Pain is a subjective experience and its perception is influenced by a complex web of biological, psychological and social factors.1 Acute pain is often linked to a specific injury or condition; the clinical course is usually predictable and temporary, with management tailored to its severity and cause.2 In contrast, chronic pain is a far more complex clinical scenario that can be caused by a number of factors, including sub-optimal management of acute pain by the patient and/or clinician. It is estimated that one in five adults in New Zealand are affected by chronic pain.3 Chronic pain is broadly defined as pain lasting more than three months and can be further classified as being either:4
- Chronic primary pain – the cause of pain is uncertain, or it appears to be disproportionate to any observable injury or condition
- Chronic secondary pain – pain is caused by an underlying condition, e.g. rheumatoid arthritis, osteoarthritis, endometriosis, ulcerative colitis
For further information on pain perception, including the distinct mechanisms that underpin acute and chronic states, see: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6650904/
In primary care, clinicians are often faced with the difficult task of interpreting whether a reported degree of distress or disability justifies initiation, continuation or escalation of pharmacological treatment. Often, such decisions depend on using clinical judgement to balance patient perceptions against their clinical and social history, as well as potential risk factors that may impact on treatment selection.
The World Health Organization (WHO) analgesic ladder
The WHO analgesic ladder is a widely used framework for the management of nociceptive pain.5, 6 Most patients can be prescribed Step 1 medicines (e.g. paracetamol and/or non-steroidal anti-inflammatory drugs [NSAIDs]).5, 6 If necessary, “weaker opioids” such as codeine and tramadol can be added which are at Step 2, while “stronger opioids” such as morphine and oxycodone are Step 3 on the analgesic ladder.5, 6 Each step of management can be supported by adjuvant treatments where applicable, e.g. non-analgesic medicines such as tricyclic antidepressants, as well as non-pharmacological interventions, e.g. heat/cold, relaxation and behavioural techniques.5, 6
Subsequent revisions to the WHO analgesic ladder:5, 6
- Emphasise a bidirectional approach to pain management, i.e. escalating treatment to effectively manage pain, then de-escalating to lower steps when practically possible
- Distinguish between acute and chronic pain management – stronger analgesics (weak and strong opioids) are often used first for acute pain and the patient progressively steps down treatment, whereas patients with chronic pain should start on Step 1 (non-opioid analgesics) and move upwards, as required
- Include an additional step to encompass the numerous other procedures available for the treatment of persistent pain, e.g. neurosurgical interventions, neuromodulation strategies, nerve blocks
Indications and cautions for opioid use
Despite the hierarchical approach outlined in the WHO analgesic ladder, opioids are still widely and inappropriately prescribed (and requested).7 While these medicines can be highly effective at alleviating moderate to severe acute pain, there is no compelling evidence that opioids are effective for the management of chronic primary pain.4 In addition, regular opioid use is associated with an increased risk of:7
- Adverse effects, e.g. cognitive impairment, respiratory depression (including fatal opioid-induced ventilatory impairment), sleep apnoea, increased risk of falls and fall-related injuries, depression, hypotension, bradycardia and multiple gastrointestinal effects, e.g. nausea, vomiting, bloating, constipation and in severe cases bowel impaction or perforation
- Dependence, tolerance and opioid-induced hyperalgesia due to neuroadaptation
- Misuse and death
Indications for opioid prescribing include:2, 4, 7
- Moderate to severe acute pain following surgery or injury (short-term use preferred)
- Moderate to severe cancer-related pain or pain associated with terminal-conditions (palliative care)
- Moderate to severe chronic non-cancer pain for selected patients in whom pain cannot be controlled despite the use of non-opioid analgesics/other non-pharmacological interventions, and which is adversely affecting functioning and quality of life (short-term or intermittent use preferred). The decision to initiate longer periods of opioid use should only be made when there is a documented benefit (e.g. improvements in pain score or function) that outweighs potential harms, and ideally be made in consultation with a multi-disciplinary pain management team*.
*This recommendation is based on evidence from clinical trials, however, we acknowledge that it is not always practical due to resource limitations.
If opioids are indicated, they should be prescribed at the lowest potency and dose to adequately manage pain, for the shortest possible duration, with a preference for immediate release formulations, and in combination with non-opioid analgesics (see: “Key recommendations for opioid prescribing”).7 There are limited situations where strong opioids should be initiated for the management of acute pain in primary care; community use most commonly involves renewing such prescriptions for patients who have been discharged from hospital. This scenario can be a source of frustration for primary care clinicians who must determine if there is an ongoing need, and if not, gradually attempt to safely withdraw these medicines in patients who may have developed opioid dependence.
The risk of long-term opioid use increases:8
- With each additional day of use beyond Day 3; there are marked increases in risk at around Days 5 and 31 of treatment
- When the initial prescription is for a period exceeding 10 days
- When repeats are included in a first prescription or a second prescription is given
Key recommendations for opioid prescribing 2,4,7
- Establish a treatment plan when initiating an opioid, including measurable goals and the timeframes for achieving these, information about adverse effects and a plan to stop use. This jointly agreed plan can be verbal, but it should be documented in the patient notes.
 To access an editable pain management plan template, click here
To access an editable pain management plan template, click here
In some cases, a formal written and signed opioid contract may be suitable to ensure safe and effective opioid use, e.g. when strong opioids are prescribed and there are concerns over the potential risk of misuse or dependence. Click here to access an example opioid contract if you think it might be suitable for a specific patient.
- Ideally select an immediate release formulation due to the lower risk of sedation, respiratory depression and overdose (particularly during initiation). Modified-release opioids are a strong risk factor for opioid dependence. N.B. modified-release formulations may still be considered in certain scenarios depending on clinical judgement.
- Use the lowest potency and dose possible to effectively manage pain. Reassess the benefits and risks of treatment when considering each dose increase if pain is insufficiently controlled.
- Prescribe in combination with non-opioid analgesics and/or adjuvant medicines as this may reduce the dose of opioid required to achieve pain relief (due to different modes of action)
- If initiation of a strong opioid is being considered in primary care, ensure morphine is trialled first before prescribing oxycodone (unless the patient has a documented allergy or intolerance)
- Prescribe for the shortest possible duration (ideally three days or less). If this is not practical and longer-term use is required, advise intermittent dosing (i.e. as-needed within the daily dosing limits), rather than continuous use. Intermittent dosing reduces the risks of treatment without compromising potential benefits.
- Prescribe a laxative if use will exceed 2 – 3 days duration and advise patients to remain hydrated
- Be alert for potential signs of misuse and dependence, e.g. requests for early repeats or escalating doses
- If longer-term use is required, check in with the patient at each new prescription to assess the need for continued use. The opioid dose or potency should be gradually titrated down as pain improves (as per treatment plan). For further information, click here
For further information on the role of opioids in manging chronic non-cancer pain from bpacnz, see:
Live Well with Pain is an initiative developed by clinicians in the United Kingdom. It includes a comprehensive suite of freely available resources designed to inform and support health professionals working with patients who have persistent pain and to help guide the appropriate use of opioid medicines. For further information, see: https://livewellwithpain.co.uk/
Given the significant risks related to opioid use in the community, reducing unnecessary use is a key focus in New Zealand, as it is worldwide. Previous work by bpacnz demonstrated that overall, opioid dispensings in New Zealand were relatively stable between 2013 – 2017, with small increases in the use of some options, including codeine, tramadol and morphine, and slight decreases in others, e.g. paracetamol with codeine, oxycodone. Here, we present an update to this investigation of opioid use in New Zealand for the next five-year period (2017 – 2021) to reflect on our progress towards reducing opioid prescribing.
Methodology
- The data reported here is based on two Manatū Hauora, Ministry of Health, National Collections:
- The Pharmaceutical Collection holds claim data submitted by pharmacies for all community dispensings of subsidised medicines.
- The Primary Health Organisation Enrolment Collection holds patient enrolment data for patients registered in New Zealand general practices.
- bpacnz has no control over data errors which may occur at the pharmacy, Sector Services or Ministry of Health. Discrepancies may also exist due to rounding.
- Data has been excluded for patients who are not registered to a practice in the PHO Enrolment Collection. Registered patients accounted for 99% of pharmaceutical dispensings recorded in the National Collections. Data has also been excluded when a National Health Index (NHI) number was not recorded for the patient.
- Injectable opioid formulations were excluded from the analysis as these are most often used in palliative care, i.e. data was limited to oral formulations
- Different morphine salts (e.g. morphine sulphate, morphine hydrochloride) were combined into a single category
The big picture: overall opioid use has declined slightly but there has been a recent increase in dispensings
As expected, weak opioids (e.g. codeine, tramadol) are used significantly more than strong opioids (e.g. morphine, oxycodone) in New Zealand (Figure 1). While there was a net decline in the use of weak opioids between 2017 and 2021, an increase occurred between 2020 and 2021 (Figure 1A). For strong opioids, this upward shift occurred a year earlier in 2019, and was associated with a net increase across the same five-year period (Figure 1B). Despite these opposing net changes in use between weak and strong opioids, overall opioid use marginally declined between 2017 and 2021 as weak opioids account for a significantly greater proportion of total prescriptions.
The increase in opioid dispensings between 2020 and 2021 is notable. Of the various factors that have recently impacted on healthcare and its delivery in New Zealand, none are more obvious or pertinent than the COVID-19 pandemic. The associated nationwide lockdowns and restrictions have had wide-reaching effects on service provision, and recent reports illustrate that high numbers of patients have had surgeries/appointments cancelled or deferred across the regions.9 While it is tempting to speculate that such delays have increased the volume of patients living with chronic pain and therefore are dispensed opioids while they wait, further investigation is required to establish a link.
For updated data on national opioid use in 2022, see: 2022 Data Update: Opioid use remains elevated during the COVID-19 pandemic
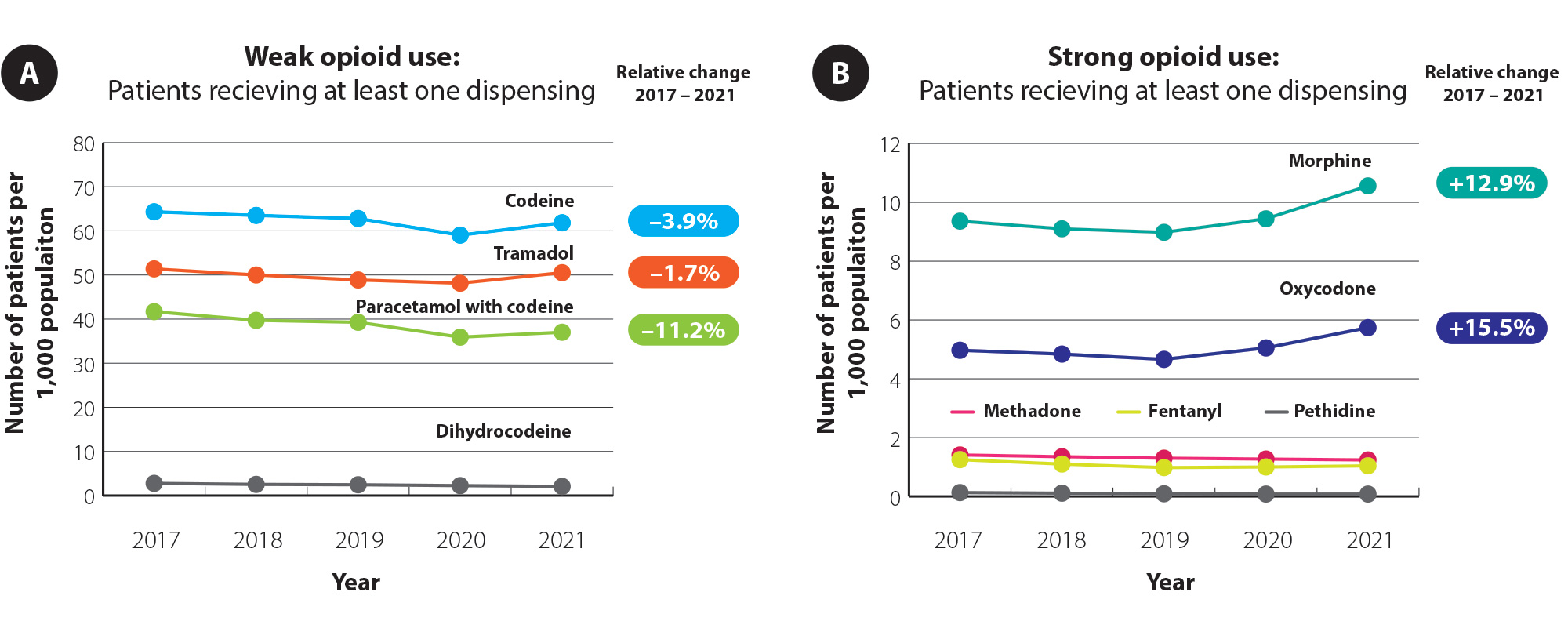
Figure 1. Dispensing of (A) weak and (B) strong opioid analgesics (number of patients with at least one dispensing/1,000 population) in New Zealand between 2017 – 2021. Note the different scales on the y-axis between panels A and B. Data obtained from Manatū Hauora, Ministry of Health, Pharmaceutical collection, 2022.10
Is oxycodone being used appropriately?
Morphine is considered the first-line option if a strong opioid is required. Oxycodone should ideally only be prescribed in patients who cannot tolerate morphine, due to the added risks (particularly misuse).11 In 2016, bpacnz reported that 86% of patients in New Zealand dispensed oxycodone in the community within the previous 12 months did not have a prior prescription for morphine. Most prescriptions were initiated in secondary care, e.g. on hospital discharge.
Using the same methodology, we have determined that:
In 2021, 88% of patients did not have a recorded trial of morphine within the 12 months prior to their first oxycodone prescription.
N.B. Some of these patients may have trialled morphine in hospital and not tolerated it, so no prescription was recorded.
Given that oxycodone dispensing increased by 16% between 2017 and 2021 (Figure 1B), the appropriate use of strong opioids must continue to be a focus moving forward. While the majority of these prescriptions are not initiated in primary care, general practitioners can still question the suitability of renewal requests, and ensure their own prescribing decisions follow best practice standards (see: “How does your prescribing compare?”).
For further information on managing acute pain with strong opioids, see: bpac.org.nz/2018/opioids.aspx
A closer look at national opioid use: key insights
By age group (Figure 2) – total opioid use increases with age. In 2021, peak tramadol use occurred in people aged 55 – 64 years before declining, whereas codeine use continued to increase beyond age 85 years. This difference is possibly because codeine is considered the clinically safer “weak” opioid option and therefore more suitable for older patients. Use of strong opioids (morphine and oxycodone) increased progressively with age, likely due to higher rates of use in cancer care, palliative care, or use in patients with age-related degenerative conditions, e.g. osteoarthritis.
Figure 2. Opioid dispensing by age group in New Zealand in 2021.10
Click between tabs to sort by weak or strong opioids.
Data obtained from Manatū Hauora, Ministry of Health, Pharmaceutical collection, 2022.10
By ethnicity (Figure 3) – people of European/Other ethnicity had significantly higher rates of opioid dispensings compared with other ethnic groups. Between 2017 and 2021, codeine use decreased among people of Asian and Pacific ethnicity while use remained largely static among European/Other and Māori groups. Use of the strong opioids oxycodone and morphine increased among all ethnicities between 2017 and 2021.
Figure 3. Opioid dispensing by age group in New Zealand for 2017 and 2021.10
Click between tabs to sort by weak or strong opioids.
Data obtained from Manatū Hauora, Ministry of Health, Pharmaceutical collection, 2022.10
By region (Figure 4) – there was significant variation in opioid dispensings between New Zealand regions over time.* For example:
- The rate of codeine dispensing for Canterbury in 2021 was the highest in the country; approximately double that in Counties Manukau and, despite being geographically adjacent, 46% higher than in South Canterbury
- Morphine use increased by 31% in Nelson/Marlborough between 2017 and 2021
- The Waikato DHB had the lowest rate of morphine dispensing of all regions in 2021, but had the highest rate of oxycodone use
- The Capital and Coast DHB had the lowest rates of oxycodone use in both 2017 and 2021, potentially due to the persisting impact of their opioid prescribing campaign
The reason behind the observed variation between regions is likely multi-factorial including differences in demographics, hospital and surgical waitlist times and the clinical preferences of local surgical and pain-management teams. These findings highlight the challenge that Te Whatu Ora, Health New Zealand, faces in reducing healthcare inequities between the regions.
* This data was obtained from timepoints pre-dating the disestablishment of New Zealand DHBs and the centralisation of their functions under Te Whatu Ora, Health New Zealand
Figure 4. Opioid dispensing by region (DHB) in New Zealand for 2017 and 2021.10
Click between tabs to sort by opioid.
Data obtained from Manatū Hauora, Ministry of Health, Pharmaceutical collection, 2022.10
The bottom line
Despite a slight decrease in overall opioid dispensings between 2017 – 2021, these medicines are still commonly used in New Zealand. The increase in use near the end of this five-year period is a notable finding that warrants further investigation (particularly in the context of COVID-19 and its effects on healthcare provision), and there is considerable variation in use between age groups, ethnicities and regions. While trends in the use of stronger opioids will be heavily influenced by prescribing initiated in secondary care, these conclusions serve as a reminder that primary care clinicians may benefit from reflecting on their approach to opioid prescribing. Prescribers should always consider whether the indication warrants the potential risk, even if it means questioning secondary care discharge prescriptions. A primary care clinician’s judgement and knowledge of their patient – including their unique clinical history, needs and challenges – is a powerful tool in the fight against opioid misuse.
2022 Data Update: Opioid use remains elevated during the COVID-19 pandemic
The increase in opioid use identified in 2021 was not a transient occurrence; both weak and strong opioid use remained elevated in 2022 compared with “pre-COVID-19” levels (Figure 5).13* Notably, the number of patients dispensed at least one prescription for oxycodone increased by almost 20% between 2020 and 2022 (from 5.0 to 6.0 patients per 1,000 population). In comparison, the increase in the number of patients dispensed morphine was smaller during this period (approximately 10%), despite being the preferred first-line option if a strong opioid is required.
Figure 5. Dispensing of (A) weak and (B) strong opioid analgesics (number of patients with at least one dispensing/1,000 population) in New Zealand between 2017 – 2022. Note the different scales on the y-axis between panels A and B. Data obtained from Manatū Hauora, Ministry of Health, Pharmaceutical collection, 2023.13
When assessing oxycodone use by region in 2020 and 2022, considerable differences can be observed across New Zealand (Figure 6):13
- Waikato consistently had the highest rates of oxycodone use, and in 2022 had a level almost nine times that of Capital and Coast (the lowest in New Zealand)
- The most significant increases during this time period (from 2020 to 2022) were in South Canterbury (+60.8%), Hawkes Bay (+57.0%), Lakes (+41.2%) and Taranaki (+35.3%)
- Rates of oxycodone use were consistently lower on average in the South Island compared with the North Island. Of the five South Island regions, only the Southern region was above the national average in both years.
*The “number of patients with at least one dispensing” was used to assess opioid use rather than “total number of dispensings”. This is because a patient may get multiple prescriptions for small amounts of an opioid or one prescription for up to one month’s supply; therefore, counting the total number of dispensings does not provide meaningful information in this context.
Figure 6. Oxycodone dispensing by region in New Zealand for 2020 and 2022. Data obtained from Manatū Hauora, Ministry of Health, Pharmaceutical collection, 2023.13
Discuss with your peers or self-reflect on factors that could potentially explain the increase in opioid use over the past few years:
- Is the overlap with the “COVID-19 era” causal or coincidental?
- Why might there be such significant variation between regions?
- Are surgical wait times influencing opioid prescribing?
- Do healthcare resource and time limitations make prescribing opioids the more “convenient” option?
- Has the increasing frequency of medicine supply issues compromised or limited prescribing choices?
Evidence suggests that peer prescribing comparisons can reduce opioid prescribing by
primary care clinicians.12 In a 2022 randomised controlled trial clinicians who received
monthly prescribing-comparison emails were 41% less likely to prescribe an opioid for a
patient after their first visit, and 27% less likely to continue prescribing for use beyond three
months compared with a control group.12 For further information, see: “Peer-comparisons can
prompt clinicians to re-consider prescribing decisions”.
With these study findings in mind, consider whether you might benefit from a peer-comparison.
Peer-comparisons can prompt clinicians to re-consider prescribing decisions
A 2022 randomised controlled trial involving 48 primary care practices in the United States has shown that receiving personal versus peer prescribing comparisons leads to a reduction in opioid prescribing by clinicians. Between September 2018 and January 2020, a total of 22,616 opioid-naïve adults were diagnosed with acute non-cancer pain; these patients were specifically identified as having uncomplicated musculoskeletal pain or non-migraine headache (for which opioids are not generally not indicated but are often prescribed).12 If a clinician started a new entry within the electronic system for an opioid prescription in an opioid-naïve patient during an appointment, it would trigger one of four possible alerts/actions depending on the study arm the clinician was randomised to:12
- Active control – clinicians were presented with an electronic alert containing a short checklist of recommendations, including to (1) check their State’s prescription drug monitoring programme, (2) assess for risk factors, (3) avoid extended-release or long-acting formulations, (4) use a low-dose immediate release formulation for a short-period (e.g. 3 – 7 days) and (5) consider non-opioid management options. N.B. An “active” control (rather than a control involving no intervention) was used due to the significance of the “opioid epidemic” in the United States.
- Justification – in addition to the same electronic alert received by the control group (described above), clinicians were required to enter a free-text justification for why they had decided to prescribe the opioid analgesic
- Comparison – in addition to the same electronic alert received by the control group (described above), clinicians received monthly feedback emails comparing their opioid prescribing practices (e.g. total prescriptions, adherence to safe opioid-prescribing guidelines, the proportion of their patients who transition from short- to long-term use) with those of other clinicians
- Justification + Comparison – clinicians were presented with the electronic alert and both the justification requirement and comparison interventions (described above)
Overall, prescribing rates for the study arms were (1) 4.2% in the control group, (2) 3.6% in the justification group, (3) 2.6% in the clinician comparison group and (4) 1.9% in the opioid justification/comparison combination group.12 Further analysis demonstrated that clinicians receiving comparison emails were 41% less likely to prescribe an opioid for a patient after their first visit (P = 0.02), and 27% less likely to continue prescribing for use beyond three months compared with the control group (P = 0.01).12 Notably, given that the control group in this study was “active” (i.e. they still received information that could discourage prescribing), it is likely that the benefit of clinician-targeted peer comparisons would be even greater if no safeguards existed for the controls.
If you are a primary care prescriber and have a My bpac account, log in to see your personalised prescribing snapshot for both 2021 and 2022, including how your prescribing compares to your peers and national trends.
If you don’t have a My bpac account,
sign up for free.
