 View / Download pdf version of this article
View / Download pdf version of this article
Asthma in primary care
In New Zealand, nearly 500 000 people take medicines for asthma1; one in seven children and one in nine people
aged over 15 years. People with poorly controlled asthma have a reduced quality of life and are at increased risk of
hospitalisation. Factors influencing asthma control include asthma literacy and treatment adherence among patients,
and asthma management by health professionals.2
A stepwise approach to asthma management is recommended in New Zealand. This involves intensifying or reducing
treatment to allow patients to achieve and maintain asthma control and reduce their risk of exacerbations. The steps of treatment are outlined below:
-
Step One
Mild, intermittent asthma – SABA alone
Those with symptomatic asthma should be prescribed a short-acting beta2-agonist (SABA) such as salbutamol or terbutaline.
-
Step Two
More severe asthma, or symptoms uncontrolled – SABA and ICS
The addition of inhaled corticosteroids (ICS) may be beneficial for those whose symptoms are uncontrolled on Step One or whose asthma symptoms are more severe.
-
Step Three
Control not achieved at Step Two – add LABA
If control is not achieved with a SABA and an ICS preventer then additional treatment with a long acting beta agonist (LABA) should be considered.
Sample Asthma Patients
In 2015, Sample Medical Centre had 100 patients who were dispensed an asthma inhaler. The figures below show the
proportion of these patients on each treatment step. For comparison, the same proportions for similar practices and nationally are shown below.
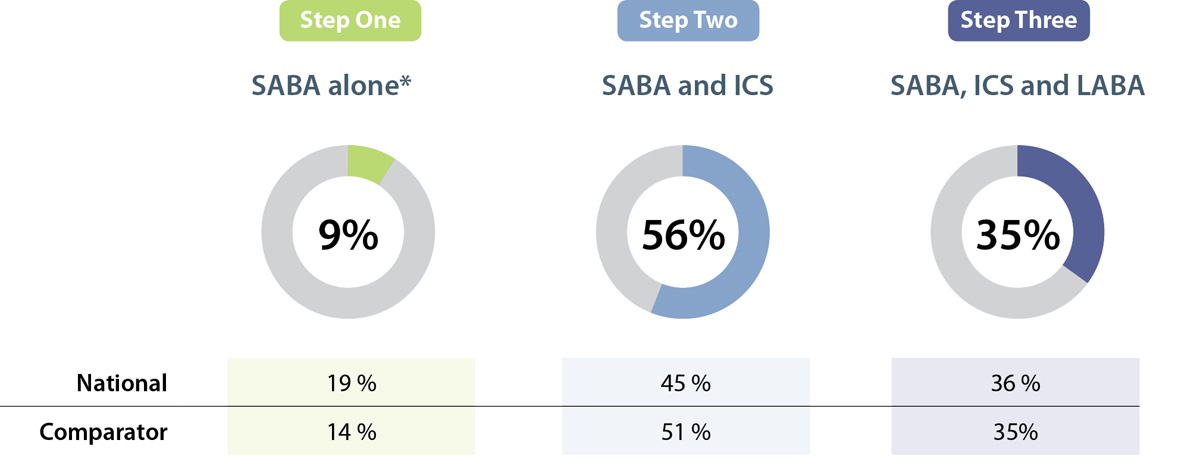
* Patients with >1 dispensing of a SABA were included in this category
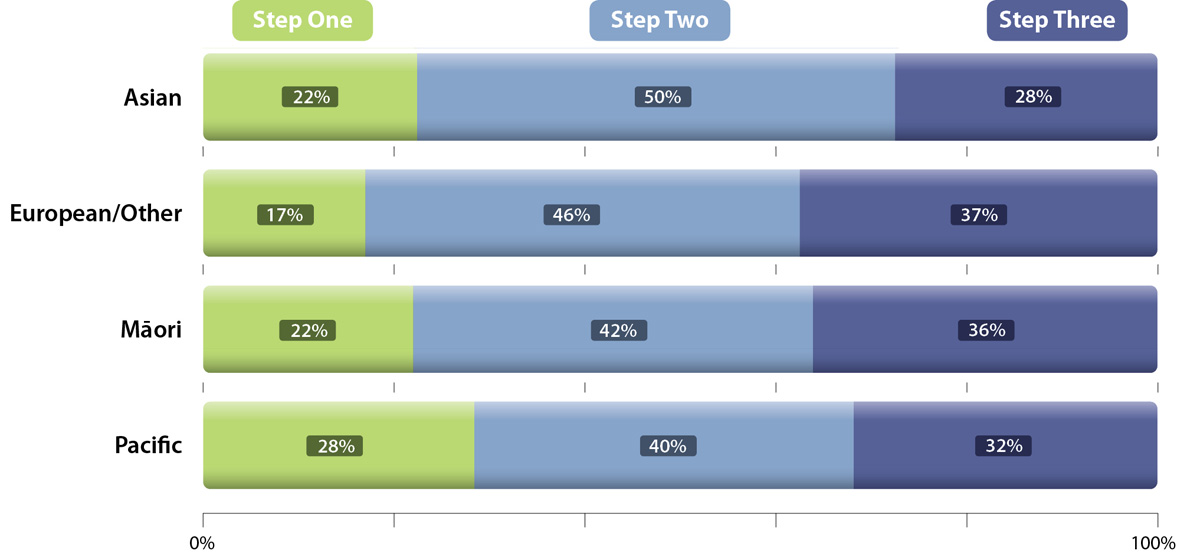
National Data by Ethnicity
Māori and Pacific peoples are more severely affected by asthma. Māori are almost three
times, and Pacific peoples over 3.5 times, more likely to be hospitalised due to asthma than people of other ethnicities
in New Zealand.3 Despite having a higher
prevalence and severity of asthma Māori and Pacific children are less likely to have their treatment escalated,4 and
it is likely that this is also true for Māori and Pacific adults with asthma. The figure below shows the proportion of
patients in New Zealand, dispensed medicines relating to each treatment step, by ethnicity, during 2015. These data show
that in comparison to New Zealand Europeans with asthma, those of other ethnicities have less escalation to step three,
despite being at higher risk of hospitalisation due to asthma.
Practice Points
- Most patients with asthma should be reviewed every three months
- Nominating an “asthma champion” in your practice ensures someone is responsible for checking that each patient is
receiving regular follow-up as well identifying the patients with the greatest unmet need
- An asthma audit may help you identify patients who are most in need of a review; including patients of Māori, Pacific or
Asian ethnicity or those who have been recently hospitalised due to asthma.
 For further information see: "Asthma
education in primary care", BPJ 70 (Sep, 2015)
For further information see: "Asthma
education in primary care", BPJ 70 (Sep, 2015)
References
- Pharmaceutical Collection, Ministry of Health, 2016
- Jones B, Ingham T, Reid S, et al. He Māramatanga Huangō: Asthma Health Literacy for Māori Children in New Zealand. 2015.
Available from:
www.health.govt.nz/publication/he-maramatanga-huango-asthma-health-literacy-maori-children-new-zealand
- Telfar Barnard L, Baker M, Pierse N, et al. The impact of respiratory disease in New Zealand: 2014 update. 2015.
Available from:
www.asthmafoundation.org.nz/research/the-impact-of-respiratory-disease-in-new-zealand-2014-update
- Gillies TD, Tomlin AM, Dovey SM, et al. Ethnic disparities in asthma treatment and outcomes in children aged under
15 years in New Zealand: analysis of national databases. Prim Care Respir J 2013;22:312–8.