 View / Download pdf version of this sample report
View / Download pdf version of this sample report
Vitamin D is found naturally in some foods, but approximately 80% of our vitamin needs are derived from sunlight, when ultraviolet rays strike the skin and trigger vitamin D synthesis.
Vitamin D promotes calcium absorption in the gut and maintains adequate serum calcium and phosphate concentrations to enable normal bone mineralisation.
It is also needed for bone growth and remodeling. Without sufficient vitamin D, bones can become thin, brittle, or misshapen.
Vitamin D sufficiency prevents rickets in children and osteomalacia in adults.
Key messages
- Most people can achieve adequate levels of vitamin D through exposure to sunlight
- Testing vitamin D levels is rarely beneficial for patients, is expensive and often unreliable; in most cases deficiency is likely to be a consequence of poor health rather than a cause
- Vitamin D supplementation should be reserved for frail older people or those at risk of deficiency; routine supplementation for the general population is not recommended
- There is no evidence of vitamin D toxicity at doses recommended to treat mild deficiency, although this practice may increase the risk of renal tract stones
Vitamin D in our diet
Diet contributes approximately 5 - 10% of a person's vitamin D requirements. Natural sources of vitamin D are found in:
- Oily fish (e.g. salmon, tuna, sardines)
- Milk and milk products
- Eggs
- Liver
- Cod liver oil
Appropriate use of Vitamin D Supplementation1
Vitamin D supplementation of the general population is not recommended.
Supplementation is only beneficial for people at risk of deficiency such as, those who:
- Spend most of their time indoors
- When outside, cover up for cultural, medical or other reasons
- Have naturally very dark skin
- Are living in a rest home
- Are frail older people
- Have osteoporosis and inadequate dietary calcium intake
Colecalciferol is the recommended form of vitamin D for patients at risk of deficiency, who are unlikely to meet sun exposure recommendations.
Colecalciferol is contraindicated in renal failure, the hydroxylated derivatives alfacalcidol or calcitriol should be prescribed for these patients.
Vitamin D Testing
- Vitamin D supplementation can be initiated in people at risk of deficiency without the need for testing
- Testing of vitamin D levels is usually only indicated in patients with features of severe deficiency
- Vitamin D testing is requested as serum 25-hydroxyvitamin D (vitamin D)
- A serum level ≥ 50 nmol/L is generally considered to be sufficient to maintain adequate bone health, and levels < 25
nmol/L are considered to be deficient
Prescribing Trends
Over the past 8 years there has been a 124% increase in the number of patients dispensed vitamin D supplementation in New Zealand. In 2015,
this was the 12th most frequently prescribed medicine in the country. This suggests that vitamin D
is possibly being prescribed inappropriately to people who are not deficient nor at risk of vitamin D deficiency.
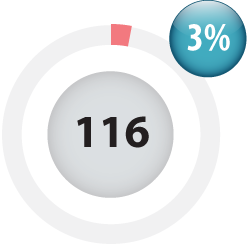
Sample Practice |
The wheel on the left shows that 116 patients at Sample Medical Centre were dispensed vitamin D in the past 12 months.
This accounted for 3% of your patient population. As a comparator, the wheel on the right shows the average number and
proportion of patients dispensed vitamin D by practices within your DHB. |
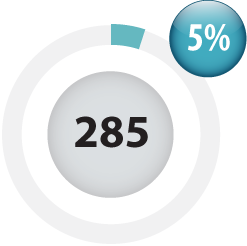
Average for practices in your DHB |
Table 1 below shows the proportion (and number) of patients dispensed vitamin D by 10 year
age bands at your practice, your comparator practices and nationally.
| Age (years) |
Sample Practice |
Your Comparator |
National |
| 0 – 9 |
0% (n = 0) |
0% |
0% |
| 10 to 19 |
0% (n = 1) |
1% |
1% |
| 20 to 29 |
0% (n = 0) |
2% |
1% |
| 30 to 39 |
1% (n = 3) |
2% |
2% |
| 40 to 49 |
2% (n = 9) |
4% |
3% |
| 50 to 59 |
2% (n = 10) |
7% |
6% |
| 60 to 69 |
9% (n = 31) |
13% |
11% |
| 70 to 79 |
15% (n = 29) |
22% |
19% |
| 80 + |
30% (n = 33) |
37% |
35% |
Practice Points
- A number of your patients may be receiving unnecessary vitamin D supplementation and/or testing – supplementation is only required for people at risk of deficiency
- Consider running an audit or review the need for repeats at the next consultation to determine if your patients may be able to stop their supplementation
 See BPJ 76 “Vitamin D and calcium supplementation in primary care: an update“ for more information
See BPJ 76 “Vitamin D and calcium supplementation in primary care: an update“ for more information
References
- Ministry of Health and Cancer Society of New Zealand. 2012. Consensus Statement on Vitamin D and Sun Exposure in New Zealand. Wellington: Ministry of Health