Lactose is a disaccharide naturally found in dairy products including milk, yoghurt, cream, chocolate, ice cream and cheese.1 It
can also be used as a flavour enhancer in processed foods such as potato chips, crackers, margarine and bread.2
Lactose malabsorption. Approximately 70% of the world’s population aged ten years or older is affected
by lactose malabsorption, i.e. the failure to absorb lactose in the small intestine due to lactase deficiency or other intestinal
pathology, with most causes being genetically determined (see: “There are four types of lactase deficiency”).2,
3 People from Middle Eastern countries (70%), Asia (64%) and Africa (63 – 65%) have higher rates of lactose malabsorption,
while lower rates are reported in Eastern Europe, Russia and former Soviet Republics (47%), Northern America (42%) and Northern,
Western and Southern European countries (28%).3 Within Asia, the prevalence of lactose malabsorption is estimated
to range considerably; from 58% in Pakistan to 100% in South Korea.3 Both males and females are affected equally
worldwide.4
Lactose intolerance. When lactose malabsorption, i.e. the inability to digest lactose, causes gastrointestinal
symptoms it is referred to as lactose intolerance (see: “Gastrointestinal symptoms characterise lactose
intolerance”).2 Many people with lactose malabsorption will not develop lactose intolerance.2 The
likelihood of developing symptoms depends on the amount of lactose ingested, whether lactose is eaten with other foods that
affect transit through the intestine to the colon, the amount of lactase expression in the small intestine, composition
of the microbiome and history of gastrointestinal disorders or surgery.2
The estimated prevalence of lactose intolerance in New Zealand.
The prevalence of lactose intolerance is more difficult to estimate than lactose malabsorption as studies mainly rely
on self-reported symptoms during a lactose challenge, which are rarely blinded; self-reported lactose intolerance has a
sensitivity of 30 – 71% and specificity of 25 – 87%.2, 5 Of the limited New Zealand data available, an increased
prevalence of lactose malabsorption in Māori and Pacific peoples has been observed compared to New Zealand Europeans, based
on breath hydrogen testing (see: “Laboratory tests have a limited role in diagnosing lactose intolerance
in New Zealand”).6, 7 A study conducted in Christchurch in 2010 found that the overall prevalence of primary
lactose intolerance determined by genetic testing was 8% (among 1,064 participants); of the 30 Māori and Pacific participants,
the prevalence was 30%.8
There are four types of lactase deficiency that can result in lactose intolerance
Primary lactase deficiency is the most common cause of lactose intolerance (sometimes referred to as
lactase non-persistence or adult or late-onset lactose intolerance).2 Lactase concentrations reach their peak
around the time of birth in most people, and decline after the usual age of weaning.2, 9 The timing and rate
of this decline is genetically determined.10 Onset of primary lactase deficiency is typically subtle and progressive
over several years, with most people diagnosed in late adolescence or adulthood.2, 9, 10 However, acute development
is also possible.10
Secondary lactase deficiency (also referred to as acquired lactase deficiency) is transitory and can
occur after a gastrointestinal illness that alters the intestinal mucosa resulting in reduced lactase expression.2,
11 Secondary lactase deficiency is common in children after rotaviral (and other infectious) diarrhoea. Giardiasis,
cryptosporidiosis and other parasitic infections of the proximal small intestine often lead to lactose malabsorption.9 Secondary
lactase deficiency may also occur with coeliac disease, inflammatory bowel disease, small intestinal bacteria overgrowth,
cows’ milk protein allergy (CMPA)-induced enteropathy and immune-related illnesses such as HIV.9 In addition,
some medicines can cause villous atrophy resulting in secondary lactase deficiency, e.g. aminoglycosides, tetracyclines,
colchicine, chemotherapy treatments.12 Secondary lactase deficiency usually resolves after one to two months
but may be permanent if caused by a long-term condition.
Developmental lactase deficiency (neonatal) occurs in premature infants.9 This condition
is usually temporary and rapidly improves as the intestinal mucosa matures.9 Lactase and other disaccharidases
are deficient until after 34 weeks gestation.9
Congenital lactase deficiency (alactasia) is a life-long genetic condition involving the complete deficiency
of lactase expression from birth, despite the person having an otherwise normal intestinal mucosa.2 Alactasia
is extremely rare; it has been diagnosed in fewer than 50 people worldwide.2, 9
Gastrointestinal symptoms characterise lactose intolerance
In general, the symptoms of lactose intolerance are often non-specific, mild and vary between individuals.2, 11 Symptoms
usually occur between 30 minutes and a few hours after the ingestion of lactose.13 The severity of symptoms
is influenced by the degree of lactase deficiency and the amount of lactose consumed; typically the more lactose consumed,
the more frequent or severe the symptoms.13 In children, diarrhoea is often more pronounced, particularly those
with secondary lactose deficiency.9
Symptoms result from two main causes (see: “Pathophysiology of lactase deficiency”):2
- Undigested lactose acting as an osmotic laxative (diarrhoea, abdominal pain)
- Intestinal bacteria using lactose as a growth substrate, resulting in production of hydrogen, carbon
dioxide and methane gases (flatulence, dyspepsia, abdominal distension or borborygmi [stomach gurgling])
Pathophysiology of lactase deficiency
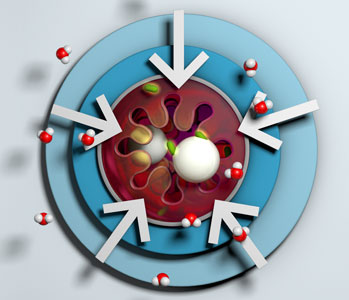
Lactase is an enzyme produced by cells located in the microvilli of the small intestine which hydrolyses dietary lactose
(a disaccharide sugar) into glucose and galactose (monosaccharide sugars) for transport across the cell membrane. In the
absence or deficiency of lactase, unabsorbed lactose causes an influx of fluid into the bowel lumen, due to osmotic pressure.
Unabsorbed lactose then enters the colon and is used as a substrate by intestinal bacteria, producing gas and short-chain
fatty acids via fermentation. The fatty acids cannot be absorbed by the colonic mucosa, therefore more fluid is drawn into
the bowel. A proportion of the lactose can be absorbed but the overall result of ingestion is a substantial rise of fluid
and gas in the bowel, causing the symptoms of lactose intolerance.2
Lactose intolerance is usually diagnosed by dietary challenge
- Step 1: Rule out other causes
- Step 2: Dietary challenge
- Step 3: Further investigation, if dietary challenge inconclusive
Lactose intolerance can be suspected in people who report gastrointestinal symptoms following the ingestion of milk or
milk products. An accurate diagnosis is important as it can significantly relieve a person’s anxiety and help them to avoid
inappropriate investigation and treatment. For people who present in primary care with severe or persistent gastrointestinal
symptoms, other potential causes should also be excluded (see: “Differential diagnoses to consider”). In particular, an
underlying secondary cause of lactose intolerance should be ruled-out in children, e.g. rotavirus infection, giardiasis
or coeliac disease. Self-diagnosis of lactose intolerance is not recommended as it could lead to unnecessary dietary restrictions
and expense, lack of essential nutrients and most importantly, failure to detect a more serious gastrointestinal problem;
other physiological and psychological factors can contribute to gastrointestinal symptoms that mimic lactose intolerance.14
A lactose-free diet should be trialled for two to four weeks when lactose intolerance is suspected.14 It
is important that all sources of lactose are eliminated, so patients should be advised to read food labels carefully to
identify “hidden” sources of lactose, which are particularly common in processed foods, e.g. whey, cheese, milk by-products,
milk solids, milk powder.14 Lactose can then be re-introduced to the diet. If symptoms improve during the two
to four week period and return when lactose is reintroduced, the diagnosis can be made.14
N.B. Some prescription and over-the-counter medicines e.g. oral contraceptive pills and nitrofurantoin (100 mg, modified
release), contain a small amount of lactose, but not enough to cause gastrointestinal symptoms in someone with lactose intolerance.11
If dietary challenge is inconclusive or self-reported symptoms are unreliable, further investigations may be required.
However, laboratory testing for lactose intolerance (see below) will often not provide a definitive diagnosis and the availability
of tests throughout New Zealand is variable.
Laboratory tests have a limited role in diagnosing lactose intolerance in New Zealand
Although laboratory testing is often cited in literature to aid in the diagnosis of lactose intolerance, most of these
tests are not widely accessible in New Zealand or not publicly funded, and some lack sensitivity and/or specificity. If
there is significant uncertainty concerning a diagnosis, consider asking your local laboratory if any additional tests are
available, such as:2, 9, 14
- Breath hydrogen test - measures
the level of hydrogen in exhaled air after ingestion of lactose, following overnight fasting. Currently considered the most
reliable laboratory method for diagnosing lactose malabsorption (sensitivity is 80 – 90%) but false negatives can occur
due to breath hydrogen production associated with other conditions unrelated to lactose digestion, e.g. gut motility disorders.
Breath hydrogen testing is usually not possible in young children due to the need for wearing a tight-fitting mask.
- Lactose tolerance test –
measures blood glucose levels after ingestion of lactose. Less reliable than the breath hydrogen test (sensitivity
is 75%). Requires significant adherence and is not suitable for children.
- Faecal pH test – non-specific
marker for lactose (or other carbohydrate) malabsorption. A pH of < 6.0 suggests lactose intolerance. Because of the
high rate of false-negative results, this test is only recommended in infants aged under two years.
- Faecal reducing substances –
another indirect test for lactose (or other carbohydrate) malabsorption. A positive test suggests an absence of the
corresponding enzyme. However, false negatives can occur if the person has not recently ingested lactose.
- Small bowel disaccharidases –
requires duodenal biopsy in secondary care. This test may occasionally be considered in the context of secondary
lactose intolerance where a gastroscopy is being performed to determine an underlying cause (e.g. coeliac disease, Crohn’s
disease, protracted diarrhoea).
- Genetic testing for hereditary lactase
persistence – tests for a cytosine (C)/thymine (T) single nucleotide polymorphism upstream of the lactase gene;
T/T or C/T genotypes are lactose tolerant, while C/C genotype is lactose intolerant15, 16
Do not routinely request skin prick or serum allergen-specific IgE tests as lactose intolerance is not immune
mediated. However, these tests may be considered to rule out CMPA if this is suspected.
N.B. There are various online allergy testing services marketed to the public. These are recommended against by the Australasian
Society of Clinical Immunology and Allergy (ASCIA) due to the potential for harms from misdiagnosis. The full ASCIA position
statement is available here:
www.allergy.org.au/images/stories/pospapers/ASCIA_HP_Evidence-Based_Vs_Non_Evidence-Based_Allergy_Tests_Treatments_2021.pdf
Differential diagnoses to consider
If a dietary challenge proves inconclusive, alternative diagnoses should be considered, including:17
- Irritable bowel syndrome
- Coeliac disease
- Diverticular disease
- Inflammatory bowel disease
- Bacterial infection, e.g. Clostridium difficile
- Parasitic disease, e.g. giardiasis
- Cystic fibrosis
- Inadvertent or excessive laxative ingestion,
e.g. in products that act as natural laxatives
- Mechanical bowel compromise
- Bowel neoplasm or polyp
Lactose does not need to be completely restricted
- Step 1: Confirm diagnosis of lactose intolerance
- Step 2: Determine how much lactose can be tolerated without symptoms
- Step 3: Encourage gradual reintroduction of milk and milk products – this usually improves symptoms and tolerance
The complete avoidance of all lactose-containing foods is not recommended to manage primary lactose intolerance.1 Instead,
people should start with a more restricted diet and gradually increase the consumption of lactose-containing foods according
to their individual tolerance level.18 Consistency is the key to building tolerance; continual exposure often
enhances the number and efficiency of colonic bacteria capable of metabolising lactose, thereby producing fewer symptoms.19 The
majority of people, including children, can tolerate up to 5 g of lactose (approximately ½ cup milk) on its own, and up
to one to two cups of milk in total per day, when eaten with other foods (e.g. cereal) or spread out across the day.1,
2 Consuming lactose with meals rather than on an empty stomach slows the release of lactose in the small intestine,
and people can experiment to see which foods are more tolerable.18
Some lactose-containing foods are better tolerated than others
Better tolerated dairy products include yoghurt with live culture and hard cheese (especially aged) because the lactose
is partially hydrolysed by bacteria during preparation and gastric emptying is slower due to their thicker consistency.1,
9 Dairy products with a higher fat content or higher osmolality are also better tolerated due to delayed gastric emptying,
e.g. ice cream or chocolate milk.20 Symptoms may be more severe with skim milk (green top) than whole milk due
to the higher lactose and lower fat content.1, 20
Probiotics may be beneficial for some people
Probiotic supplementation may be beneficial for symptom relief in some people with lactose intolerance by promoting lactose
digestion.21 A 2020 systematic review of randomised controlled trials found an overall positive association between
probiotic supplementation and reduced gastrointestinal symptoms of lactose intolerance, although the effect size varied
and the quality of evidence was low.21 Probiotic strains that were shown to be beneficial included Lactobacillus
acidophilus, L. reuteri, L. rhamnosus and L. bulgaricus, Streptococcus thermophilus and Bifidobacterium
longum (dose range 108 – 1011 colony-forming units [CFU] per day).21
Lactose-free milks and milk alternatives are usually not required
Lactose-free milk or milk alternatives are generally not necessary unless large quantities of milk are consumed, or in
the rare case of intolerance to even small amounts of milk (in which case lactose-free foods may also need to be considered).
If these alternatives are required, the milk substitutes selected should be fortified with calcium and vitamin D to prevent
deficiencies.22 For children aged under five years, almond, coconut, rice and oat milk alternatives should not
be used as the main milk source as they are not nutritionally adequate.22 Fortified soy milk is recommended if
an alternative to cows’ milk is required in children. N.B. Soy milk or infant formula is generally not advised in children
aged under 12 months (see: “Feeding options for infants”).23
Maintaining calcium and vitamin D intake when minimising lactose in the diet
Adequate calcium and vitamin D intake are particularly important during childhood and adolescence for optimal peak bone
mass.24 People with lactose intolerance should continue to have at least two servings of milk or milk products
daily if tolerated in multiple small doses or with food.22 If this is not possible, calcium-fortified milk or
fortified milk substitutes should be considered as tolerated, and the diet should be supplemented through intake of non-dairy
calcium-rich food, e.g. bony fish, tofu, dark green leafy vegetables and nuts and seeds.1, 22 As sunlight is
the primary source of vitamin D, all people should be advised to take a daily walk or other form of outdoor activity.25
Lactase enzymes may be helpful alongside dietary management
Lactase enzyme supplements (available over-the-counter, not funded) should be considered as an adjunct, not a substitute
for dietary management; if dairy products can be tolerated in small amounts, enzyme supplements are unnecessary.2 Enzyme
supplements may not completely relieve symptoms and it is difficult to determine the effective dose.2
Feeding options for infants with lactose intolerance
In general, infants with lactose intolerance should continue breastfeeding.9 Breastfeeding mothers do not have
to eliminate lactose containing foods from their diets; the amount of lactose present in breastmilk is largely independent
of maternal consumption.9 Formula-fed infants may initially require a lactose-free formula, but reintroduction
of lactose containing formula or foods should be trialled after two to four weeks, as tolerated.9 In New Zealand,
lactose-free and soy milk infant formulas are available from supermarkets and pharmacies (not funded). Ongoing use of soy
formula in infants aged under 12 months is generally not recommended, but could be considered in infants aged over six months
if they are unable to tolerate adequate quantities of cows’ milk formula.23 Lactose-free infant formula can be
used in infants from birth.26
N.B. For guidance on feeding for infants with CMPA, see: bpac.org.nz/2019/cmpa.aspx
Managing secondary lactose intolerance
Short periods of lactose intolerance are common in children following infectious diarrhoea.27 In infants aged
under three months or malnourished children, this may negatively influence recovery from the primary illness.28 A
meta-analysis of clinical trials found that a lactose-free diet in non-breastfed infants may reduce the duration of diarrhoea
by up to 18 hours.27 Diluting lactose-containing milk has not been shown to resolve diarrhoea earlier compared
to undiluted milk (low quality evidence).27 Breastfed infants with temporary lactose intolerance can continue
to safely breastfeed.9
In general, treatment of the cause of the secondary lactase deficiency will lead to restoration of lactase activity.9 Therefore,
a lactose-free diet is usually only required temporarily until secondary lactase deficiency resolves.
Lactose intolerance is NOT an allergy to milk
In cows’ milk allergy, children are allergic to the protein in milk.
CMPA is one of the most common food allergies in young children (prevalence of 2 – 3% of children before age three years).29 The
prevalence in adults is much lower (approximately 0.5%).30 CMPA is reported to resolve in approximately half
of children before age 12 months, and in up to 90% by age five years.31
There are two types of clinical manifestation of CMPA:29
- IgE-mediated (Immediate): Symptoms usually develop within minutes to one hour after ingestion of cows’
milk. Symptoms include eczema, urticaria, rhinitis, cough, wheezing, abdominal pain, vomiting, diarrhoea. Life threatening
anaphylaxis is possible but rare.
- Non-IgE mediated (Delayed): Symptoms typically occur more than two hours or even days following ingestion
of cows’ milk. Symptoms include vomiting, diarrhoea, blood in stools, with or without eczema.
Differentiating between lactose intolerance and CMPA:
- CMPA can manifest during breastfeeding (due to cows’ milk ingested by the mother), in an infant on a cows’ milk-based
formula or shortly after weaning. Lactose intolerance is usually seen after age two years.
- Infants with lactose intolerance may safely breastfeed without the need for any maternal dietary modification, but mothers
may need to remove dairy products from their diet if their infant is diagnosed with CMPA
- Children with lactose intolerance can usually tolerate small amounts of dairy products, whereas in milk allergy, small
traces usually cause symptoms. N.B. IgE mediated CMPA reactions typically have a more rapid onset than non-IgE-mediated
reactions or symptoms of lactose intolerance.29
- Differentiation is usually possible based on clinical symptoms
For further detail on the diagnosis and management of CMPA, see “Managing cows’ milk protein allergy in infants”,
available from: bpac.org.nz/2019/cmpa.aspx
Clinician’s Notepad: lactose intolerance
If a person reports gastrointestinal symptoms that consistently occur following the ingestion of milk or milk products
- First rule out other possible causes of symptoms –
particularly if symptoms are severe or persistent, e.g. irritable bowel syndrome, inflammatory bowel disease
-
Secondary causes should be strongly considered in children, e.g. rotavirus infection, giardiasis or coeliac disease
-
If there is no other obvious cause, a lactose-free diet should be trialled for two to four weeks; ensure the patient is aware of
“hidden” sources of lactose which are common in processed foods
-
At the end of the trial, the patient should re-introduce lactose; if symptoms have improved during the trial and return when
lactose is reintroduced, then this is sufficient to diagnose lactose intolerance
-
Do not routinely request skin prick or serum allergen-specific IgE tests unless cows’ milk protein allergy is
suspected as lactose intolerance is not immune-mediated
-
If the dietary challenge is inconclusive or there is uncertainty, discuss with your local laboratory whether additional testing
is available, e.g. breath hydrogen testing, or consult with a secondary care clinician
Management of lactose intolerance
-
Lactose usually does not need to be excluded from the diet; people should start with a more restricted diet and gradually
increase the consumption of lactose-containing foods according to individual tolerance level
- Most people can tolerate up to 5 g of lactose (approximately ½ cup milk) on its own, and up to one to two cups of milk
in total per day, when eaten with other foods or spread out across the day
-
Some lactose-containing foods are better tolerated than others, e.g. yoghurt with live culture or dairy products with higher fat content
-
Lactose-free milks and alternative milks are usually not required but if used (or if sufficient quantities of cow’s milk cannot be consumed)
must be fortified with calcium and vitamin D to meet the recommended intake
-
Probiotics or lactase enzyme supplements (not funded) may be beneficial for some people alongside dietary management, however,
these are not routinely required and efficacy varies
-
Infants with lactose intolerance should continue breastfeeding and the mother does not need to eliminate lactose from her
diet; lactose-free infant formulas are available, if required
-
A temporary lactose-free diet may be beneficial for people with secondary lactose intolerance, e.g. following a bout of infectious
diarrhoea, to promote recovery from the primary illness
