Published: July, 2023 | Review date: July, 2026
This audit is a tool for primary care health professionals
to increase medicines safety in their practice. The aim is to
ensure that patients who are prescribed anti-hypertensive
medicines are not put at increased risk of acute kidney injury.
Angiotensin converting enzyme (ACE) inhibitors, angiotensinII receptor blockers (ARBs), diuretics and non-steroidal
anti-inflammatory drugs (NSAIDs) all have the potential to
decrease renal function. When any of these medicines are
prescribed together the patient’s risk of acute kidney injury
(AKI) is increased. ACE inhibitors/ARBs and diuretics are
often taken concurrently, either as individual medicines or
combination formulations. In patients taking ACE inhibitors/
ARBs and diuretics particular care is required to avoid NSAIDS
(the “triple whammy”) due to the increased risk of AKI. The
addition of a NSAID to the patient’s treatment may also reduce
the blood pressure-lowering effect of the ACE inhibitor and
reduce the volume depleting effect of the diuretic.
When treatment with an ACE inhibitor/ARB and a diuretic is
initiated, it is helpful to highlight the need to avoid NSAIDs in
the patient’s notes to alert other clinicians who may consider
prescribing a NSAID in the future. Patients taking an ACE
inhibitor/ARB and a diuretic should be warned of the risks of
using NSAIDs and should be advised to avoid using over-the
counter (OTC) NSAIDs, including combination products that
contain NSAIDs, e.g. paracetamol and ibuprofen.
If a NSAID must be prescribed to a patient already taking
an ACE inhibitor/ARB and diuretic, the lowest effective dose
should be used for the shortest possible duration. Patients
should also be advised to:
- Maintain adequate fluid intake at all times
- Avoid additional NSAIDs
- Manage periods of acute illness carefully, e.g. by
maintaining good fluid intake, stopping the NSAID and
seeking medical attention if their condition deteriorates
Before the triple whammy is initiated, a baseline
measurement of serum creatinine is essential as it may be
required later to diagnose AKI. A follow-up assessment,
with repeat measurements of body weight, blood pressure,
serum creatinine and electrolytes, within the first month of
treatment may also be beneficial, due to the increased risk of
AKI during this period.
Further information is available from: “Avoiding the
“triple whammy” in primary care: ACE inhibitor/ARB + diuretic
+ NSAID”, bpac.org.nz/2018/triple-whammy.aspx
Summary
This audit identifies patients who are taking ACE inhibitors/ARBs and diuretics. Patient management is then assessed to
determine if appropriate steps have been taken to maximise
safety, including patient advice, avoidance of NSAIDs and
testing of renal function in patients who do require NSAIDs.
Recommended audit standards
Ideally, all patients who are taking an ACE inhibitor/ARB with a
diuretic will have documented evidence in their patient record
of a discussion about the need to avoid NSAIDs. Patients who
are prescribed a NSAID at any time while also prescribed an
ACE inhibitor/ARB and a diuretic, should also have a baseline
renal function test recorded prior to the NSAID prescription,
e.g. in the last three months, and have documented evidence
that strategies to avoid the adverse effects of treatment have
been discussed.
Eligible patients
All patients who are currently taking an ACE inhibitor/ARB and a diuretic are eligible for this audit.
Identifying patients
You will need to have a system in place that allows you to
identify eligible patients. Many practices will be able to
identify patients by running a "query" through their PMS.
Once a patient taking an ACE inhibitor/ARB and a diuretic
is identified, the patient’s notes should then be reviewed to
check if they have been concurrently prescribed a NSAID at
any time.
Sample size
A sample size of 30 patients who are currently taking an ACE inhibitor/ARB and a diuretic is sufficient for the purposes of this audit.
Criteria for a positive outcome
A positive result is if a patient who is currently taking an ACE
inhibitor/ARB and a diuretic has documented evidence in
their patient record of a discussion about the need to avoid
NSAID use. Ideally, the notes would also be flagged to alert
other clinicians in the practice to avoid prescribing NSAIDs.
If the patient has also been concurrently prescribed a NSAID at any time they should have:
- The results of a renal function test recorded in the three
months prior to the NSAID prescription
- Documented evidence that strategies to avoid adverse
effects have been discussed, e.g. maintaining fluid
intake, avoiding other NSAIDs and managing acute
illness
Data analysis
For each patient who is currently taking an ACE inhibitor/ARB
and a diuretic, record whether or not there is documented
evidence in their record that the need to avoid NSAIDs has
been discussed. If the patient has also been prescribed a NSAID
at any time, note if a renal function test has been performed in
the three months prior to the NSAID prescription and if there
is documented evidence of a discussion about strategies to
avoid adverse effects.
Patients who do not meet the criteria for a positive result, i.e.
they have “No” recorded in any column the data sheet, should
be flagged for review.
Clinical audits can be an important tool to identify where gaps exist between expected and actual performance. Once completed, they can provide ideas on how to change practice and improve patient outcomes. General practitioners are encouraged to discuss the suitability and relevance of their proposed audit with their practice or peer group prior to commencement to ensure the relevance of the audit. Outcomes of the audit should also be discussed with the practice or peer group; this may be recorded as a learning activity reflection if suitable.
The Plan, Do, Study, Act (PDSA) model is recommended by the Royal New Zealand College of General Practitioners (RNZCGP) as a framework for assessing whether a clinical audit is relevant to your practice. This model has been widely used in healthcare settings since 2000. It consists of two parts, the framework and the PDSA cycle itself, as shown in Figure 1.
1. The framework
This consists of three questions that help define the “what” and “how” of an improvement project (in this case an audit).
The questions are:
- "What are we trying to accomplish?" – the aim
- "How will we know that a change is an improvement?" – what measures of success will be used?
- "What changes can we make that will result in improvement?" – the concept to be tested
2. The PDSA cycle
This is often referred to as the “engine” for creating, testing and carrying out the proposed changes. More than one cycle is usually required; each one is intended to be short, rapid and frequent, with the results used to inform and refine the next. This allows an ongoing process of continuous learning and improvement.
Each PDSA cycle includes four stages:
- Plan – decide what the change to be tested is and how this will be done
- Do – carry out the plan and collect the data
- Study – analyse the data, assess the impact of the change and reflect on what was learned
- Act – plan the next cycle or implement the changes from your plan
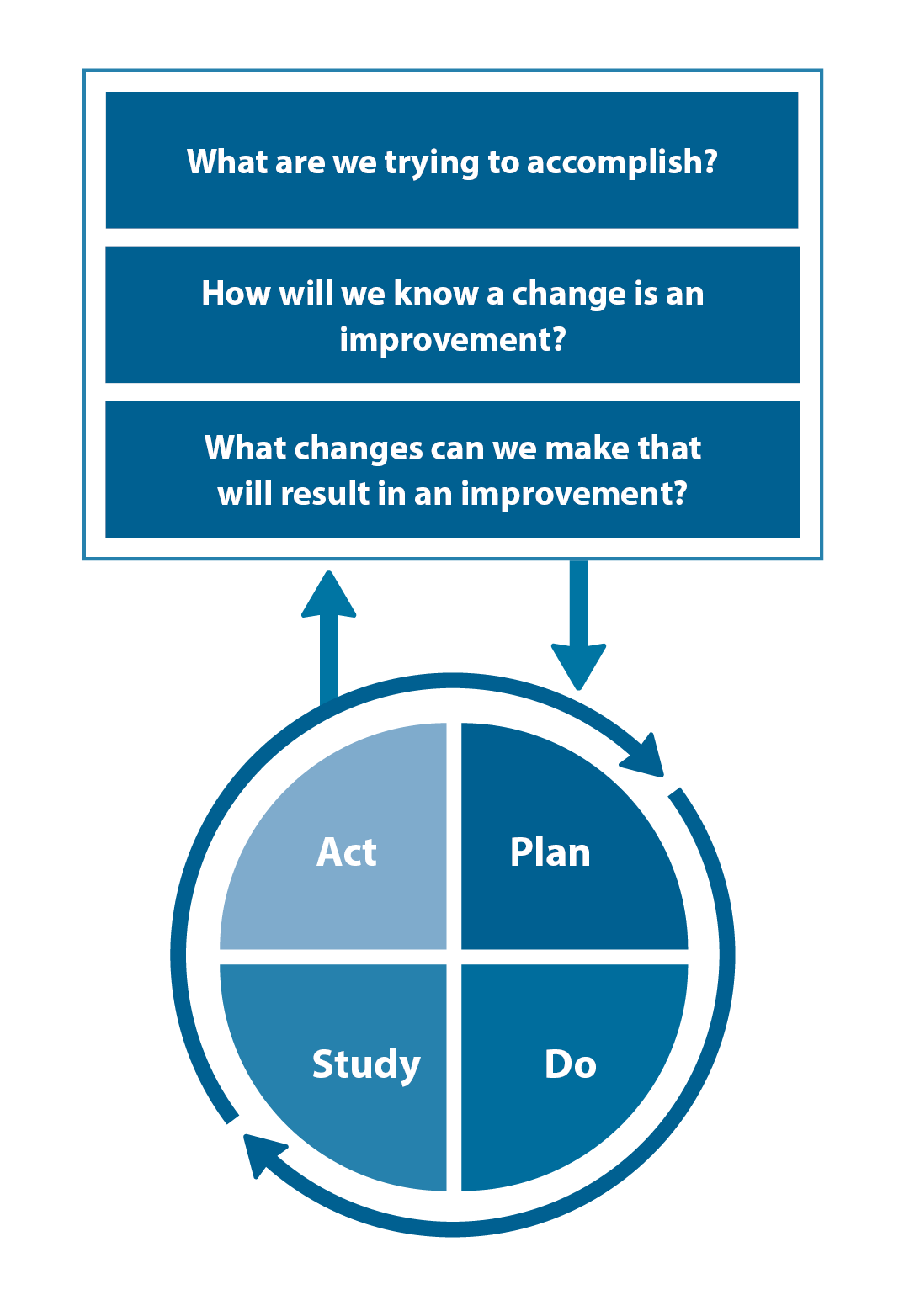
Figure 1. The PDSA model for improvement.
Source: Plan, Do, Study, Act (PDSA) cycles and the model for improvement

Claiming credits for Te Whanake CPD programme requirements
Practice or clinical audits are useful tools for improving clinical practice and credits can be claimed towards the Patient Outcomes (Improving Patient Care and Health Outcomes) learning category of the Te Whanake CPD programme, on a two credit per learning hour basis. A minimum of 12 credits is required in the Patient Outcomes category over a triennium (three years).
Any data driven activity that assesses the outcomes and quality of general practice work can be used to gain credits in the Patient Outcomes learning category. Under the refreshed Te Whanake CPD programme, audits are not compulsory and the RNZCGP also no longer requires that clinical audits are approved prior to use. The college recommends the PDSA format for developing and checking the relevance of a clinical audit.
To claim points go to the RNZCGP website: www.rnzcgp.org.nz
If a clinical audit is completed as part of Te Whanake requirements, the RNZCGP continues to encourage that evidence of participation in the audit be attached to your recorded activity. Evidence can include:
- A summary of the data collected
- An Audit of Medical Practice (CQI) Activity summary sheet (Appendix 1 in this audit or available on the
RNZCGP website).
N.B. Audits can also be completed by other health professionals working in primary care (particularly prescribers), if relevant. Check with your accrediting authority as to documentation requirements.





