Published: 14 September 2021
Twenty-twenty was challenging for everyone, particularly for the health professionals at the front line of New Zealand’s
response to the COVID-19 pandemic. While New Zealand has experienced low COVID-19 case and mortality rates and few ongoing
restrictions compared to many other countries, the effects of the pandemic continue to be felt,
e.g. the August, 2021 Delta variant outbreak and return to Level 4 restrictions. The key events in New Zealand’s
COVID-19 pandemic 2020 timeline are outlined in Figure 1. The four-week national Level 4 “lockdown” and the following three
weeks of further restrictions from 25 March until 13 May saw most people staying at home, with many adapting to working
and learning remotely. Another cluster of cases in August moved Auckland up to Alert Level 3 (effectively another lockdown)
for two weeks.
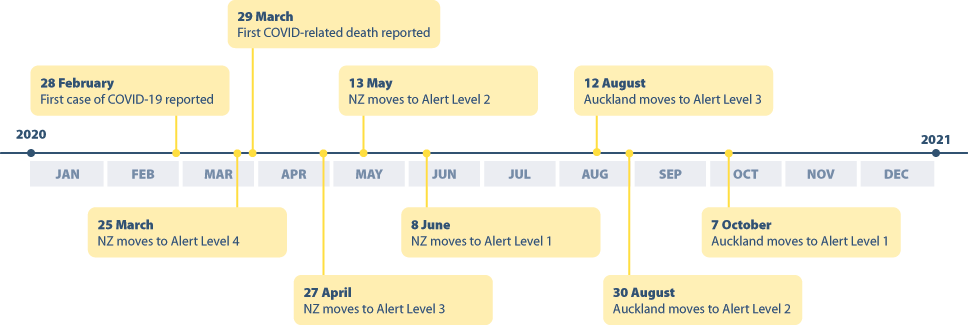
Figure 1: Overview of key events in the COVID-19 pandemic in New Zealand in 2020.1
Primary care rapidly adapted to the COVID-19 pandemic, particularly with respect to the use of technology to enable patients
to access care remotely. Examining the dispensing data provides an opportunity to reflect on 2020 and whether there were
any notable trends as a result of the changes to and challenges of general practice during this time. This report raises
and addresses the following questions about dispensing in the community in 2020:
- Were there changes in the number of dispensed prescriptions overall and was there any evidence of worsening inequities
in dispensing by ethnicity?
- Were there changes in antibiotic dispensing given the lower rates of respiratory illness due to various measures, including
lockdowns, social distancing, wearing face masks, hygiene measures and high rates of influenza vaccination?
- Were there changes in the dispensing of antidepressants, anti-anxiety or insomnia medicines given the potential for
stress associated with the pandemic to trigger or worsen depression, anxiety or sleep issues?
- Were there changes in the dispensing of medicines used for the management of long-term conditions commonly encountered
in primary care, i.e. did people remain adherent despite the restrictions of the lockdowns?
Overall, approximately 236,000 more prescriptions were dispensed in 2020 than 2019 (an increase of 0.5%). However, after
adjusting for population, the number of dispensed prescriptions (per 1,000 registered patients) was 1% lower in 2020
than 2019 (Figure 2). The number of dispensed prescriptions has remained relatively stable over time, increasing
by 2% between 2018 and 2019, no change between 2017 and 2018, and decreasing by 1% between 2016 and 2017. The decrease in
dispensing in 2020 suggests there may have been some patients who did not receive medicines they would have otherwise received,
e.g. due to not obtaining a repeat prescription, not presenting to primary care (virtually or in person) for diagnosis and
management, or reduced need for certain medicines (see: “Antibiotic dispensing”).
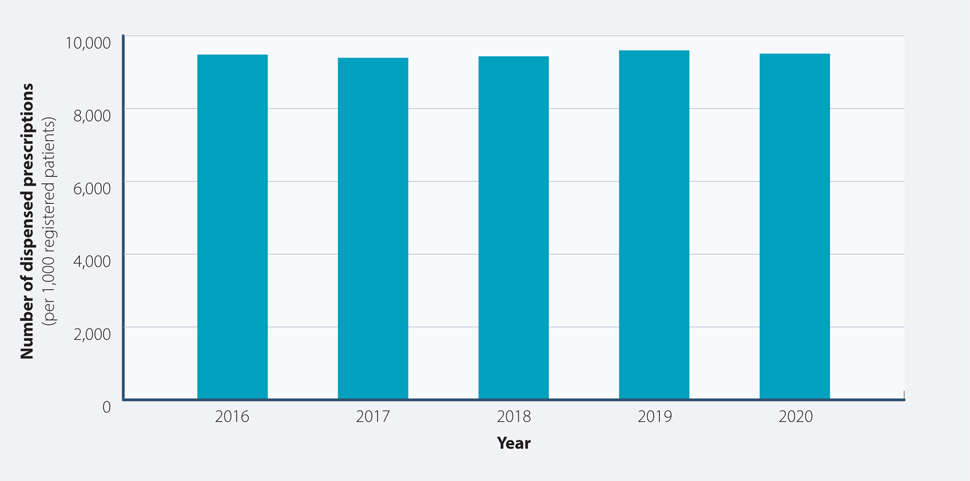
Figure 2: Total number of dispensed prescriptions (per 1,000 registered patients) from community pharmacies
in New Zealand, 2016 – 2020.
Figure 3 shows the number of dispensed prescriptions (per 1,000 registered patients) by month between 2016 and 2020. Dispensing
in March, 2020 was markedly higher than the same month in the previous four years. There were 1,008,418 more prescriptions
(200 per 1,000 registered patients) dispensed from community pharmacies in March, 2020 compared to March, 2019, reflecting
the trend of people "stocking up" on prescriptions prior to the national lockdown. This was followed by a comparable
decrease in dispensing in April, 2020 – there were 750,890 fewer dispensed prescriptions (168 per 1,000 registered patients)
than in April, 2019. Following the March peak and April trough in 2020, the dispensing rate increased steadily and by August
was comparable to 2019. There was another peak in dispensing in November, 2020, which was higher than previous years.
Anecdotally, there have been reports that some patients stopped taking their regular preventative medicines during the national lockdown and did not
resume them until later in the year, which may explain this observation.
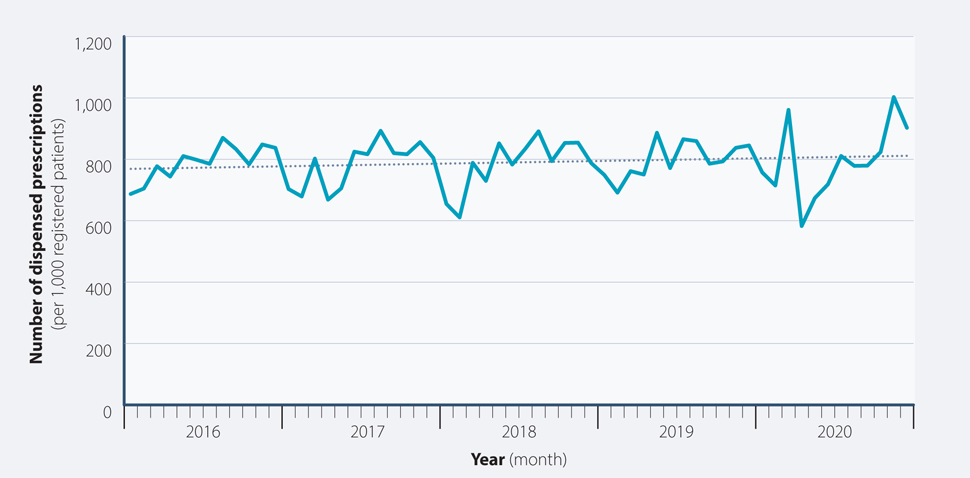
Figure 3: Number of dispensed prescriptions (per 1,000 registered patients) from community pharmacies in New Zealand by month, 2016 – 2020.
The dotted line represents the linear trend in dispensing over time.
Total community dispensings in New Zealand by ethnicity, 2016 - 2020
The COVID-19 pandemic has disproportionately burdened communities who were already experiencing inequities in healthcare.
In New Zealand, ethnic minorities have poorer health outcomes compared to those of European descent, which includes access
to medicines. The peak in dispensing prior to the national lockdown (Figure 3) shows that many people rapidly accessed healthcare,
but this required further examination to see if this effect was seen in all ethnic groups or if differences in the ability
to access healthcare in this way (e.g. due to cost, transport, time away from work or childcare, internet access for virtual
appointments) affected access to medicines.
Figure 4 shows the number of dispensed prescriptions (per 1,000 registered patients) by ethnicity between 2016 and 2020.
During this time period, the dispensing rate was relatively stable for all ethnic groups; the largest change was for Pacific
peoples between 2018 and 2019 (3% increase). Between 2019 and 2020, however, the dispensing rate decreased for all
ethnic groups except European/Others (Table 1). This was in contrast to an increase of 2 – 3% for all ethnic groups
between 2018 and 2019.
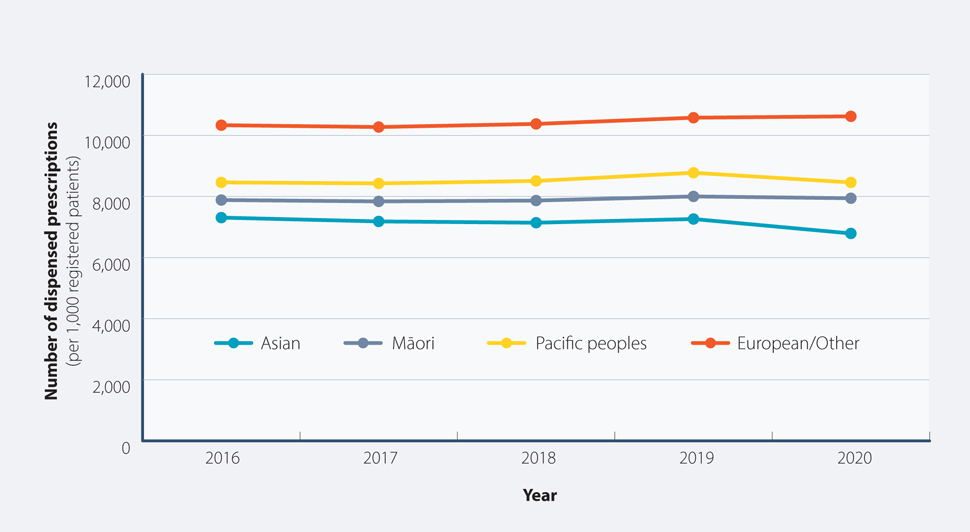
Figure 4: Total number of dispensed prescriptions (per 1,000 registered patients) from community pharmacies in New Zealand
by ethnicity, 2016 – 2020.
Table 1: Percentage change in the number of dispensed prescriptions (per 1,000 registered patients) from
community pharmacies in New Zealand by ethnicity between 2018 – 2019 and 2019 – 2020.
| Ethnic group |
Change 2018/2019 |
Change 2019/2020 |
| Asian |
 2% increase 2% increase |
 6% decrease 6% decrease |
| European/Other |
 2% increase 2% increase |
0% |
| Māori |
 2% increase 2% increase |
 1% decrease 1% decrease |
| Pacific peoples |
 3% increase 3% increase |
 4% decrease 4% decrease |
Figure 5 shows the dispensing rate by ethnicity by month in 2020. There was a similar peak and trough
in March and April, respectively, in 2020 for each ethnic group, corresponding to the national lockdown. Dispensing
after the national lockdown did not recover to the same extent in Māori, Pacific and Asian peoples as for European/Others,
which is reflected in the overall lower dispensing rate in 2020 than 2019 for these ethnic groups (Figure
4). Together these data suggest that the effects of the COVID-19 pandemic in 2020 may have increased disparities and
adherence issues with people not resuming preventative medicines, but may also reflect reduced need for some medicines at
this time, e.g. antibiotics (see: “Antibiotic dispensing”).
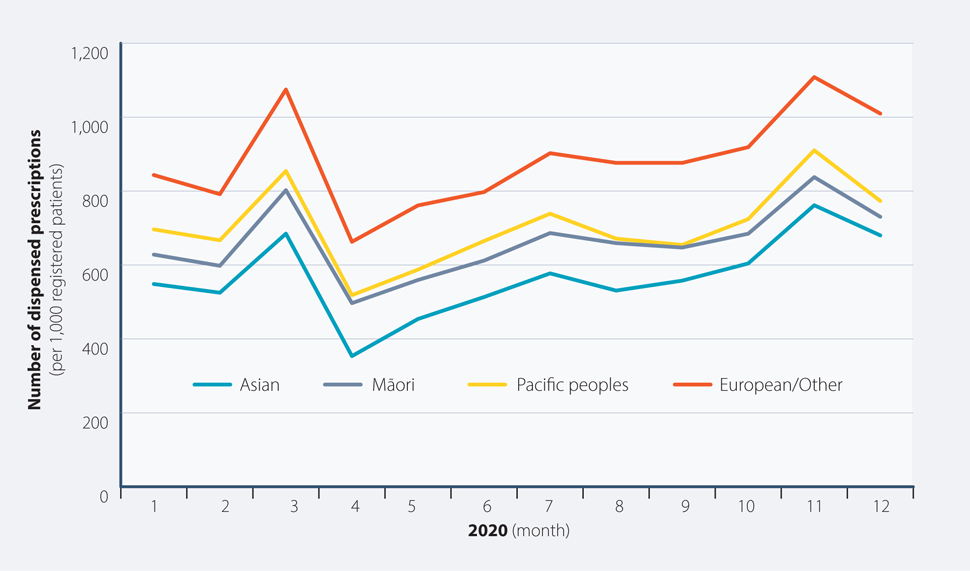
Figure 5: Number of dispensed prescriptions (per 1,000 registered patients) from community pharmacies in New Zealand
by ethnicity, by month in 2020.
Overall, antibiotic dispensing has been trending downward over time due to improved antimicrobial stewardship. Dispensing
of oral antibiotics dropped dramatically in 2020, with 20% fewer prescriptions dispensed (per 1,000 registered patients)
in 2020 than 2019, compared to a 3% decrease in the number of dispensed prescriptions between 2019 and 2018. The
2020 pandemic response saw the adoption of various practices to mitigate transmission of COVID-19, including lockdowns,
social distancing, wearing face masks, hygiene measures and high rates of influenza vaccination. This resulted in not only
low numbers of COVID-19 cases, but also a reduction in other infectious illnesses, e.g. upper respiratory tract infections
and influenza. Improved public awareness of viral infections and acceptance of the limited role of antibiotics in treatment
also likely contributed to the marked reduction in antibiotic dispensing in 2020.
Antibiotic dispensing rates typically increase over the winter months, reflecting more people presenting to primary care
with respiratory tract infections and receiving a prescription for antibiotics. Figure 6 shows that there
was a marked decrease in dispensing in the second quarter of 2020 (April – June) and the absence of a peak in the third
quarter (July – September) compared to the same periods in 2019. Antibiotic dispensing rates are usually highest
in Pacific peoples and Māori, followed by Europeans/Other and lowest in Asian peoples (Figure 7). There
was a marked decrease in antibiotic dispensing in all ethnic groups in 2020, with the largest decreases in Asian and Pacific
peoples (Table 2).
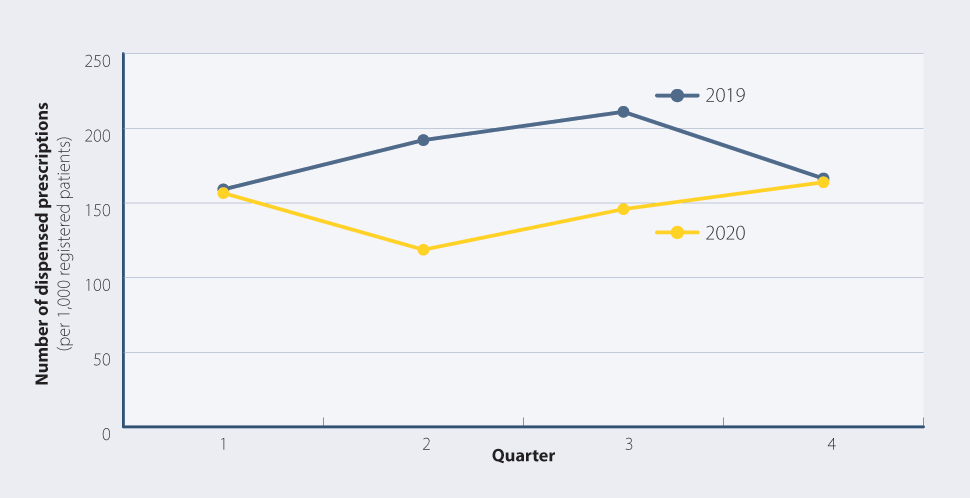
Figure 6: Number of dispensed prescriptions (per 1,000 registered patients) for oral antibiotics from
community pharmacies in New Zealand by quarter, 2019 and 2020.
Table 2: Percentage change in the number of dispensed prescriptions (per 1,000 registered patients) from
community pharmacies in New Zealand by ethnicity between 2018 – 2019 and 2019 – 2020.
| Ethnic group |
Change 2018/2019 |
Change 2019/2020 |
| Asian |
 2% decrease 2% decrease |
 30% decrease 30% decrease |
| European/Other |
 3% decrease 3% decrease |
 18% decrease 18% decrease |
| Māori |
 5% decrease 5% decrease |
 17% decrease 17% decrease |
| Pacific peoples |
 3% decrease 3% decrease |
 23% decrease 23% decrease |
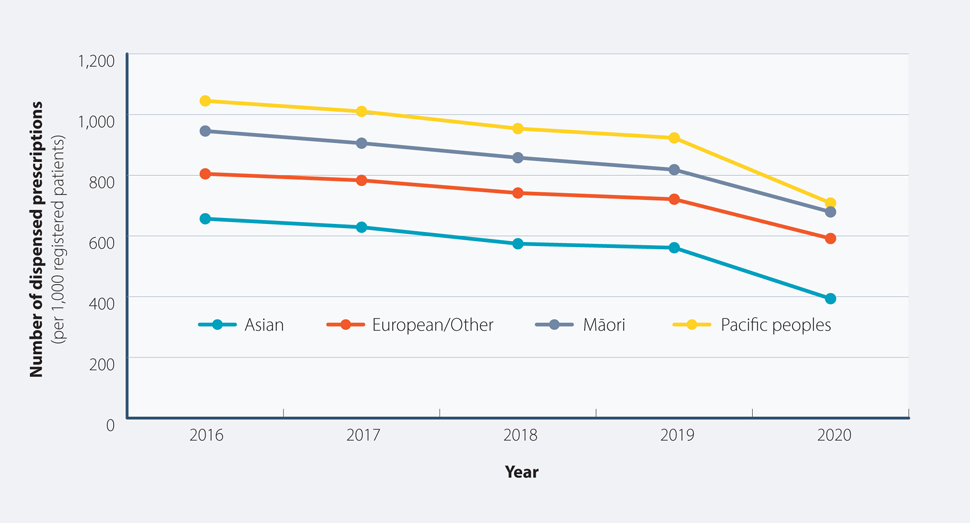
Figure 7: Number of dispensed prescriptions (per 1,000 registered patients) for oral antibiotics from
community pharmacies in New Zealand by ethnicity, 2016 – 2020.
The COVID-19 pandemic was, and continues to be, stressful for many people for a variety of reasons, including health concerns,
job loss or insecurity, isolation from family/whānau and friends, and balancing working-from-home with childcare, schooling
and family relationships. These factors would be expected to increase presentations to primary care of people with symptoms
of distress, depression, anxiety and sleep problems, and potentially result in more prescriptions for antidepressants, anxiolytics
and hypnotics in 2020 compared to previous years. The data show that, in general, this was not the case, although there
may have been more antidepressants dispensed.
Antidepressants
Figure 8 shows that the number of dispensed prescriptions for selective serotonin re-uptake inhibitors
(SSRIs) has been steadily increasing over time; dispensing of tricyclics and other antidepressants has remained relatively
stable between 2016 and 2020. There was a 7% increase in SSRI dispensing between 2019 and 2020, compared
to 4% between 2018 and 2019 and 1% increases between both 2016 and 2017 and 2017 and 2018. While the expected rate of change
over time is not known, the 7% increase in dispensing rate in 2020 appears larger than the usual rate of increase.
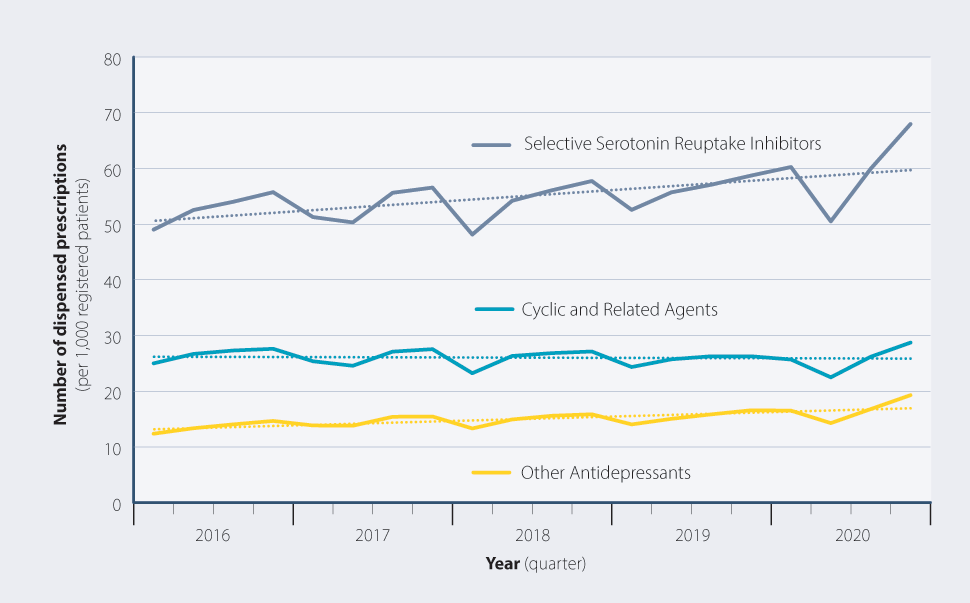
Figure 8: Number of dispensed prescriptions (per 1,000 registered patients) for antidepressants from community
pharmacies in New Zealand by quarter, 2016 – 2020. Dotted lines represent the linear trend in dispensing over time.
Profile of patients newly initiated or re-initiated on an antidepressant, 2018 – 2020
In 2020, a total of 543,842 patients (114 per 1,000 registered patients) were dispensed an antidepressant. Of these, 28%
were newly initiated or re-initiated, i.e. were not dispensed an antidepressant in the previous year (Table
3). Unexpectedly, the COVID-19 pandemic did not seem to have a marked effect on the number of patients initiated on
an antidepressant, as the proportion of new patients was comparable to previous years (Table 3).
In those initiated on antidepressants in 2020, the dispensing rate (number of patients per 1,000 registered patients)
was highest in those aged 20 – 39 years and over age 80 years, which was consistent with 2018 and 2019.
Table 3: Characteristics of patients (per 1,000 registered patients) initiated on antidepressants, 2018 – 2020.
|
|
2018 |
2019 |
2020 |
| Number of patients dispensed an antidepressant |
Total |
504,494 |
521,695 |
543,842 |
| Per 1,000 |
110 |
111 |
114 |
| Number of patients newly initiated or re-initiated* |
Total |
141,791 |
149,057 |
153,198 |
| Per 1,000 |
31 |
32 |
32 |
| Age* |
< 20 years |
9 |
9 |
10 |
| 20 – 39 years |
42 |
44 |
45 |
| 40 – 59 years |
38 |
38 |
39 |
| 60 – 79 years |
34 |
33 |
34 |
| ≥ 80 years |
42 |
43 |
41 |
| Ethnicity* |
Asian |
18 |
18 |
19 |
| European/Other |
36 |
37 |
37 |
| Māori |
28 |
29 |
29 |
| Pacific peoples |
15 |
16 |
17 |
* No antidepressant dispensed in the previous year
Zopiclone, benzodiazepines and quetiapine
The number of dispensed prescriptions for zopiclone, indicated for the treatment of insomnia, has remained relatively
stable over the past five years and there was no marked change in this trend in 2020 (Figure 9). Conversely, the number
of dispensed prescriptions for benzodiazepines, which are indicated for the management of anxiety and insomnia, has been
trending upward since 2017 (Figure 9). There was a 2% increase in the number of dispensed prescriptions for benzodiazepines
between 2019 and 2020, compared to previous increases of 1% between 2018/2019 and 2017/2018 and a 2% decrease between
2016 and 2017, i.e. much the same.
Quetiapine is an atypical antipsychotic indicated for the treatment of psychosis and bipolar disorder; it is also used
off-label for the treatment of insomnia, anxiety, post-traumatic stress disorder and the behavioural and psychological symptoms
of dementia (BPSD). Figure 9 shows an upward trend in quetiapine dispensing since 2016. Between 2019 and 2020, the
number of dispensed prescriptions for quetiapine increased by 10%, continuing the pattern of increase seen in previous
years. Dispensing increased by 7% between 2018 and 2019, 5% between 2017 and 2018 and 3% between 2016 and 2017. This trend
may be explained by increased clinician familiarity with this medicine and its use off-label in younger people for treating
insomnia and anxiety.
For further information on managing BPSD, see: bpac.org.nz/2020/bpsd.aspx
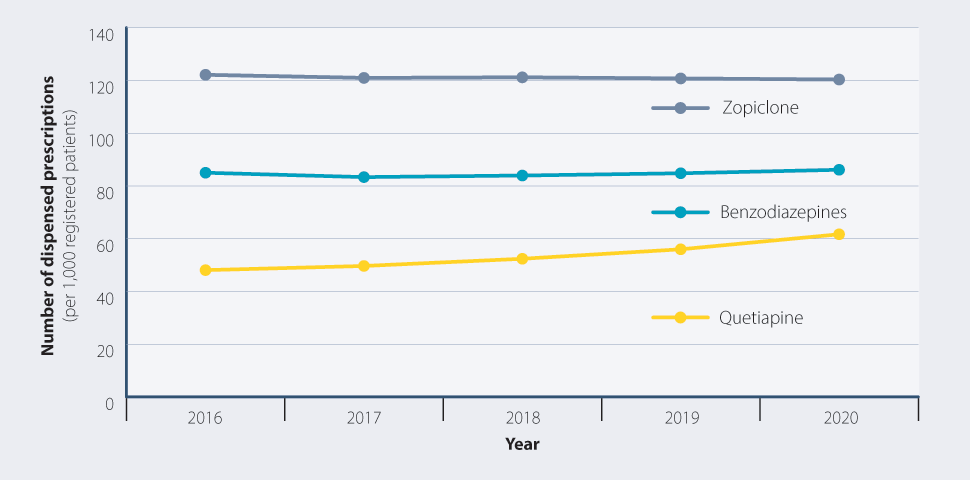
Figure 9: Number of dispensed prescriptions (per 1,000 registered patients) for zopiclone, benzodiazepines and
quetiapine from community pharmacies in New Zealand, 2016 – 2020.
Profile of patients newly initiated or re-initiated on zopiclone, a benzodiazepine or quetiapine, 2018 – 2020
Surprisingly, the number of patients newly initiated or re-initiated* on zopiclone and benzodiazepines was
lower in 2020 than previous years (Figure 10). The majority of patients initiated on zopiclone or a benzodiazepine were of
European/Other ethnicity and the dispensing rate generally increased with age (Figure 11).
*No dispensed prescriptions for these medicines in the previous year
The number of patients newly initiated or re-initiated on quetiapine has been increasing since 2018, although the overall
numbers remain small (Figure 10). The dispensing rate was highest in those aged 20 – 39 years and over 80 years in 2020,
which was unchanged from 2018 and 2019 (Figure 11). Increasing dispensing rates in the older age groups likely reflect its
off-label use for managing BPSD, rather than an effect of the COVID-19 pandemic. In younger people, the reason for the increase
is less certain, but may relate to increasing off-label use for insomnia or anxiety.2 The highest dispensing
rates for quetiapine were in Māori and European/Others (Figure 11), which was unchanged from previous years and consistent
with other reports of antipsychotic prescribing in New Zealand.2
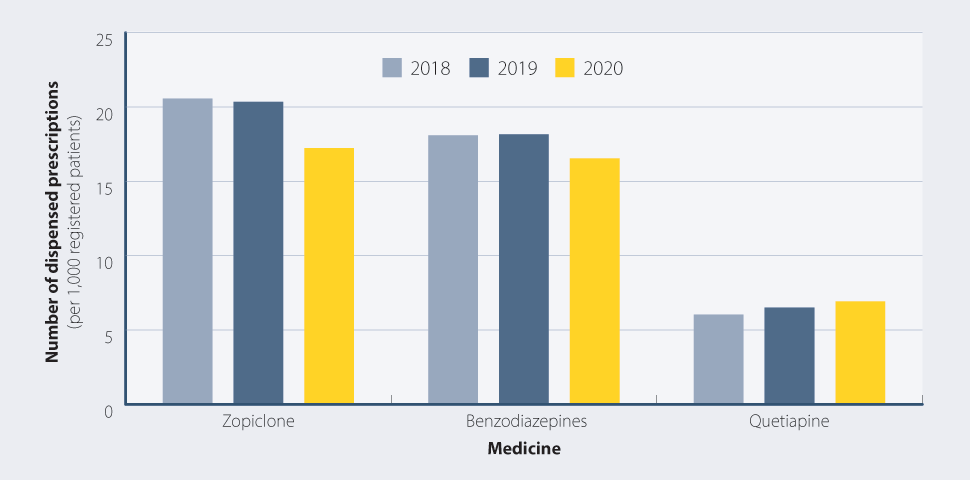
Figure 10: Number of patients (per 1,000 registered patients) newly initiated or re-initiated on zopiclone,
benzodiazepines or quetiapine, 2018 – 2020.
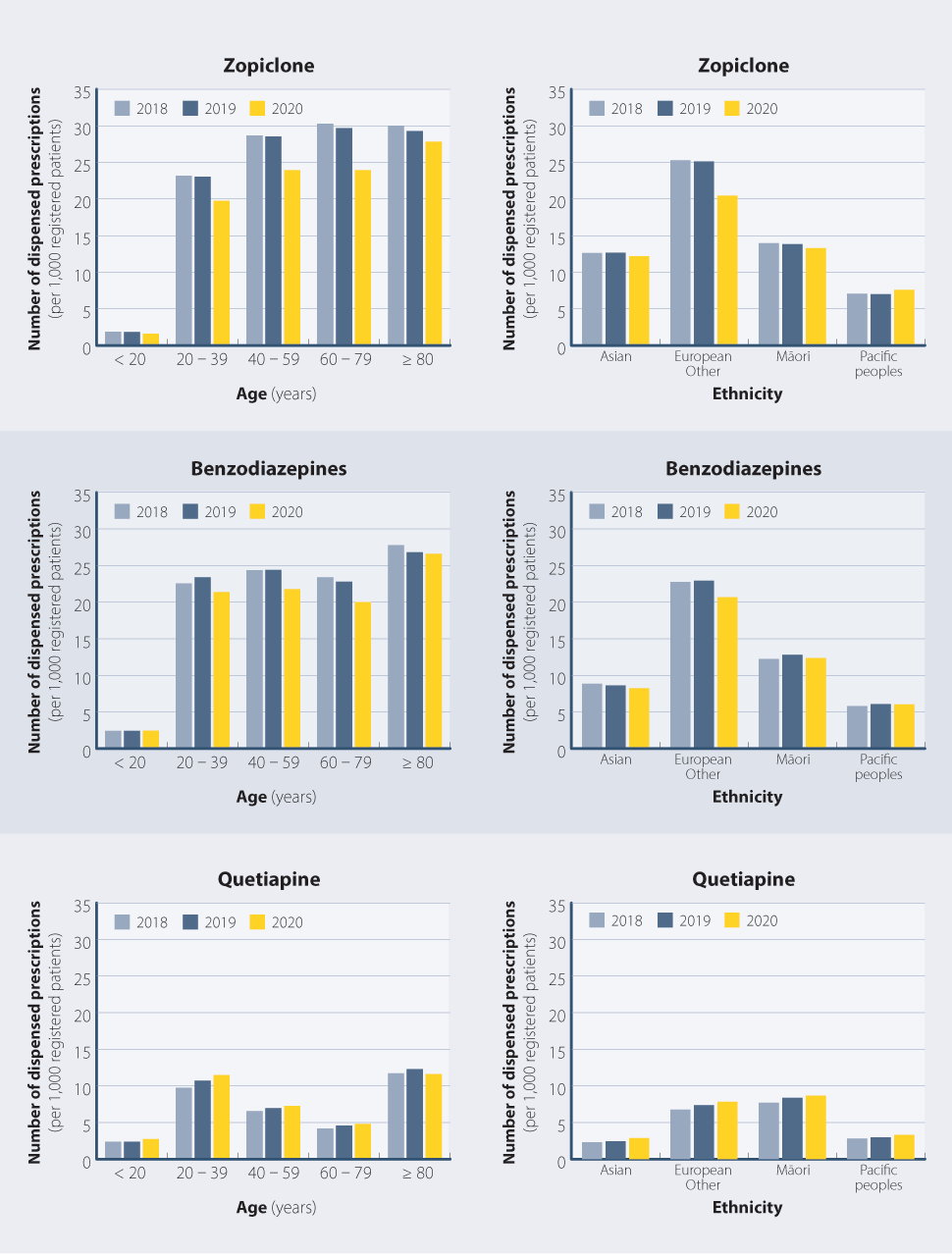
Figure 11: Number of patients (per 1,000 registered patients) newly initiated or re-initiated on zopiclone, benzodiazepines or
quetiapine by age and ethnicity, 2018 – 2020.
The number of dispensed prescriptions for medicines used for the management of long-term conditions such as cardiovascular
disease, gout and type 2 diabetes is expected to increase over time due to population growth, ageing and increasing rates
of co-morbidities. During the COVID-19 pandemic, it was predicted that the lockdown restrictions might result in people
delaying primary care appointments or not accessing primary care remotely to request a prescription and therefore not receiving
regular prescriptions for their long-term medicines. Encouragingly, this did not seem to be the case.
Type 2 diabetes is a significant health issue in New Zealand, particularly for Māori and Pacific peoples. The number of
people diagnosed with type 2 diabetes increases by approximately 3 - 4% each year*. Consequently, dispensing
of oral glucose-lowering medicines has also been increasing over time (Figure 12 and Table
4). The number of dispensed prescriptions for oral glucose-lowering medicines (per 1,000 registered patients)
increased by 8% between 2019 and 2020, continuing the upward trend from the previous year (7% increase between
2018 and 2019).
*Based on data from the Virtual Diabetes Register. N.B. The Virtual Diabetes Register does not
distinguish between type 1 and type 2 diabetes. Therefore, the estimation of the proportion of type 2 diabetes is based
on the assumed ratio of 90% type 2 diabetes to 10% type 1 diabetes.3
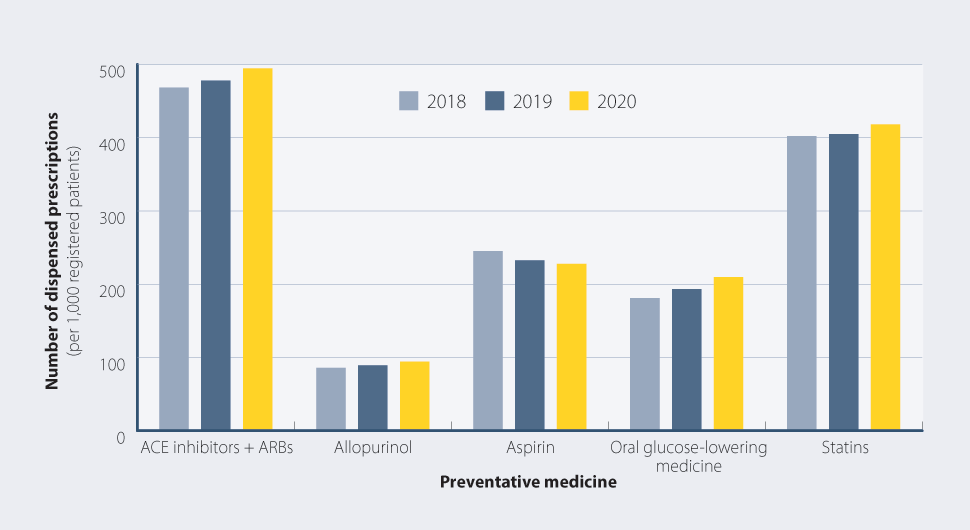
Figure 12: Number of dispensed prescriptions (per 1,000 registered patients) from community pharmacies in
New Zealand for selected medicines used in the management of long-term conditions, 2018 – 2020.
The number of dispensed prescriptions for ACE inhibitors and ARBs, allopurinol and statins was also higher in
2020 than in 2019, continuing an upward trend in dispensing from 2018 (Table 4).
The number of dispensed prescriptions for aspirin decreased by 2% between 2019 and 2020, continuing a downward trend;
dispensing decreased by 5% between 2018 and 2019 (Table 4). The reasons for this decrease may relate
to changing evidence about its role in primary prevention of cardiovascular disease, availability of other antiplatelet
medicines or people with atrial fibrillation being prescribed an anticoagulant rather than aspirin.
Table 4: Percentage change in the number of dispensed prescriptions (per 1,000 registered patients) from
community pharmacies in New Zealand for selected medicines used in the management of long-term conditions, 2018 – 2019
and 2019 – 2020.
| Medicine |
Change 2018/2019 |
Change 2019/2020 |
| ACE inhibitors + ARBs |
 2% increase 2% increase |
 4% increase 4% increase |
| Allopurinol |
 4% increase 4% increase |
 6% increase 6% increase |
| Aspirin |
 5% decrease 5% decrease |
 2% decrease 2% decrease |
| Oral glucose-lowering medicines |
 7% increase 7% increase |
 8% increase 8% increase |
| Statins |
 1% increase 1% increase |
 3% increase 3% increase |
Taken together, these data show that the COVID-19 pandemic and associated restrictions did not appear to have a marked
negative ”pandemic” effect on the dispensing of preventative medicines. A number of factors are likely to underpin this,
including many people receiving prescriptions prior to the national lockdown, widespread uptake of telehealth and other
technologies to enable patients to access primary care virtually and the pro-active efforts of primary care to contact patients
and ensure they had supplies of their regular medicines.
