Published: 22 September 2023
Key practice points:
- Prostatitis can be categorised into four distinct conditions: acute bacterial prostatitis, chronic bacterial prostatitis, chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) and asymptomatic inflammatory prostatitis
- Acute bacterial prostatitis is characterised by the rapid onset of pelvic or genitourinary pain and lower urinary tract symptoms; prompt recognition and antibiotic treatment is essential to avoid complications, e.g. sepsis
- Antibiotic penetration of the prostate tissue limits the choice of effective medicines for both acute (and chronic) bacterial prostatitis
- Consider urgent referral for urology assessment or referral to the emergency department for patients with suspected sepsis or those whose symptoms do not resolve with initial treatment
- Chronic bacterial prostatitis is characterised by persistent infection causing intermittent genitourinary pain and ongoing lower urinary tract symptoms lasting for three months or longer, with evidence of bacterial infection
- Treatment involves longer courses of antibiotics, simple analgesia and alpha-adrenergic antagonists
- CP/CPPS is the most prevalent form of prostatitis, and is diagnosed by excluding other genitourinary conditions
- Symptoms include pelvic, perineal and genitourinary pain, lower urinary tract symptoms and sexual dysfunction; diagnostic criteria require symptoms to be present for at least three of the previous six months, in the absence of infection
- Management is variable depending on the symptoms most affecting the patient’s quality of life
- Antibiotic treatment is not recommended
- Asymptomatic inflammatory prostatitis can be an incidental finding when assessing for suspected prostate cancer or during fertility investigations; it is a diagnosis typically made on biopsy. Treatment is not usually required.
N.B. The term “male” is used in this article to describe the biological sex of the patient population who are at risk of developing prostatitis. However, we acknowledge that this may not reflect the identity of all patients, which will include transgender girls or women, intersex and non-binary individuals.
Prostatitis, referring in general to inflammation of the prostate gland, is a collective term used to describe a spectrum of disorders that can be grouped into four separate clinical categories.1 These were originally defined by the National Institutes of Health (NIH) International Prostatitis Collaborative Network classification system:2
- Acute bacterial prostatitis involves pelvic and genitourinary pain and lower urinary tract symptoms in the presence of a causative pathogen.2 Systemic symptoms, e.g. fever and malaise, are possible in severe cases.2
- Chronic bacterial prostatitis has similar features to acute bacterial prostatitis but symptoms are often less severe and continue (intermittently) for at least three months.3, 4 Urine or semen cultures will often reveal an ongoing or recurrent infection with the same bacterial strain.4
- Chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) is the most common type of prostatitis.2 It is characterised by ongoing pelvic, perineal and genitourinary pain for at least three months in the absence of a causative pathogen.4 Lower urinary tract symptoms, sexual dysfunction and psychological symptoms may also be present.4
- CP/CPPS can be further differentiated into type IIIa (inflammatory) or type IIIb (non-inflammatory) depending on the presence of white blood cells in prostatic secretions or semen,2 however, this investigation is generally only used in a research setting
- Asymptomatic inflammatory prostatitis refers to the incidental finding of inflammation of the prostate in the absence of symptoms, e.g. during fertility investigations or on biopsy for suspected prostate cancer2
A small subset of patients diagnosed with acute bacterial prostatitis may develop chronic bacterial prostatitis,5 however, the exact progression rate is uncertain. Others diagnosed with chronic prostatitis commonly have no history of an acute prostatic infection.
There have been no recent studies on the prevalence of prostatitis in New Zealand
Determining the true prevalence of prostatitis in primary care is challenging, due to changing definitions and variable or non-specific symptoms that overlap with other urological conditions.6 There are no recent epidemiological data on the rates or ethnic distribution of prostatitis in New Zealand; overseas figures are often outdated or involve population groups that are too specific for extrapolation to primary care in this country. Analysis of more than 10,000 males from North America and Asia estimates a prevalence of prostatitis-related symptoms of 8%.7
Bacterial prostatitis has varied aetiology
Bacterial infection of the prostate can be caused by various factors involving infection or obstruction of the urinary tract (Table 1).8 Gram-negative species are often implicated in acute bacterial prostatitis; causative pathogens include Escherichia coli (55 – 75% of cases), followed by other members of the Enterobacteriaceae family (e.g. Klebsiella, Proteus, Enterobacter, Citrobacter and Serratia species) and Enterococcus species (2 – 10%).8
Occasionally, bacteria responsible for sexually transmitted infections (STI), such as those that cause urethritis and epididymitis, e.g. Neisseria gonorrhoeae and Chlamydia trachomatis, can spread to the prostate.8 Consider sexually transmitted pathogens as a cause of bacterial prostatitis in sexually active males; particularly those who engage in high risk sexual activity, e.g. anal intercourse.8, 9
In patients with an indwelling catheter or who have undergone a recent urological procedure and are experiencing symptoms, Pseudomonas aeruginosa can be responsible for acute bacterial prostatitis.8
Immunocompromised people, e.g. with HIV, are at higher risk of developing lower urinary tract infections (UTI) and prostatitis.1, 5 In addition to common causative pathogens, other possible causes in these patients include Candida species and Mycobacterium tuberculosis.10
Table 1. Risk factors for the development of bacterial prostatitis.1 ,8, 9
| Risk factor |
Examples |
| Bacterial infection of the genitourinary tract |
UTI, urethritis, epididymitis and/or orchitis, STI |
| Functional or anatomical anomalies that can predispose people to genitourinary infections and therefore prostatitis |
Phimosis, urethral strictures or narrowing of the urethra due to benign prostatic hyperplasia |
| Genitourinary procedures |
Indwelling or intermittent catheterisation, transrectal prostate biopsy |
| High-risk sexual activity |
Unprotected anal intercourse |
| Co-morbidities |
Diabetes or immunocompromise, e.g. HIV infection |
BPH = benign prostatic hyperplasia; HIV = human immunodeficiency virus; STI = sexually transmitted infection; UTI = urinary tract infection
Pelvic or genitourinary pain (e.g. perineal pain, rectal pain, pain during or after ejaculation), and lower urinary tract symptoms such as urgency, dysuria, hesitancy, incomplete bladder emptying, are features of acute bacterial prostatitis.9 Systemic symptoms include nausea and vomiting with fever.11 Rigors may be present in more severe cases.11 Early identification and treatment of these patients is paramount as progression to significant complications is possible,1 e.g. sepsis, prostatic abscess, urinary retention (secondary to prostatic oedema/swelling).11
Examination and investigations in patients with suspected acute bacterial prostatitis
Physical examination should include:
- An assessment of temperature, heart rate, blood pressure and other observations, depending on the patient’s clinical condition
- An abdominal examination to assess for the site of the pain, urinary retention (if available, ultrasound scanning can aid assessment of retention) and to help exclude other causes for the symptoms, e.g. gastrointestinal conditions9, 12
- An examination of the external genitalia for features such as discharge, swelling, tenderness13
- A digital rectal exam (DRE) may provide further evidence for the diagnosis; gentle palpation is recommended to avoid inducing bacteraemia.9 A tender, enlarged and “boggy” prostate gland is common in a patient with acute bacterial prostatitis,1 whereas its absence may help differentiate patients with urethritis or epididymitis and/or orchitis.13
Relevant investigations include:
- Mid-stream urine (MSU) for culture and susceptibility testing to support the diagnosis and guide antibiotic selection (see: “Management of chronic bacterial prostatitis in primary care“)9
- Haematuria may also indicate a bladder stone or tumour
- Additional laboratory investigations will depend on the clinical presentation and patient risk factors,9 e.g. consider a first void urine sample if a STI pathogen is suspected
Practice point: Investigating prostate specific antigen (PSA) is not recommended during acute infection as levels may be temporarily elevated.9 It may take up to two months for PSA to return to normal following treatment.9 If delaying the investigation is not appropriate, interpret results with caution, and repeat after symptoms have resolved.6 Continue to monitor patients with abnormal PSA results until the level normalises, or refer if it does not (for further information on PSA monitoring and referral thresholds, see: www.health.govt.nz/system/files/documents/publications/prostate-cancer-management-referral-guidance_sept15-c.pdf).
A wide differential diagnosis is required for patients with lower urinary tract symptoms
There is significant crossover between symptoms and signs caused by acute bacterial prostatitis and other genitourinary conditions.9 In patients presenting with new onset genitourinary pain, lower urinary tract symptoms and symptoms and signs of systemic illness, also consider:9, 13
- UTI
- STI
- Acute pyelonephritis
- Epididymitis and/or orchitis
- Benign prostatic hyperplasia (BPH)
- Urinary obstruction, e.g. cancer or calculi
- Proctitis
- Prostate cancer
 Red flag prostatitis symptoms
Red flag prostatitis symptoms
Red flags indicating that emergency department or acute urology referral is warranted are similar across the spectrum of prostatitis,
and include patients with:4, 11
- Severe systemic symptoms and signs indicative of sepsis
- Acute urinary retention
N.B. Patients with suspected acute bacterial prostatitis whose symptoms are worsening or have not improved 48 hours after initiation of antibiotics should also be considered for emergency department referral.11 Patients with a palpable abnormality on DRE who are not severely unwell should be reassessed following treatment and referred to urology, if required. Clinical judgement is needed to distinguish “expected” abnormalities (e.g. a tender, soft or boggy prostate often present in acute prostatitis which should resolve) from more concerning features (e.g. hard irregular lump, potentially indicating prostate cancer), taking into account symptom history and PSA results.
Antbiotic treatment is indicated in acute bacterial prostatitis
Empiric antibiotic treatment is recommended for all patients with suspected acute bacterial prostatitis (Table 2).9, 11 Trimethoprim achieves therapeutic concentrations in prostate tissue,8 and can be used alone or in combination with sulfamethoxazole as first-line treatment.11, 14 Antibiotics should be prescribed for at least two weeks.11
The patient should be reviewed within 48 hours and then 14 days after initiating treatment.11 Initial antibiotic treatment may require modification depending on results of urine culture and sensitivities,11 e.g. consider switching the patient to ciprofloxacin* if MSU results indicate the causative pathogen is not sensitive to the prescribed antibiotic. Antibiotic treatment can be withdrawn after 14 days if symptoms have resolved, otherwise consider an additional two weeks of treatment depending on the patient’s symptoms, signs and any additional test results, if applicable.11
*Ciprofloxacin is recommended as the first-line choice for acute bacterial prostatitis in some guidelines (e.g. National Institute for Health Care Excellence, NICE) as it is effective against a wider range of urinary pathogens than trimethoprim,11 however, due to rates of resistance to ciprofloxacin in New Zealand,15 it is reserved as a second-line choice for infections known to be susceptible. NICE lists trimethoprim as an equal first-line option for patients unable to take ciprofloxacin.11
Table 2. Oral antibiotic options for the management of patients with mild to moderate acute bacterial prostatitis in primary care.11, 14
| Antibiotic choice |
Dose |
| First-line: |
|
| Trimethoprim; OR |
300 mg, once daily, for two to four weeks |
| Trimethoprim + sulfamethoxazole |
960 mg, twice daily, for two to four weeks |
| Second-line: |
|
| Ciprofloxacin (only if known to be susceptible) |
500 mg, twice daily, for four weeks |
N.B. Some regional guidelines differ in antibiotic recommendations for acute bacterial prostatitis (e.g. cefalexin as a first-line option). This may be due to local resistance or sensitivity patterns and choices should not be routinely used in other regions. Check for local advice (e.g. HealthPathways) and follow corresponding empiric treatment recommendations, if available.
Symptomatic treatment should be tailored to the individual patient; paracetamol or NSAIDs should be prescribed for genitourinary pain management.11 Patients with obstructive lower urinary tract symptoms, e.g. hesitancy or incomplete emptying of the bladder, may benefit from an alpha-adrenergic antagonist, e.g. doxazosin.16 Consider discussion with a urologist or emergency department referral for patients with suspected acute bacterial prostatitis whose symptoms are worsening or have not improved 48 hours after initiation of antibiotics.11 Patients with acute bacterial prostatitis and significant co-morbidities, e.g. diabetes or immunocompromise, should be monitored closely to confirm symptoms are improving, and have a lower threshold for referral to the emergency department.
Antibiotic treatment for prostatitis caused by STI pathogens
If first void urine results indicate that either N. gonorrhoeae or C. trachomatis are the causative pathogen, prescribe appropriate antibiotic treatment for these STIs.1 Discussion with an infectious diseases or sexual health physician is recommended as the duration of treatment may need to be extended to allow sufficient medicine concentrations in prostatic tissue.
N.B. Contract tracing of sexual contacts is also required.1
For guidelines on appropriate antibiotics for STI management in primary care, see: bpac.org.nz/antibiotics/guide.aspx
Recurrent symptoms are possible
Patients who experience a recurrence of symptoms following initial treatment may require an extended course of antibiotics,9 i.e. more than four weeks. Urine culture should be repeated to confirm presence of the same organism and susceptibility testing used to guide any changes to antibiotic choice.9 If symptoms repeatedly recur or persist for three months, the patient meets criteria for chronic bacterial prostatitis.9
A small number of patients may develop a prostatic abscess
Prostatic abscess is a rare complication of acute bacterial prostatitis.17 Patients can present with similar symptoms to acute bacterial prostatitis and a fluctuant abscess may be palpable on DRE.17 Possible risk factors include diabetes, immune suppression, urinary instrumentation, e.g. indwelling catheter or prostate biopsy, and chronic kidney or liver disease.17, 18 A prostatic abscess should be considered in patients who do not respond to (or worsen following) initial antibiotic treatment;17 referral to the emergency department is appropriate.11
Chronic bacterial prostatitis is a persistent or recurrent infection of the prostate resulting in episodes of genitourinary pain and lower urinary tract symptoms over three months or longer.4 Infection may be the result of a UTI migrating from the urethra to the prostate, or haematogenous or lymphogenous spread from elsewhere in the body, e.g. rectum.1 In some cases, undertreated or recurrent acute bacterial prostatitis can progress to a chronic infection.1, 5 The causative bacterial species are consistent with those found in acute bacterial prostatitis, e.g. E. coli, and repeated urine or semen culture results usually show that the same organism(s) is present throughout the course of the condition (see: “Bacterial prostatitis has varied aetiology”).1, 5
Diagnosing chronic bacterial prostatitis can be challenging.1 The presence and severity of symptoms varies, although they are often milder than seen in acute bacterial prostatitis,3, 4 and people can be asymptomatic between episodes.12 Some level of genitourinary pain is expected.1 Systemic symptoms are rare but possible, e.g. fever.5 New-onset sexual dysfunction or psychological symptoms, e.g. anxiety or depression, can develop;4 potentially as a result of persistent and invasive symptoms having a negative impact on a person’s quality of life.
Recommended examination and investigations are the same as for evaluating a patient with acute bacterial prostatitis, however, the physical examination and DRE are frequently normal (see: “Examination and investigations in patients with suspected acute bacterial prostatitis”).1
Management of chronic bacterial prostatitis requires extended antibiotic treatment
Antibiotic options recommended for chronic bacterial prostatitis are the same as those used for acute infection (Table 2), although the optimal duration of treatment is uncertain. The European Association of Urology (EAU) recommends treatment for four to six weeks.10 A longer duration (e.g. up to 12 weeks) may be necessary in some patients if symptoms do not completely resolve.5
Symptom specific treatments should be prescribed in combination with antibiotics, as indicated.16 This may include paracetamol or NSAIDs for genitourinary pain and an alpha-adrenergic antagonist, e.g. doxazosin, for obstructive lower urinary tract symptoms.16 Effective symptom management and reassurance that their condition can be managed may help to reduce or alleviate symptoms of anxiety and depression.
A relapse or recurrence of symptoms can occur
Some patients with chronic bacterial prostatitis will experience a relapse or recurrence of symptoms.5 This can occur for various reasons, e.g. functional/anatomical prostate abnormalities, antibiotic resistance, non-adherence to the treatment regimen or medicine interactions.5 Some patients may develop prostatic calculi that can become reservoirs for bacteria, making eradication difficult.5
In patients who experience symptom recurrence, repeat the urine culture before prescribing another course of antibiotics.5 If the previous antibiotic was effective, consider prescribing a longer duration of treatment, e.g. six weeks instead of four weeks, or change the antibiotic according to susceptibility testing.5 Patients who remain symptomatic following two courses of antibiotics should be discussed with a urologist.4
Recognising and treating bacterial prostatitis may be more familiar for many clinicians, however, CP/CPPS is actually more prevalent.2 Part of the difficulty with recognising this condition relates to variable symptom patterns, often with unclear aetiology (i.e. absence of confirmed infection) and limited effective treatments.
The pathophysiology of CP/CPPS is not fully understood and likely multifactorial.12 One proposed mechanism is central sensitisation; disruption of central pain pathways by ongoing inflammation or infection of the prostate, resulting in an altered perception of pain.4 Similar theories have been postulated as an explanation for other chronic pain conditions such as fibromyalgia and endometriosis.4 It is also likely that psychological stress plays a significant role in CP/CPPS.1 Pelvic floor dysfunction, e.g. muscle spasm or tenderness, may explain symptoms in some people.6
CP/CPPS subcategories have limited use
CP/CPPS is further categorised in the literature, however, these subcategories have not been clinically validated,19 and investigations to determine the category are not recommended in primary care and are unlikely to influence treatment. CP/CPPS can be type IIIa (inflammatory) or type IIIb (non-inflammatory) depending on the presence or absence of leukocytes in a post-prostatic massage urine sample, prostate secretions or semen.2 In some cases, patients may also switch between CP/CPPS type IIIa and type IIIb.6 The required investigations, e.g. four-glass Meares–Stamey test, are not recommended outside of a specialist urology setting.6
Evaluation of CP/CPPS
The diagnosis of CP/CPPS is based on recognising a pattern of symptoms that are not explained by any other diagnoses. This is likely to take place over multiple consultations.
The symptoms of CP/CPPS fall into four main categories:
- Pelvic or genitourinary pain. Pain is a feature in most patients with CP/CPPS and can include one or multiple locations, e.g. the perineum, penis or testes (especially penile tip), groin, rectum, lower back or abdomen.6 Pain on or after urination or ejaculation may also occur.6 People may describe feeling like they are “sitting on a hot poker” or have pain deep inside their anus or behind the scrotum. Suprapubic pain is also described.
- Lower urinary tract symptoms. These are similar to those experienced by people with other forms of prostatitis, e.g. hesitancy, urgency, dysuria, haematospermia1, 6
- Psychological symptoms. People with CP/CPPS may experience co-morbid depression and anxiety.6 Difficulties associated with managing their symptoms can also lead to maladaptive coping mechanisms and catastrophising, further reducing the patient’s quality of life.20
- Sexual dysfunction. Erectile dysfunction, premature or delayed ejaculation and decreased libido are associated with a diagnosis of CP/CPPS, however, the causes are not well understood and likely multifaceted.6, 21
Initial discussions with the patient should include:3
- The nature, duration, frequency and severity of symptoms; the presence of individual symptoms and severity may fluctuate6
- Their sexual history
- Their medical history, e.g. asking about co-morbidities such as diabetes or immunocompromise, previous pelvic injury, recent diagnosis of a UTI or STI, known BPH, recent urological procedures
Making the diagnosis: Consider CP/CPPS in a patient if pelvic or genitourinary pain has been present for at least three of the past six months and urine culture results are negative (ruling out chronic bacterial prostatitis).4 Prostate cancer and BPH should also be excluded. Differential diagnosis for CP/CPPS can be found in Table 3.
Table 3. Differential diagnosis of chronic prostatitis/chronic pelvic pain syndrome.4, 22
| Gastrointestinal |
Irritable bowel syndrome, inflammatory bowel disease, colorectal cancer |
| Genitourinary |
Chronic bacterial prostatitis, UTI, STI, bladder pain syndrome, BPH, bladder or prostate cancer, renal calculi, overactive bladder, prostatic abscess |
| Musculoskeletal |
Pelvic floor dysfunction, pelvic injury or trauma |
| Neurologic |
Neurogenic bladder, pudendal neuralgia |
BPH = benign prostatic hyperplasia; STI = sexually transmitted infection; UTI = urinary tract infection
Symptoms guide management
Once a diagnosis has been made, discuss realistic treatment outcomes with the patient.20 CP/CPPS is a chronic condition that cannot be cured but the symptoms can be successfully managed.20 A pragmatic approach is required, and treatment should be individually tailored to a patient’s predominant symptoms (Figure 1), with the overall goal of improving their quality of life.20
Combination treatment with appropriate first-line options is recommended, such as alpha-adrenergic antagonists for lower urinary tract symptoms and NSAIDs for pain (Figure 1), as there is evidence that this is more effective than monotherapy.6 Initial pharmacological interventions should be trialled for four to six weeks;6 beneficial medicines usually need to be continued long term.
Physiotherapy for pelvic floor dysfunction
Targeted physiotherapy, e.g. strengthening of pelvic floor muscles, can be beneficial in patients whose symptoms are suspected to be the result of pelvic muscle dysfunction.6 Some regions may offer publicly funded pelvic physiotherapy, otherwise patients would need to self-fund. Acupuncture and transdermal electrical nerve stimulation (TENS) have been trialled for chronic pain conditions, however, there is a lack of evidence to support their use in practice.6
For local physiotherapists, see: physio.org.nz/#find-a-physio
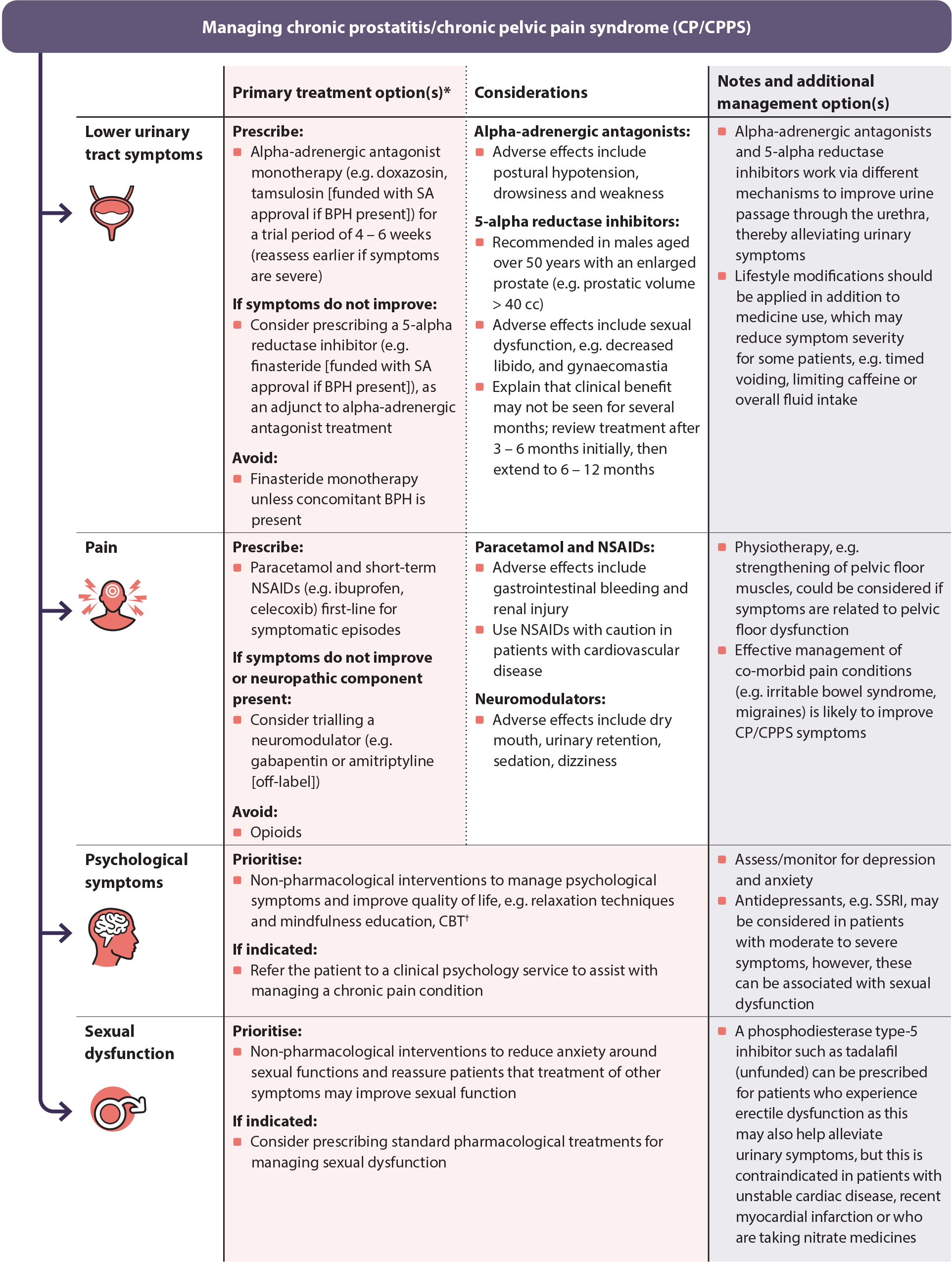
Figure 1. Symptom-based management of chronic prostatitis/chronic pelvic pain syndrome.6, 14, 20 ,24, 25
* For further information on specific dosing of medicines for CP/CPPS, see: https://nzf.org.nz/nzf_4259
† Free online (non-specific) CBT courses are available from: https://www.justathought.co.nz/ and https://beatingtheblues.co.nz/
BPH = benign prostatic hyperplasia; CBT = cognitive behavioural therapy; SA = Special Authority; SSRI = selective serotonin reuptake inhibitor
Prescribing antibiotics for CP/CPPS is controversial
For a diagnosis of CP/CPPS, a bacterial cause for the patient’s symptoms must be ruled out but despite this, some expert groups recommend the use of antibiotics in these patients.4, 6, 20 A 2020 analysis of six international studies found low-quality evidence that compared to placebo, quinolone antibiotics may reduce prostatitis symptoms with no increase in rates of adverse effects,26 however, there is insufficient evidence to support their use in primary care.
Regular patient follow up is usually required
Follow-up should occur four to six weeks after initial presentation to evaluate the patient’s response to treatment.6 Regular follow-up also provides an opportunity to assess mental health and wellbeing, and how the patient is coping with the psychological impacts of their symptoms. Patients should be informed that the expected treatment response time is usually slow; it may take four to six weeks before there is any obvious symptom improvement.
International guidelines recommend early referral to urology for patients who do not report symptom improvement following initial treatment.6 In practice, it may appropriate to trial second-line interventions while awaiting non-acute urology assessment, e.g. a 5-alpha reductase inhibitor for refractory lower urinary tract symptoms. Evidence suggests there may be benefit in patients aged over 50 years with an enlarged prostate.6, 20 Amitriptyline can be considered if pain is likely neuropathic or was not adequately controlled with paracetamol or NSAIDs.6, 20 Early referral is recommended for patients with pelvic pain or lower urinary tract symptoms that are causing a significant impact on their quality of life.6
The final classification of prostatitis is asymptomatic inflammatory prostatitis. This is characterised by elevated white blood cells in prostate specific samples, e.g. leukocytospermia, and may be detected during fertility investigations or on biopsy for suspected prostate cancer.1 Exploratory research has associated asymptomatic inflammation of the prostate with increased serum PSA levels and prostatic calcification in patients with obstructive BPH,27, 28 however, the clinical significance of this inflammation is still uncertain.1 Patients diagnosed with asymptomatic inflammatory prostatitis do not usually require treatment.1 In practice, some patients undergoing treatment for infertility may be prescribed a course of oral antibiotics, however, there is no clinical evidence to support this.





