In this article

View / Download pdf version of this article
Recent research into the use of medicines in New Zealand has revealed major differences in the number of prescriptions dispensed to Māori compared with non-Māori. Using data from the Ministry of Health National Collections for all prescriptions dispensed between 1 July 2006 and 30 June 2007, disparities were identified in a number of key areas, including medicines for cardiovascular disease, infectious diseases, diabetes and respiratory conditions.1 While this data is now five years old, it remains meaningful, and is the only available analysis of gaps in the prescribing of community pharmaceuticals to date. Further details will be available in the full analysis, planned for submission for publication later this year.
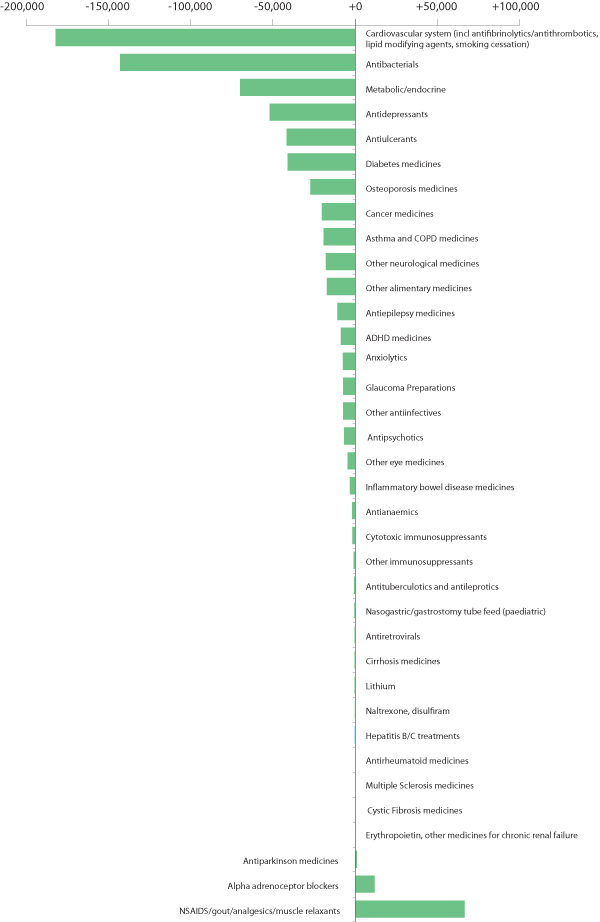
To make a comparison between the prescribing for Māori compared with non-Māori, the dispensing data was adjusted to account for population differences. The Māori population has a younger age structure than the non-Māori population,2 therefore the data was adjusted for age to account for the effects of a comparatively smaller ageing Māori population. The higher rate of disease, earlier onset and poorer outcomes experienced by Māori compared with non-Māori are also well known. To account for this, the data in Figure 1 has been adjusted for "Disability Adjusted Life Years" (DALY) in Māori. These adjustments were based on the Ministry of Health 2001 New Zealand Burden of Disease Study (NZBDS),3 which quantified the years of life lost by the New Zealand population in 1996 from premature mortality and disability caused by a number of diseases.
The adjusted data in Figure 1 shows that Māori have fewer prescriptions dispensed for pharmaceuticals to treat a number of key conditions. For example, in 2006/07 180,000 fewer prescriptions for cardiovascular medicines were dispensed to Māori than would have been expected in a comparable non-Māori population. Māori are also more likely to have unfilled prescriptions - the non-filling rate is almost 1.5 times that of non-Māori aged over 15 years.4 There is also evidence that Māori and Pacific peoples do not have their treatment escalated as frequently as non-Māori/Pacific peoples. Most recently, bpacnz examined how this affects prescribing for children with asthma, which demonstrated a lower proportion of Māori and Pacific children being escalated to long-acting beta-2 agonist treatment than children of other ethnicities, despite these populations experiencing a higher rate of severe asthma.5
While there are limitations of the data in Figure 1, including the inability to assess potential disparity in medicine use for Pacific peoples due to a lack of specific detailed ethnicity data in the published NZBDS data,3,6 it shows that there are differences between medicines dispensed to Māori and non-Māori, after adjusting for the most important confounding factors between the populations. This raises some important issues for health professionals to consider in the management of Māori patients.
Figure 1: Deficits (–) or excesses (+) in dispensed medicines for Māori compared with non-Māori, adjusted for age and relative disease burden (DALY loss)
1
References
- PHARMAC/Te Whaioranga. Gaps in use. 2009. Available from: www.tewhaioranga.co.nz (Accessed Jul, 2012).
- Statistics New Zealand. National ethnic population projections: 2006 (base) – 2026. Available from: www.stats.govt.nz (Accessed Jul, 2012).
- Ministry of Health. The burden of disease and injury in New Zealand. Public Health Intelligence Occasional Bulletin No. 1. 2001. Available from: www.moh.govt.nz(Accessed Jul, 2012).
- Ministry of Health. Tatau Kahukura: Māori Health Chart Book 2010, 2nd Edition. Available from: www.health.govt.nz (Accessed Jul, 2012).
- bpacnz . Data report: Prescribing for children with asthma. bpacnz , 2012. Available from: www.bpac.org.nz (Accessed Jul 2012).
- Ministry of Health. Priorities for Māori and Pacific health: evidence from epidemiology. Public Health Intelligence Occasional Bulletin No. 3. 2001. Available from: www.moh.govt.nz (Accessed Jul, 2012).