Published: 17th October, 2025
Key practice points
- Most people with COVID-19 now experience a mild illness and can safely manage their symptoms and recovery at home. However, some people remain at high risk of progressing to severe disease and may require COVID-19 antiviral treatment to reduce the likelihood of adverse outcomes.
- There are two COVID-19 antivirals available in New Zealand; nirmatrelvir with ritonavir (Paxlovid; oral) and remdesivir (Veklury; IV). Their use is only recommended for people who are at high risk of severe outcomes (i.e. hospitalisation and death) from COVID-19. Nirmatrelvir/ritonavir is the only COVID-19 antiviral prescribed to patients in the community.
- Risk factors for severe outcomes could be due to medical (e.g. co-morbidities), personal (e.g. vaccination status, ethnicity) or social circumstances (e.g. unreliable setting in which to recover from COVID-19)
- Nirmatrelvir/ritonavir is a combination protease inhibitor that blocks SARS-CoV-2 viral replication. Ritonavir slows the metabolism of nirmatrelvir (by inhibiting CYP3A4) so that it reaches therapeutic concentrations.
- The usual dose is 300 mg nirmatrelvir (two pink tablets) and 100 mg ritonavir (one white tablet), twice daily, for five days. Lower doses are prescribed for patients with an eGFR < 60 mL/min/1.73 m2.
- Nirmatrelvir/ritonavir was previously contraindicated in patients with an eGFR < 30 mL/min/1.73 m2, but now can be considered in this group
- Nirmatrelvir/ritonavir should be initiated as soon as possible once the patient has COVID-19; it must be started within five days of symptom onset. Clinical review to assess the suitability of the combination medicine prior to prescribing should include:
- Establishing whether the patient meets access criteria for funded treatment
- Reviewing most recent eGFR (if available)
- Checking for potential medicine interactions
- The prescription for nirmatrelvir/ritonavir must be endorsed by the prescriber to confirm that the patient meets access criteria. The following information should also be included: date of symptom onset, eGFR result if known renal impairment and the prescriber’s contact number.
- Nirmatrelvir/ritonavir is generally well tolerated. Adverse effects may include taste disturbances, gastrointestinal upset (e.g. nausea, diarrhoea) and less commonly, hypertension and myalgia.
- Viral rebound can occur in some patients following COVID-19 antiviral treatment. If this occurs, symptoms are usually mild and can be self-managed; further COVID-19 antiviral treatment is not indicated.
- Nirmatrelvir/ritonavir is approved for use in people aged ≥ 18 years; management of COVID-19 in children and adolescents in the community should focus on vaccination, supportive care and referral to paediatric services when required
SARS-CoV-2, the virus that causes COVID-19, continues to circulate in the community.1 Most people with COVID-19 have mild disease that can be managed at home with supportive care. However, some people experience more severe disease and are at high risk of complications, including hospitalisation and death (see: “Factors that increase risk of severe outcomes from COVID-19”).
COVID-19 was declared a Public Health Emergency of International Concern (PHEIC) by the World Health Organization in January, 2020, and in March, 2020, the COVID-19 global pandemic officially began; the PHEIC ended in May, 2023.2 Reported COVID-19 case numbers in New Zealand peaked in 2022, and have since generally declined, with occasional spikes; wastewater detections have followed a similar trend.1, 3 New variants and subvariants of SARS-CoV-2 have emerged over time, with varied transmissibility and severity.4, 5 The predominant variant in New Zealand as of October, 2025, is NB.1.8.1, which belongs to the Omicron lineage.4 The Omicron variant has a lower risk of severe outcomes compared to earlier variants such as Delta.6 Hospitalisations and mortality due to COVID-19 have also reduced over time,1 likely due to a combination of factors, including reduced SARS-CoV-2 virulence, immunity (acquired through infection and/or vaccination) and COVID-19 antiviral treatments.
COVID-19 vaccination and antivirals influence hospitalisation and mortality rates
COVID-19 vaccination, introduced in 2021, has been associated with significantly improved clinical outcomes, including hospitalisation and mortality from COVID-19 in New Zealand over time.7, 8 COVID-19 vaccines have been modified and updated since they were first established to better address the new variants and subvariants in circulation. The Comirnaty JN.1 vaccine is currently available in New Zealand. This vaccine has been adapted to target the JN.1 variant of SARS-CoV-2, which as of October, 2025, is in circulation in New Zealand, but at lower levels than NB.1.8.1.4 While this COVID-19 vaccine does not have specific coverage against NB.1.8.1, it is still likely to offer much protection, as the variant shares similarities with JN.1.9
Most people in New Zealand (who are eligible) are vaccinated against COVID-19; additional doses (previously termed “booster” doses) are available every six months for eligible people. Of those aged ≥ 12 years, 83.1% had completed the primary vaccination course (originally two doses, now a single dose); 71.2% of people aged ≥ 18 years had received their first additional dose, and 57.3% of people aged ≥ 50 years had received their second additional dose (data up to 12th October, 2025).1 People who have not been vaccinated against COVID-19 are likely to now have some natural immunity from infection, given the time that has passed since SARS-CoV-2 first began circulating.10 However, there will be a very small group who will have no COVID-19 immunity, i.e. not vaccinated against COVID-19 and have not been exposed to SARS-CoV-2.
COVID-19 antivirals have been funded for groups at high risk of severe outcomes from COVID-19 since 2022 in New Zealand.7 Currently, there are two antivirals available; nirmatrelvir with ritonavir (Paxlovid; oral) and remdesivir (Veklury; intravenous [IV]; hospital use). Nirmatrelvir/ritonavir is the only COVID-19 antiviral prescribed for patients in the community, and it has been shown to reduce the risk of hospitalisation and death in patients at high risk of progressing to severe COVID-19 (see: “A closer look at the evidence for nirmatrelvir/ritonavir”).11 There is insufficient evidence to determine whether the use of antivirals during the acute COVID-19 phase reduces the risk of post-acute sequalae of COVID-19 (“long COVID”). Therefore, they are not currently recommended for this purpose,10 although this remains an active area of research.
People with certain factors or within specific population groups have been identified as being at increased risk of hospitalisation and death from COVID-19, and are, therefore, likely to benefit from COVID-19 antiviral treatment. This could be due to medical, personal or social factors. It is possible that recommendations may be revised over time as further evidence emerges. Table 1 lists medical co-morbidities and independent factors that increase the risk of severe COVID-19.
Demographic factors, vaccination status and co-morbidities influence risk
 Age. Increasing age is a predominant risk factor for severe outcomes (i.e. hospitalisation and death) from COVID-19.8, 12 This risk is reported to be particularly high in people aged over 70 years in New Zealand.6
Age. Increasing age is a predominant risk factor for severe outcomes (i.e. hospitalisation and death) from COVID-19.8, 12 This risk is reported to be particularly high in people aged over 70 years in New Zealand.6
 Ethnicity. Numerous New Zealand-based studies have shown that people of Māori and Pacific ethnicity experience higher rates of hospitalisation and mortality due to COVID-19.8, 12, 13 The effects remain after controlling for other variables, e.g. age, co-morbidities, socioeconomic deprivation.8, 12 Therefore, ethnicity is an important independent factor in determining patients at high risk of severe outcomes from COVID-19.
Ethnicity. Numerous New Zealand-based studies have shown that people of Māori and Pacific ethnicity experience higher rates of hospitalisation and mortality due to COVID-19.8, 12, 13 The effects remain after controlling for other variables, e.g. age, co-morbidities, socioeconomic deprivation.8, 12 Therefore, ethnicity is an important independent factor in determining patients at high risk of severe outcomes from COVID-19.
 High socioeconomic deprivation is associated with an increased risk of hospitalisation and mortality due to COVID-19.8, 14 An effect has also been observed independent of age, co-morbidities and ethnicity.8 This may include people living in overcrowded homes, with no fixed home, who are unemployed, have a lack of transport or an unreliable phone or internet connection. On a practical basis, this may mean that people who do not have a stable setting in which to recover from COVID-19, or a reliable means of caring for themselves, seeking help or responding to follow up, are likely to be at higher risk.
High socioeconomic deprivation is associated with an increased risk of hospitalisation and mortality due to COVID-19.8, 14 An effect has also been observed independent of age, co-morbidities and ethnicity.8 This may include people living in overcrowded homes, with no fixed home, who are unemployed, have a lack of transport or an unreliable phone or internet connection. On a practical basis, this may mean that people who do not have a stable setting in which to recover from COVID-19, or a reliable means of caring for themselves, seeking help or responding to follow up, are likely to be at higher risk.
A closer look at the evidence for COVID-19 outcomes by ethnicity and socioeconomic deprivation
Two studies and two national reports have provided evidence that Māori and Pacific ethnicity and socioeconomic deprivation are risk factors for severe outcomes from COVID-19.
- An epidemiological study conducted between 2020 and 2022 reported that Māori had approximately two to eight-fold higher risk of COVID-19, three-fold higher age-standardised hospitalisation risk and four-fold higher age-standardised mortality risk, compared to European/Other.13 Pacific peoples had approximately 9 – 35-fold higher risk of COVID-19, five-fold higher age-standardised hospitalisation risk and nine-fold higher age-standardised mortality risk, compared to European/Other.13
- A study published in 2021 that examined just under 2,000 COVID-19 cases, reported that after controlling for age and co-morbidities, Māori and Pacific peoples had 2.5 and three-fold higher odds of COVID-19-related hospitalisation, respectively12
- This study was not sufficiently powered to determine a statistically significant relationship between demographic factors and COVID-19 mortality, but higher odds of mortality were observed with increasing age and socioeconomic deprivation12
- An analysis published by the Public Health Agency in 2022 reported that Māori and Pacific ethnicity and high socioeconomic deprivation are independent risk factors for COVID-19 population mortality. Each group has double, 2.5 and triple mortality rates, respectively, after controlling for age.8 When adjusting for other variables, i.e. sex, ethnicity, co-morbidity and vaccination status, the risk of COVID-19 mortality was lower than when adjusted for age alone but remained higher in people of Māori and Pacific ethnicity. Data on the fully adjusted risk associated with socioeconomic deprivation were not available.8
- A report published in 2024 by the New Zealand Royal Commission inquiring into COVID-19 stated that in 2022, Māori and Pacific peoples had a 74% and 140% increased rate of hospitalisation and a 74% and 100% increased rate of mortality from COVID-19, respectively, compared to people of other ethnicities. After adjusting for socioeconomic deprivation and co-morbidity, the risks reduced but remained higher among these ethnic groups. Hospitalisation and mortality risk also increased with socioeconomic deprivation (including after adjusting for age, sex and ethnicity). For example, hospitalisation rates were 16%, 31%, 51% and 79% higher for Quintiles 2, 3, 4 and 5, respectively, compared to the least deprived.14
 Vaccination status influences the risk of progression to severe COVID-19.11, 15 People who were not fully vaccinated* against COVID-19 have been shown to be at greater risk of hospitalisation and mortality due to COVID-19 compared to those who were.6, 8 While most of the eligible population in New Zealand are vaccinated to some degree against COVID-19,1 there will be a very small group who in addition to never being vaccinated, have not been exposed to SARS-CoV-2 and will, therefore, have no COVID-19 immunity.6 This will likely result in more severe illness if infected with COVID-19.
Vaccination status influences the risk of progression to severe COVID-19.11, 15 People who were not fully vaccinated* against COVID-19 have been shown to be at greater risk of hospitalisation and mortality due to COVID-19 compared to those who were.6, 8 While most of the eligible population in New Zealand are vaccinated to some degree against COVID-19,1 there will be a very small group who in addition to never being vaccinated, have not been exposed to SARS-CoV-2 and will, therefore, have no COVID-19 immunity.6 This will likely result in more severe illness if infected with COVID-19.
* Considered to be those who had not received at least two primary doses of COVID-19 vaccine (a single dose of the Comirnaty JN.1 COVID-19 vaccine is now considered a primary course)
 Medical co-morbidities. People with co-morbidities, e.g. immunocompromised, cardiovascular or respiratory disease, experience poorer outcomes associated with COVID-19.11, 15 Data from New Zealand have shown that people with any co-morbidity had more than six times the risk of COVID-19 mortality than people without.8 After adjusting for age, sex, ethnicity and socioeconomic deprivation, having any co-morbidity has been associated with a 4.58-fold increased rate of hospitalisation and 4.25-fold increased risk of death, compared to those without co-morbidities.14 See Table 1 for a list of medical co-morbidities that are associated with a high risk of severe COVID-19.
Medical co-morbidities. People with co-morbidities, e.g. immunocompromised, cardiovascular or respiratory disease, experience poorer outcomes associated with COVID-19.11, 15 Data from New Zealand have shown that people with any co-morbidity had more than six times the risk of COVID-19 mortality than people without.8 After adjusting for age, sex, ethnicity and socioeconomic deprivation, having any co-morbidity has been associated with a 4.58-fold increased rate of hospitalisation and 4.25-fold increased risk of death, compared to those without co-morbidities.14 See Table 1 for a list of medical co-morbidities that are associated with a high risk of severe COVID-19.
Table 1. Medical co-morbidities and independent factors that increase risk of COVID-19 severity.8, 16
| Respiratory |
- Chronic lung or airway disease
|
| Cardiovascular and metabolic |
- Serious cardiovascular conditions, e.g. congestive heart failure, coronary artery disease, rheumatic heart disease, congenital heart disease
- Poorly controlled hypertension
- Diabetes
- Chronic kidney disease
- Morbid obesity (BMI ≥ 35 kg/m2)
|
| Mental health |
- Severe mental health conditions, e.g. schizophrenia, major depressive disorder, bipolar or schizoaffective disorder
- Accessing secondary and tertiary mental health and addiction services
- Mental health and addiction issues and currently homeless or without permanent housing
|
Other illness/disability |
- Chronic neurological or neuromuscular disease
- Severe haematological disorders
- Severe liver disease, e.g. cirrhosis
- Active cancer
- Significant developmental disability
|
Independent factors |
- Increasing age, i.e. aged > 70 years
- Māori or Pacific ethnicity
- High socioeconomic deprivation
- No immunity to SARS-CoV-2, i.e. not completed a primary course of COVID-19 vaccination and never had COVID-19 before
|
The access criteria for funded COVID-19 antivirals for people aged 50 – 64 years was amended from 1st September, 2025, to include all people aged 50 years and over with COVID-19 who are considered by their healthcare professional to be at high risk of hospitalisation or death from COVID-19.10 Previously, access was restricted to people aged ≥ 50 years if they were of Māori or Pacific ethnicity or had not yet completed a primary course of COVID-19 vaccination.10
This change is intended to give healthcare professionals more discretion as to which patients they consider to be at high risk due to factors not covered in other aspects of the access criteria (see below). Healthcare professionals can use their clinical judgement, including knowledge of COVID-19 epidemiology and risk factors, to prescribe COVID-19 antivirals to patients aged ≥ 50 years based on need.10 This may include consideration of the patient’s medical, personal and/or social factors and circumstances, such as ethnicity and access to healthcare, e.g. social or geographical isolation, lack of transport, unreliable phone or internet connection, housing issues (see: “Demographic factors, vaccination status and co-morbidities influence risk”).
People aged 65 years and over remain eligible for funded COVID-19 antiviral treatment based on age alone. People of any age can also access funded COVID-19 antivirals if they meet other criteria, e.g. if they are immunocompromised, have previously required care in the intensive care or high dependency unit for COVID-19, people with a disability or severe vulnerability due to medical conditions or a combination of risk factors (see box).10
A funding criteria flowchart and assessment tool for nirmatrelvir/ritonavir (Paxlovid) is available from Pharmac.
COVID-19 antiviral access criteria
Patients are eligible for funded COVID-19 antiviral treatment if they have:10
- Confirmed (or probable) symptomatic COVID-19, or symptoms consistent with COVID-19 and are a household contact of a positive case; AND
- Symptom onset within the last five days; AND
- No requirement for supplemental oxygen due to COVID-19 infection;* AND
- ANY of the following:
- Are aged ≥ 65 years; OR
- Are aged ≥ 50 years and considered by their healthcare professional to be at high risk of hospitalisation or death from COVID-19 due to factors not covered below; OR
- Are immunocompromised and not anticipated to reliably mount an adequate immune response to COVID-19 vaccination or infection; OR
- Had a previous admission to critical or high dependency care directly as a result of COVID-19; OR
- Has Down syndrome; OR
- Has sickle cell disease; OR
- Receives Disability Support Services from the Ministry of Social Development (previously administered by the Ministry of Disabled people | Whaikaha); OR
- Has pre-existing high risk due to a health condition and needs direct family/whānau or external disability care most days; OR
- Has pre-existing severe frailty and/or vulnerability due to one or more severe health conditions;† OR
- Has any combination of ≥ 3 high-risk factors for severe illness from COVID-19
N.B. The antiviral cannot be used concurrently with another COVID-19 antiviral.10
* Supplemental oxygen to maintain oxygen saturation > 93%, or at or above baseline, for patients with chronic resting hypoxia due to COVID-19 infection (excluding those with chronic resting hypoxia as a result of conditions other than COVID-19)
† Health conditions that include severe or very advanced disease including, but not limited to, severe neurological, cardiovascular, renal and respiratory conditions
So, how do you determine who is at high risk to meet criteria 4.2?
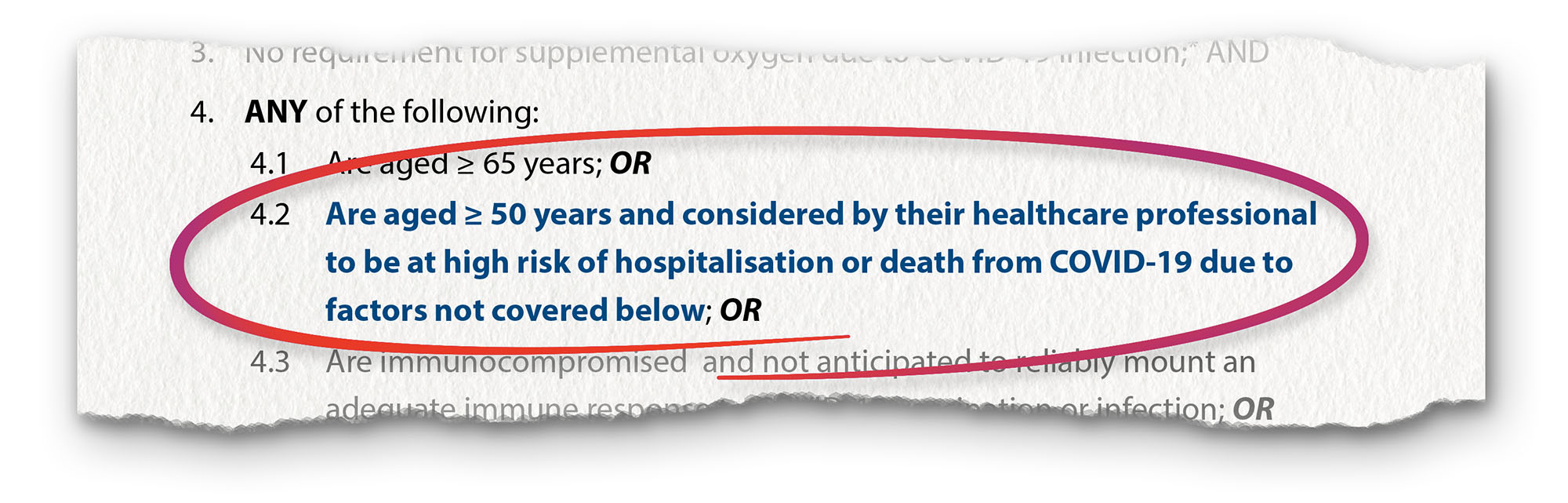
When deciding whether a patient needs a COVID-19 antiviral, if they clearly meet the listed access criteria, then treatment is appropriate, e.g. are aged ≥ 65 years, have three or more co-morbidities in Table 1. The decision to prescribe a COVID-19 antiviral to patients aged 50 years or over who are at high risk of hospitalisation or death due to factors not covered in other aspects of the criteria (i.e. to meet access criteria 4.2) comes down to clinical judgement of the individual circumstances of the patient. In general, consider COVID-19 antivirals in a patient aged 50 – 64 years if they have any of the following factors:
- Māori or Pacific ethnicity
- Socioeconomic deprivation, e.g. do not have a stable setting in which to recover from COVID-19, or a reliable means of caring for themselves, seeking help or responding to follow up
- Are not fully vaccinated against COVID-19 (primary course) and never had COVID-19 before
- One or two of the medical co-morbidities from Table 1 if there is clinical concern about the effect on recovery from COVID-19
While eligibility criteria have broadened, an equity approach to COVID-19 antivirals should continue to be implemented, given that it has been observed in some groups, e.g. Māori and Pacific, that uptake has not always matched clinical need, particularly in rural settings. Barriers to treatment include awareness of antiviral availability, logistical challenges of accessing treatment within the necessary timeframe, and variable clinician confidence with managing medicine interactions (see: “Check for potential medicine interactions”).
The remainder of this article covers the prescribing of nirmatrelvir/ritonavir (Paxlovid) as this is the medicine prescribed to patients with COVID-19 in a community setting. Information about remdesivir (Veklury), administered IV, for hospitalised patients at high risk of severe outcomes from COVID-19, is available from the NZF: https://nzf.org.nz/nzf_71144.
Nirmatrelvir/ritonavir (Paxlovid) is an oral combination protease inhibitor that blocks SARS-CoV-2 viral replication.7, 18 Ritonavir slows the metabolism of nirmatrelvir by inhibiting CYP3A4; this results in an increased plasma concentration of nirmatrelvir to a therapeutic level.7, 15 The combination medicine is approved for the treatment of COVID-19 in adults aged 18 years and over who do not require supplemental oxygen due to COVID-19 and are at increased risk of progression to hospitalisation or death.18 The management of COVID-19 in children and adolescents in the community should focus on vaccination, supportive care and referral to paediatric services when required.
Nirmatrelvir/ritonavir should be initiated as soon as possible once the patient has COVID-19; it must be started within five days of symptom onset to meet funding criteria.7 Treatment is more effective the earlier the medicine is started.19 A clinical review should be undertaken prior to prescribing nirmatrelvir/ritonavir to assess the patient’s suitability for treatment.7 This should include establishing whether the patient meets access criteria for funded treatment, reviewing their most recent eGFR result (if available) and checking for potential medicine interactions (see: “Prescribing nirmatrelvir/ritonavir: check eGFR to inform dosing” and “Check for potential medicine interactions”).7
Another aspect to consider when prescribing nirmatrelvir/ritonavir is managing patient expectations around COVID-19 antiviral treatment. Discuss with patients that taking the antiviral does not mean they will experience no symptoms or will not develop COVID-19 again in the future, but it will lower their risk of COVID-19 progressing to severe disease and being hospitalised or dying from COVID-19. Patients should still rest adequately during their recovery, e.g. not physically exert themselves too soon, as this helps to ensure best outcomes.
Endorse the prescription. The prescription for nirmatrelvir/ritonavir must be endorsed by the prescriber to confirm that the patient meets the access criteria for funded treatment. The following information should also be included on the prescription:7
Nirmatrelvir/ritonavir is also able to be supplied to some patients without a prescription by a registered pharmacist who has completed additional training (see: “Community pharmacist supply of nirmatrelvir/ritonavir”).7
A closer look at the evidence for nirmatrelvir/ritonavir
Most data on COVID-19 antiviral efficacy were collected prior to the emergence of the Omicron variant (currently predominant) and in unvaccinated populations. Many studies also used the criterion of PCR-confirmed SARS-CoV-2 infection, but PCR confirmation is no longer standard practice. High-quality studies assessing the effectiveness of nirmatrelvir/ritonavir in vaccinated populations exposed to the Omicron variant are limited.
Efficacy and adverse effects
The first trial showing efficacy of nirmatrelvir/ritonavir was the EPIC-HR clinical trial, which enrolled 2,246 participants from around the world (e.g. the United States, Europe, India) with COVID-19 who were not currently hospitalised, had no COVID-19 immunity* and were at high risk of progressing to severe COVID-19.19 Nirmatrelvir/ritonavir taken for five days was associated with a reduced risk of COVID-19-related hospitalisation or death from any cause by 88.9% (if taken within three days of symptom onset) and 87.8% (if taken within five days of symptom onset). This study also reported that the combination medicine was more effective the earlier it was started after symptom onset. The incidence of any adverse event during the treatment period was similar between those who took nirmatrelvir/ritonavir (22.6%) and placebo (23.9%). Most were of mild/moderate severity. There were fewer serious adverse events, e.g. pneumonia, and adverse events leading to treatment discontinuation in participants who took nirmatrelvir/ritonavir compared to placebo. Taste disturbances, diarrhoea and vomiting were reported more frequently in the nirmatrelvir/ritonavir treatment group.19
Since the EPIC-HR trial, numerous studies, systematic reviews and meta-analyses have reported the efficacy of nirmatrelvir/ritonavir in reducing COVID-19-related hospitalisations and death in high-risk groups.20–22 For example:
- A meta-analysis (published in 2024), including 32 studies (30 observational studies, two randomised controlled trials) and over two million people reported a pooled relative risk for the effect of nirmatrelvir/ritonavir on hospitalisation of 0.43 (95% CI: 0.37 – 0.51), mortality of 0.36 (95% CI: 0.25 – 0.52), hospitalisation and/or mortality of 0.52 (95% CI: 0.45 – 0.61) and progression to severe disease of 0.54 (95% CI: 0.41 – 0.73).23 N.B. Some of the studies included vaccinated patients exposed to the Omicron variant.23
- A population-based retrospective cohort study in Vienna, Austria (published in 2025) included over 12,000 people taking nirmatrelvir/ritonavir, predominantly exposed to the Omicron variant (most had some form of immunity against COVID-19) and not initially hospitalised.24 A lower risk of hospitalisation and all-cause mortality was reported in adults aged ≥ 60 years who took nirmatrelvir/ritonavir compared to controls. However, further studies are needed as the confidence intervals were wide and the number needed to treat was high.24
* Not vaccinated against COVID-19 and not previously exposed to SARS-CoV-2
Symptom resolution
It is uncertain whether nirmatrelvir/ritonavir has an effect on the symptoms of COVID-19. One study (including almost 1,300 vaccinated and unvaccinated people at high risk of severe disease from multiple geographic regions) reported that nirmatrelvir/ritonavir alleviated symptoms one day earlier than placebo (median: 12 days versus 13 days), but this was not a significant difference.25 Another study (including over 2,000 unvaccinated people at high risk of severe disease from numerous countries) reported a statistically significant reduction in the median time to sustained symptom alleviation by two days, compared to placebo (13 days versus 15 days).26
Antiviral resistance
Antiviral resistance is a theoretical concern with widespread use of nirmatrelvir/ritonavir, however, clinically significant resistance has not been observed to date.27 Ongoing genomic surveillance will be important to detect any emerging resistance patterns.
Future antiviral treatments
Several new COVID-19 antivirals are in development overseas, including an oral formulation of remdesivir. It is not known if, and when, these treatments may be available, or if they will be available in New Zealand. However, these developments highlight that evidence may frequently be updated and there is likely to be continual evolution of COVID-19 treatment strategies.
Community pharmacist supply of nirmatrelvir/ritonavir
Funded nirmatrelvir/ritonavir can be supplied without a prescription to eligible patients with COVID-19 by a registered pharmacist who has completed additional training.7, 10 A list of pharmacies offering this service is available here.
The pharmacist must have completed specific training and have the ability to access patients’ current medicines list and laboratory results, in particular eGFR (e.g. via regional clinical information sharing services or by contacting the patient’s usual healthcare provider).7 The pharmacist should ensure that the patient is well enough to be managed without further clinical assessment from their primary care clinician, and check the following prior to supplying nirmatrelvir/ritonavir:7
The training for pharmacists to supply nirmatrelvir/ritonavir without a prescription is offered through the Pharmaceutical Society of New Zealand. For further information, see: https://www.psnz.org.nz/Product?Action=View&Product_id=976.
Prescribing nirmatrelvir/ritonavir: check eGFR to inform dosing
Paxlovid is usually prescribed as 300 mg nirmatrelvir (two 150 mg pink tablets) and 100 mg ritonavir (one 100 mg white tablet), with instructions to be taken together, twice daily, for five days.18 A lower dose of nirmatrelvir is prescribed in renal impairment based on eGFR level, therefore the patient’s most recent result should be checked prior to prescribing. Ideally, the patient’s eGFR will have been measured within the last three to six months, but this is not a requirement for prescribing.7, 18 If a recent eGFR result is not available (or has never been done), request an urgent test if time permits, prescribe based on a historical result if renal function is presumed to be stable or prescribe a dose based on a conservative estimate of eGFR. Nirmatrelvir/ritonavir was previously contraindicated in patients with an eGFR < 30 mL/min/1.73 m2, but now can be considered in this group.17, 28
eGFR is used as an approximate measure of renal impairment and will be sufficient to estimate renal function for most patients. A full assessment of a patient’s renal function would also include urine albumin:creatinine ratio (ACR) and consideration of creatinine clearance (CrCl), especially in the case of severe renal impairment (but this is not a requirement prior to prescribing nirmatrelvir/ritonavir).
Prescribe nirmatrelvir/ritonavir according to the patients’ eGFR:28
- eGFR ≥ 60 mL/min/1.73 m2: no dose adjustment required – prescribe 300 mg nirmatrelvir (two tablets) and 100 mg ritonavir (one tablet), twice daily, for five days
- eGFR ≥ 30 – 59 mL/min/1.73 m2: reduce each dose of nirmatrelvir to 150 mg (one tablet), i.e. prescribe 150 mg nirmatrelvir (one tablet) and 100 mg ritonavir (one tablet), twice daily, for five days
- eGFR < 30 mL/min/1.73 m2:* for Day one, prescribe 300 mg nirmatrelvir (two tablets) and 100 mg ritonavir (one tablet). For Days two to five, prescribe 150 mg nirmatrelvir (one tablet) and 100 mg ritonavir (one tablet), to be taken once daily.
*Medicine datasheet updated in September, 2025, to include dosing for this group (previously a contraindication)
The medicine is supplied in pre-packaged blister cards containing 20 nirmatrelvir and ten ritonavir tablets. For patients prescribed lower doses due to renal impairment, pharmacists must ensure that any nirmatrelvir or ritonavir tablets that are not required are discarded prior to dispensing and the reason for this is discussed with the patient (i.e. if they only require one nirmatrelvir tablet per dose rather than two, or once daily dosing rather than twice).29 Renal dosing stickers are available from the supplier and can be used to cover the empty cavities as well as the pre-printed dosing instructions on the blister card (as they advise the patient to take three tablets at once).
No dose adjustment of nirmatrelvir/ritonavir is required in patients with mild hepatic impairment, but it should be avoided in patients with severe hepatic impairment.18
Nirmatrelvir/ritonavir during pregnancy and breastfeeding: limited data available
Nirmatrelvir/ritonavir is contraindicated by the manufacturer during pregnancy due to limited data.18 However, in practice, the increased risk of severe COVID-19 during pregnancy should be considered, and if the likely benefit of antiviral treatment outweighs the potential risks, then it may be appropriate to prescribe.18 It is best practice to seek obstetric and/or infectious diseases advice prior to deciding with the patient to prescribe nirmatrelvir/ritonavir during pregnancy.
The manufacturer also recommends avoiding nirmatrelvir/ritonavir in patients who are breast-feeding due to limited data.18 However, the amount excreted in breast milk is likely to be low and is not expected to adversely affect the infant. Therefore, if the benefits of treatment to the mother are likely to outweigh the possible risks to the infant, it may be appropriate to prescribe. Monitor the infant for adequate weight gain and symptoms such as vomiting, diarrhoea, difficulty feeding or sleeping and jaundice.18
Given that nirmatrelvir/ritonavir is contraindicated by the manufacturer during pregnancy, if it is prescribed to female patients of child-bearing potential, ensure they are advised to take extra contraception precautions during, and for one week after, treatment.7, 18 This is particularly important for patients prescribed oral contraceptives as ritonavir may affect the reliability of these medicines by reducing concentrations of ethinyloestradiol.7, 18
Check for potential medicine interactions
Ritonavir is a potent inhibitor of CYP3A4, therefore it may interact with other medicines;7, 11 check what medicines, including over-the-counter and complementary and alternative medicines, the patient is currently taking and the potential severity of any interaction. Common medicine interactions with nirmatrelvir/ritonavir include antiarrhythmics (e.g. amiodarone, digoxin), antithrombotics (e.g. rivaroxaban, dabigatran), statins (e.g. atorvastatin, rosuvastatin, simvastatin), benzodiazepines (e.g. diazepam), anticonvulsants (e.g. carbamazepine) and St John’s Wort.18, 30
The recommended COVID-19 antiviral interactions checker is the University of Liverpool COVID-19 Drug Interaction Checker. The NZF interactions checker can also be used.
Depending on the indication of the medicine and severity of the interaction, it may be appropriate to either temporarily stop the patient’s interacting medicine, reduce the dose or continue the medicine at the current dose but with close monitoring of the patient.7, 30 The risk/benefit of withholding the COVID-19 antiviral versus modifying the patient’s current treatment regimen should be considered; in many cases a temporary withdrawal of the interacting medicine or dose reduction is unlikely to have a clinically meaningful impact on the patient, given that a course of nirmatrelvir/ritonavir is only for five days.7, 30 If the patient is taking a medicine that is managed in secondary care, seek advice from the relevant specialist (e.g. nephrologist, oncologist, neurologist) before prescribing nirmatrelvir/ritonavir.7
Communicate changes clearly. If a change is being made to the patient’s existing treatment regimen so that they can safely take nirmatrelvir/ritonavir, this must be clearly communicated to them (ideally verbally and in writing).7 It is also good practice to include details of this on the prescription, so the pharmacist can reinforce the changes to the patient.
A full list of cautions and contraindications with nirmatrelvir/ritonavir are available from the NZF: https://nzf.org.nz/nzf_71162
An advance prescription can be provided
An advance prescription can be offered to patients based on need if they meet all aspects of the access criteria, except having COVID-19.7 For example, this might be appropriate for patients who live in rural areas given the narrow window between symptom onset and the time needed to initiate treatment by. Advise patients that the prescription is valid for 90 days and will only be dispensed once they have COVID-19 (i.e. meet all of the access criteria).7
Endorse the prescription as an advance prescription and note that the patient meets access criteria except for having COVID-19. Also include the patient’s eGFR and your contact details. The pharmacist will reassess the patient’s eligibility, eGFR and current medicines at the time of dispensing.7
Adverse effects are usually mild and self-limiting
Adverse effects experienced by patients taking nirmatrelvir/ritonavir are typically mild and self-limiting, such as taste disturbances and gastrointestinal upset, e.g. nausea, diarrhoea.18 Less commonly, hypertension and myalgia can occur.18 Advise patients to monitor for new or worsening symptoms or signs and to seek medical attention if there are any concerns.
COVID-19 rebound is possible
There have been reports of viral rebound and symptom recurrence in up to 10% of cases following COVID-19 antiviral treatment; usually this occurs within two weeks of initial symptom onset.7, 11 The exact mechanism by which this occurs is not currently known. However, viral rebound can also occur following SARS-CoV-2 infection in people who have not taken antivirals, which may suggest that it is part of the natural progression of COVID-19.7, 11 There is currently no clinically significant evidence that viral rebound is more likely in people who take COVID-19 antivirals compared to those who do not.31, 32
If COVID-19 rebound occurs after treatment, further antivirals are not recommended; most people experience mild symptoms that can be self-managed.7 If the patient has COVID-19 again 29 days or more after a prior infection, this should be regarded as a new infection, and nirmatrelvir/ritonavir may be considered if needed.7
The final word
Patients who are at high risk of severe outcomes from COVID-19 who meet the access criteria should be prescribed nirmatrelvir/ritonavir as they are likely to benefit from antiviral treatment. Also consider opportunistically advising at risk patients that they are eligible for antiviral treatment if they get COVID-19 to increase awareness of availability.
COVID-19 antiviral treatment must be initiated within five days of symptom onset to be effective. eGFR and medicine interactions are the predominant clinical considerations when prescribing nirmatrelvir/ritonavir to patients. Ensure that patients understand that treatment will not eliminate symptoms of COVID-19 or influence their risk of developing COVID-19 again in the future, but it will reduce their risk of experiencing severe outcomes, e.g. hospitalisation. Nirmatrelvir/ritonavir is generally well tolerated; therefore the potential benefit outweighs the risk for most people.
Ongoing research into COVID-19 antivirals and treatment advancements may change how at-risk patients with COVID-19 are managed in the future.
