary
This audit identifies patients who have been prescribed
an opioid medicine for three months or more in order to
assess whether the choice of medicine(s) and doses remain
appropriate.4
Recommended audit standards
Ideally, all patients who have been taking an opioid medicine
for the management of non-cancer pain for three months or
more should have a documented discussion in their notes
about the intended duration of opioid medicine use and a
plan for withdrawal. This could also include whether the
addition of another analgesic medicine is appropriate in order
to reduce the dose of opioid medicine(s) required or whether
switching to another analgesic medicine is appropriate. If
there is no documented evidence of a discussion, the patient
should be flagged for review.
Eligible patients
All patients who have been prescribed an opioid medicine for
three months or more are eligible for this audit.
Identifying patients
You will need to have a system in place that allows you to
identify eligible patients. Many practices will be able to
identify patients by running a “query” through their PMS. The
notes of identified patients will need to be reviewed in order
to ascertain the clinical indication for opioid prescription;
patients using opioid medicines to manage pain associated
with cancer or another palliative care condition can be
excluded from the audit.
Sample size
A sample size of 30 patients is sufficient for the purpose of the
audit. However, it is recommended that all eligible patients
using opioid medicines long-term for the management of
non-cancer pain are subsequently reviewed.
Criteria for a positive outcome
A positive result is achieved if a patient who has been
prescribed an opioid medicine for three months or more
has a documented discussion in their notes regarding their
pain management plan. This discussion could include the
expected duration of use of opioid medicines, the use of other
analgesics which could be used in combination with opioids
to help patients manage their pain, non-pharmacological
strategies for pain management and whether withdrawing
from an opioid medicine is appropriate or has been attempted.
During the review, clinicians can consider factors such as:
- Has the patient’s underlying condition changed, e.g. is a greater or lesser extent of pain relief required?
- Is the prescribed opioid medicine still the most appropriate choice?
- Should doses be adjusted or other non-opioid analgesics initiated?
- Should the patient be referred for additional support for non-pharmacological pain management, e.g. to a physiotherapist?
- Does the patient require assistance from addiction services?
Data analysis
Use the sheet provided to record your data. The percentage achievement can be calculated by dividing the total number of patients currently prescribed an opioid medicine for the management of non-cancer pain relief for three months by the number of patients who have a documented pain management plan discussion in their notes.
References
- Pharmaceutical Claims Collection, Ministry of Health, 2022.
- Manchikanti L, Kaye AM, Knezevic NN, et al. Responsible, safe, and effective prescription of opioids for chronic non-cancer pain: American Society of Interventional Pain Physicians (ASIPP) guidelines. Pain Physician 2017;20:S3–92
- Centers for Disease Control and Prevention. CDC Guideline for
Prescribing Opioids for Chronic Pain — United States, 2022. Available
from: https://www.cdc.gov/mmwr/volumes/71/rr/rr7103a1.htm (Accessed May, 2023).
- If this audit is used to identify patients taking other analgesic
medicines long-term, such as gabapentin, clinicians can choose a
timeframe appropriate for the medicine in question
Clinical audits can be an important tool to identify where gaps exist between expected and actual performance. Once completed, they can provide ideas on how to change practice and improve patient outcomes. General practitioners are encouraged to discuss the suitability and relevance of their proposed audit with their practice or peer group prior to commencement to ensure the relevance of the audit. Outcomes of the audit should also be discussed with the practice or peer group; this may be recorded as a learning activity reflection if suitable.
The Plan, Do, Study, Act (PDSA) model is recommended by the Royal New Zealand College of General Practitioners (RNZCGP) as a framework for assessing whether a clinical audit is relevant to your practice. This model has been widely used in healthcare settings since 2000. It consists of two parts, the framework and the PDSA cycle itself, as shown in Figure 1.
1. The framework
This consists of three questions that help define the “what” and “how” of an improvement project (in this case an audit).
The questions are:
- "What are we trying to accomplish?" – the aim
- "How will we know that a change is an improvement?" – what measures of success will be used?
- "What changes can we make that will result in improvement?" – the concept to be tested
2. The PDSA cycle
This is often referred to as the “engine” for creating, testing and carrying out the proposed changes. More than one cycle is usually required; each one is intended to be short, rapid and frequent, with the results used to inform and refine the next. This allows an ongoing process of continuous learning and improvement.
Each PDSA cycle includes four stages:
- Plan – decide what the change to be tested is and how this will be done
- Do – carry out the plan and collect the data
- Study – analyse the data, assess the impact of the change and reflect on what was learned
- Act – plan the next cycle or implement the changes from your plan
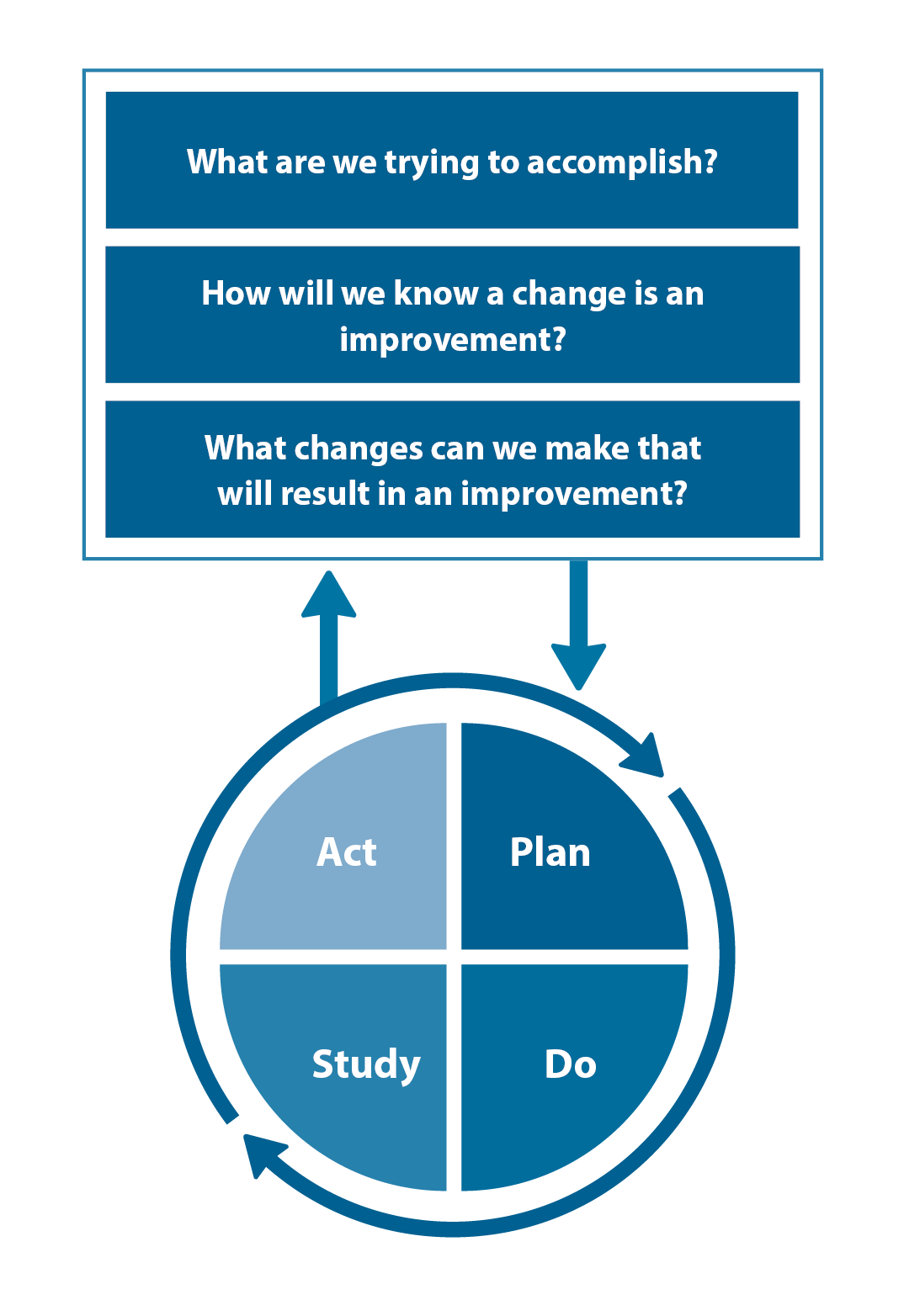
Figure 1. The PDSA model for improvement.
Source: Plan, Do, Study, Act (PDSA) cycles and the model for improvement

Claiming credits for Te Whanake CPD programme requirements
Practice or clinical audits are useful tools for improving clinical practice and credits can be claimed towards the Patient Outcomes (Improving Patient Care and Health Outcomes) learning category of the Te Whanake CPD programme, on a two credit per learning hour basis. A minimum of 12 credits is required in the Patient Outcomes category over a triennium (three years).
Any data driven activity that assesses the outcomes and quality of general practice work can be used to gain credits in the Patient Outcomes learning category. Under the refreshed Te Whanake CPD programme, audits are not compulsory and the RNZCGP also no longer requires that clinical audits are approved prior to use. The college recommends the PDSA format for developing and checking the relevance of a clinical audit.
To claim points go to the RNZCGP website: www.rnzcgp.org.nz
If a clinical audit is completed as part of Te Whanake requirements, the RNZCGP continues to encourage that evidence of participation in the audit be attached to your recorded activity. Evidence can include:
- A summary of the data collected
- An Audit of Medical Practice (CQI) Activity summary sheet (Appendix 1 in this audit or available on the
RNZCGP website).
N.B. Audits can also be completed by other health professionals working in primary care (particularly prescribers), if relevant. Check with your accrediting authority as to documentation requirements.
