In 2011, bpacnz produced guidance on vitamin D supplementation for primary care. In the past five years vitamin D use
has risen substantially and it is now the 12th most frequently prescribed medicine in New Zealand. Previously, prescribing
vitamin D on the basis of deficiency risk was recommended, without testing. This is still broadly considered best practice,
however, it is now more evident which groups of patients are likely to benefit from supplementation. Dietary calcium should
be optimised in people taking vitamin D supplements, but routine supplementation with calcium is not recommended. Despite
the growing number of studies reporting associations between vitamin D deficiency and non-skeletal diseases, there remains
no convincing evidence of a causal link from meta-analyses or randomised controlled trials.
Vitamin D supplementation: an update
March 2025. bpacnz has published a new article on vitamin D supplementation, including updated dispensing data and 2024 New Zealand recommendations for vitamin D testing and supplementation during pregnancy and infancy.
See: Vitamin D supplementation: an update
 View / Download pdf version of this article
View / Download pdf version of this article
key practice points
- Most people can achieve adequate levels of vitamin D through exposure to sunlight
- Vitamin D supplementation should be reserved for frail older people or those at risk of deficiency; routine supplementation
for the general population is not recommended
- There is no evidence of vitamin D toxicity at doses recommended to treat mild deficiency, although this practice
may increase the risk of renal tract stones
- Testing vitamin D levels is rarely beneficial for patients, is expensive and often unreliable; in most cases deficiency
is likely to be a consequence of poor health rather than a cause
- Encourage an increase in dietary calcium before considering calcium supplementation, i.e. two to three serves of
dairy products a day
 For further information on vitamin D, see:
Vitamin D supplementation: Navigating the debate, BPJ 36 (Jun, 2011)
For further information on vitamin D, see:
Vitamin D supplementation: Navigating the debate, BPJ 36 (Jun, 2011)
Sunlight is the preferred source of vitamin D
People derive approximately 80% of their circulating vitamin D from the ultraviolet B (UV-B) rays in sunlight.1 Most
healthy people can achieve adequate vitamin D levels by spending time outdoors during the day. Skin needs to be exposed
to direct sunlight to allow the synthesis of vitamin D to occur as glass blocks UV-B rays.
How much sunlight is enough?
To prevent vitamin D deficiency, a daily walk in the early morning or late afternoon from September to April in the
Southern hemisphere with face, arms and hands exposed is recommended.1 At the height of summer as little
as six to eight minutes of sun exposure may be sufficient to produce 1000 IU of vitamin D.2 From May to August
outdoor activity is best scheduled around noon as approximately 30 – 50 minutes of sun exposure is required to
produce the same amount of vitamin D.1, 2 Dark skin pigmentation is correlated with decreased rates of vitamin
D production and people with darker skin may require three to six times more sun exposure to achieve equivalent
levels of vitamin D production.2 It is not possible to develop vitamin D toxicity due to exposure to sunlight.1
The use of sun beds to boost vitamin D levels is not recommended as this practice is associated with an increased risk
of melanoma which rises with greater use and earlier age of first use.1
Diet is a secondary source of vitamin D
Diet contributes approximately 5 – 10% of a person’s vitamin D requirement.2 Diet can be an important source
of vitamin D during winter months or when sun exposure is reduced. Cod liver oil is the best dietary source of vitamin
D while oily fish, e.g. salmon, tuna, eel and warehou, are rich whole food sources.1 Milk, yoghurt and margarine
fortified with vitamin D are now available in New Zealand.
Prescribing of vitamin D is increasing
As in 2011, guidance continues to recommend prescribing vitamin D supplements based on risk of deficiency (see below).1 However,
the number of people prescribed vitamin D each year is increasing (Figure 1) and it is questionable whether all of those
prescribed supplements are at risk of long-term deficiency. Colecalciferol (vitamin D3) is the predominant formulation
prescribed; in 2015 it was the 12th most frequently prescribed medicine in New Zealand.4
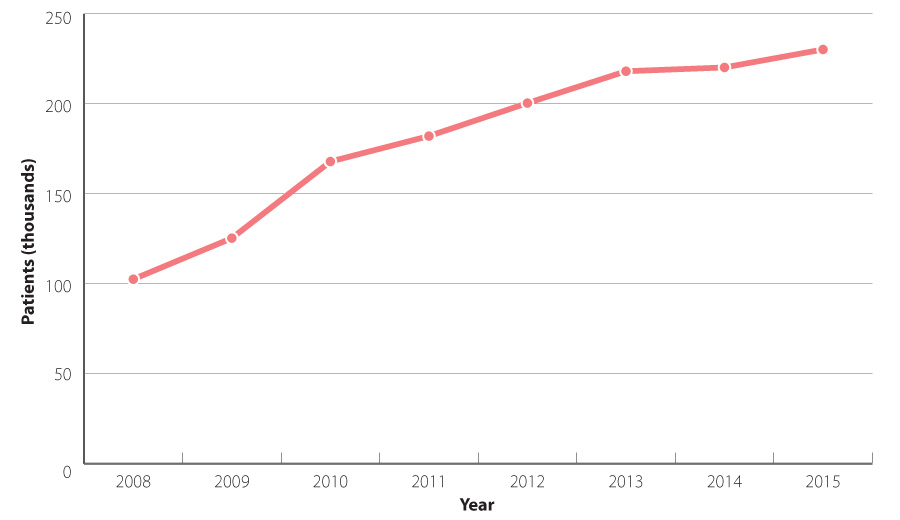
Figure 1: Number of patients dispensed subsidised vitamin D supplements in New Zealand (2008 – 2015).5
Benefits versus risks of vitamin D supplementation
Severe vitamin D deficiency reduces bone mineralisation which causes osteomalacia and increases fracture risk. This
can be prevented by empiric supplementation of people who are at risk. Since 2011, evidence has accumulated that only
a limited number of patients benefit from supplementation with vitamin D.
The benefits of supplementation on bone health and falls prevention have been overstated
More than 50 meta-analyses have examined the effects of vitamin D on falls or fractures.6 This research
now confirms that vitamin D supplementation for the general population provides no benefit and is a waste of resources.
Key findings from studies include:
- The United States Preventative Services Task Force concluded, in 2013, that daily supplementation with 400 IU (10 micrograms)
of vitamin D3 and 1000 mg of calcium has no effect on fracture incidence in post-menopausal women.7
- A meta-analysis involving more than 50 000 participants concluded that vitamin D taken without calcium has no effect
on fracture incidence and that vitamin D taken in combination with calcium has weak and inconsistent effects on fracture
risk; benefits were restricted to frail, older females living in institutions.8
- Analyses of randomised controlled trials involving almost 30 000 participants found that vitamin D with or without
calcium has no effect on the risk of falls.8
Adverse effects associated with vitamin D supplementation have been reported
Vitamin D taken at recommended doses, i.e. 1.25 mg per month or 10 – 20 micrograms (400 – 800 IU) per day, is generally
well tolerated and considered to be safe. There is no evidence of toxicity at doses of vitamin D3 below 25 micrograms
(1000 IU), daily, however, hypercalcaemia and hyperphosphatemia can occur at substantially higher doses, e.g. 50 000 IU
daily.10 Vitamin D supplementation in combination with calcium supplements is reported to increase the risk
of renal tract stones.7
In a randomised controlled trial it was found that single high doses of colecalciferol, e.g. 12.5 mg (500 000 IU) given
annually, were associated with an increased risk of falls and fractures in older women who were considered at high risk
of fracture (see: ”High and low levels of vitamin D can cause bone weakness”).9
Inconclusive research has created confusion
In addition to preventing osteomalacia, there are a plethora of health claims associated with vitamin D supplementation.
This has created confusion both for patients trying to make informed treatment decisions and for clinicians guiding their
care.
Numerous studies have examined associations between vitamin D deficiency and a range of conditions including: cardiovascular
disease, cancer, autoimmune and inflammatory diseases, neurodegeneration, cognitive impairment and mood disorders.10 Association
does not equate to causation, however, and randomised controlled trials show that vitamin D supplementation has little
or no effect on the non-skeletal illnesses studied; the meta-analyses reported also do not support the observational findings.11 It
is more likely that vitamin D deficiency is a marker of reduced health, rather than a cause of it.11
High and low levels of vitamin D can cause bone weakness
Vitamin D is thought to affect bone mineralisation by regulating circulating calcium.12 If levels of circulating
calcium are low, this is rectified through the stimulation of osteoclasts which cause bone resorption via secondary hyperparathyroidism,
thereby reducing bone mineralisation.12 High levels of vitamin D can also cause bone weakness by stimulating
osteoclasts directly.12 These two mechanisms explain why high and low levels are both associated with bone
weakness.
Prescribing vitamin D for those at risk of deficiency
Colecalciferol is the recommended form of vitamin D for patients at risk of deficiency,13 who are unlikely
to meet sun exposure recommendations.1
 Vitamin D undergoes hydroxylation in the kidney to its active form, therefore hydroxylated derivatives alfacalcidol
or calcitriol should be prescribed for patients with renal failure.13
Vitamin D undergoes hydroxylation in the kidney to its active form, therefore hydroxylated derivatives alfacalcidol
or calcitriol should be prescribed for patients with renal failure.13
Contraindications for colecalciferol include patients with hypercalcaemia, hypervitaminosis, metastatic calcification,
and renal osteodystrophy with uncontrolled hyperphosphatemia.13 The current subsidised brand of colecalciferol
contains soya oil in the gel capsule and is contraindicated in patients with soy allergy.17 People with a
history of peanut-induced anaphylaxis should also avoid this formulation as they may react to soya oil.
For mild to moderate vitamin D deficiency prescribe:13
- 1.25 mg (50 000 IU) colecalciferol, once a month
For moderate to severe vitamin D deficiency prescribe an initial loading dose of one capsule daily for up to ten days.
Vitamin D taken at these doses is associated with few adverse effects, however, it may raise concentrations of
calcium and phosphate in the plasma and urine,13 and increase the risk of renal tract stones and arterial deposits.
Patients with vitamin D deficiency due to malabsorption or liver disease often require higher maintenance doses and
consultation with an endocrinologist is recommended.13
Hypervitaminosis D from excessive supplementation has non-specific symptoms resulting from hypercalcaemia, including:
dehydration, vomiting, decreased appetite, irritability, constipation, fatigue and muscle weakness.1
When to consider vitamin D supplementation
Vitamin D supplementation is only beneficial for people at risk of deficiency such as frail older people, those with
dark skin and women who are veiled; supplementation of the general population is not recommended.1 Vitamin
D and calcium supplements are indicated for patients treated for osteoporosis if their dietary calcium intake is inadequate
(see below).13
 See: “Vitamin D supplementation during pregnancy and infancy” for guidance on prescribing vitamin D to women who are
pregnant or breast feeding.
See: “Vitamin D supplementation during pregnancy and infancy” for guidance on prescribing vitamin D to women who are
pregnant or breast feeding.
Risk factors for vitamin D deficiency
Groups considered to be at high risk of vitamin D deficiency who may benefit from supplementation include people:1
- With very dark skin pigmentation
- Who completely avoid the sun for medical reasons, e.g. they have had skin cancer or are using photosensitising
medicines long-term
- With reduced mobility who are frail or housebound and at risk of musculoskeletal pain and osteomalacia
People who completely cover their skin with clothing or veils will be at greater risk of vitamin D deficiency.1 Living
in southern regions means that transitory vitamin D deficiency is more likely to occur between the months of May and August.1
The symptoms of vitamin D deficiency
In children, vitamin D deficiency is associated with delayed tooth eruption and rickets.14
In adults, severe vitamin D deficiency causes osteomalacia with symptoms of bone pain and muscle weakness.14
Physiological changes consistent with osteomalacia in adults who are vitamin D deficient include:14
- Elevated alkaline phosphatase levels; often the earliest finding
- Low calcium levels
- Elevated parathyroid hormone levels, i.e. secondary hyperparathyroidism
- Low phosphate levels
Vitamin D testing is only indicated if severe deficiency is suspected
Vitamin D supplementation can be initiated in people at risk of deficiency without the need for testing.1 Testing
of vitamin D levels is usually only indicated in patients with features of severe deficiency.1 This includes
patients who may have:15, 16
- Metabolic bone disease or features such as unexplained fractures or bone pain
- Unexplained raised alkaline phosphatase, low calcium or phosphate levels
- Chronic kidney or liver disease
- Osteoporosis secondary to endocrine disorders, e.g. Cushing syndrome
- Malabsorption of dietary fat, due to conditions such as coeliac disease, previous intestinal surgery or gastric bypass
When vitamin D testing is requested serum 25-hydroxyvitamin D (vitamin D) is measured as it is a stable metabolite with
a plasma half-life of three weeks.2 The optimal serum vitamin D level is contentious: a serum level ≥ 50
nmol/L is generally considered to be sufficient to maintain adequate bone health,2 and levels below 25 nmol/L
are considered to be deficient.1 Day-to-day variations in serum vitamin D are small (5%), although levels
may decrease by as much as 20 nmol/L over winter compared to measurements taken during summer.2 Where severe
symptomatic vitamin D deficiency is suspected serum calcium, phosphate and alkaline phosphatase should also be tested.1
There is limited clinical value in testing vitamin D levels in patients without symptoms of deficiency because the results
of testing are difficult to interpret, as the optimum level of vitamin D is unknown and levels can vary substantially
between seasons.
Vitamin D supplementation during pregnancy and infancy
During pregnancy the same risk factors for vitamin D deficiency and recommendations for sun exposure apply as for the
general population.
In general, testing vitamin D levels is not recommended in either asymptomatic women who are pregnant or infants.15 Supplements
should be prescribed based on the risk of vitamin D deficiency.15
The same colecalciferol regimen subsidised for adults who are at risk of vitamin D deficiency, i.e. colecalciferol,
1.25 mg, monthly, may be beneficial for women who are pregnant and vitamin D deficient, or at high risk of deficiency;
this is not recommended for all women who are pregnant due to a lack of safety data.15 Women who are pregnant
who are at a lower risk of vitamin D deficiency may benefit from lower daily dosing, i.e. 10 micrograms per day of vitamin
D, especially during the third trimester.15 There is no 10 microgram vitamin D supplement subsidised in New
Zealand but this quantity of vitamin D is included in ante-natal multivitamin tablets that can be purchased over-the-counter.
Supplementation during infancy
Infants who are exclusively breastfed or who receive less than 500 mL of milk formula per day may benefit from vitamin
D supplementation if they also have one or more of the following risk factors:15
- Dark skin
- A mother who is vitamin D deficient or is at increased risk of becoming deficient
- A sibling diagnosed with rickets or hypocalcaemic seizures
- Being born preterm with a body weight less than 2.5 kg (refer to NZFC)
Vitadol C, containing vitamins A, D and C is the recommended supplement in New Zealand for infants.15 This
can be given as ten drops (0.3 mL, approximately 10 micrograms of colecalciferol) once per day.15 Due to the
high vitamin A concentration in Vitadol C this formulation is not appropriate for infants who are not deficient.15 It
is reasonable to wait until breastfeeding is well established in full-term babies before introducing vitamin D supplementation,
e.g. at six weeks of age (refer to NZFC).15
 Further information on vitamin supplementation during pregnancy or infancy is
available from:
www.health.govt.nz/system/files/documents/publications/companion-statement-vit-d-sun-exposure-pregnancy-infancy-v3.pdf
Further information on vitamin supplementation during pregnancy or infancy is
available from:
www.health.govt.nz/system/files/documents/publications/companion-statement-vit-d-sun-exposure-pregnancy-infancy-v3.pdf
Optimising calcium intake
Increasing dietary calcium is preferred over oral calcium supplementation for patients prescribed vitamin D supplements;
both are associated with increases in bone mineral density of 1 – 2%,18 although calcium supplementation
is associated with some adverse effects (see below). It should be noted, however, that modest changes in bone mineral
density of this magnitude are unlikely to result in a reduced fracture risk for most patients.18
Dietary sources of calcium
The recommended daily intake of calcium in New Zealand is:19
- 1000 mg for men and women aged 19 – 70 years
- 1300 mg for men and women aged over 70 years
Dairy products are the richest source of calcium and two to three serves, e.g. a cup of milk, a pottle of yoghurt or
two slices of cheese, per day will maintain adequate calcium intake.19
Oral calcium supplements may be associated with adverse effects
Serum calcium levels are slightly elevated in the short term by taking oral calcium supplements.7 People
who ingest an equivalent amount of calcium from their diet do not experience the same elevations in serum calcium.7 Since
vascular calcification is an established risk factor for cardiovascular disease it has been suggested that calcium supplementation
may increase cardiovascular risk.7
Calcium supplementation is known to be associated with increased rates of:20
- Renal tract stone formation
- Constipation
- Gastrointestinal symptoms
- Cardiovascular events, including myocardial infarction
A 2015 meta-analysis concluded that due to the limited benefits of calcium supplementation and the increased risk of
relatively serious adverse events, calcium supplements should not be recommended for individuals or at a population level.20
The final word
It has become clearer since 2011 that the proportion of the population who are likely to benefit from vitamin D supplementation
is relatively small and restricted to frail older patients and those at risk of deficiency. The prescribing of vitamin
D to nearly one-quarter of a million people in New Zealand therefore may not be justified. When discussing new or ongoing
supplementation with patients who do not have a clear indication for treatment, an evidence-based conversation about the
likelihood of benefit may be helpful.
Acknowledgement
Thank you to Professor Ian Reid, School of Medicine, University of Auckland for expert review of this article.
References
- Ministry of Health and Cancer Society of New Zealand. Consensus statement on vitamin D and sun exposure in New Zealand.
Wellington: Ministry of Health. 2012. Available from: Available from: www.health.govt.nz/system/files/documents/publications/vitamind-sun-exposure.pdf (Accessed
Apr, 2014).
- Kyle C (Ed). Sonic pathology handbook: a guide to the interpretation of pathology tests. New South Wales: Sonic Healthcare
2014. Available from: www.snp.com.au/ (Accessed Mar, 2016).
- Amirthalingam G, Andrews N, Campbell H, et al. Effectiveness of maternal pertussis vaccination in England: an observational
study. The Lancet 2014;384:1521–8. http://dx.doi.org/10.1016/S0140-6736(14)60686-3
- bpacnz . 2015 Annual Practice Report. 2015. Available from: www.bpac.org.nz (Accessed
Dec, 2015).
- Ministry of Health. Pharmaceutical Claims Collection. 2016.
- Bolland MJ, Grey A, Reid IR. Vitamin D supplements do not prevent falls. BMJ 2016;353:i3005 http://dx.doi.org/10.1136/bmj.i3005
- Moyer VA, U.S. Preventive Services Task Force*. Vitamin D and calcium supplementation to prevent fractures in adults:
U.S. Preventive Services Task Force recommendation statement. Ann Intern Med 2013;158:691–6. http://dx.doi.org/10.7326/0003-4819-158-9-201305070-00603
- Bolland MJ, Grey A, Reid IR. Should we prescribe calcium or vitamin D supplements to treat or prevent osteoporosis?
Climacteric J Int Menopause Soc 2015;18 Suppl 2:22–31. http://dx.doi.org/10.3109/13697137.2015.1098266
- Sanders KM, Stuart AL, Williamson EJ, et al. Annual high-dose oral vitamin D and falls and fractures in older women:
a randomized controlled trial. JAMA 2010;303:1815–22. http://dx.doi.org/10.1001/jama.2010.594
- Glendenning P, Inderjeeth CA. Controversy and consensus regarding vitamin D: Recent methodological changes and the
risks and benefits of vitamin D supplementation. Crit Rev Clin Lab Sci 2016;53:13–28. http://dx.doi.org/10.3109/10408363.2015.1074157
- Glendenning P, Chew GT-J. Controversies and consensus regarding vitamin D deficiency in 2015: whom to test and whom
to treat? Med J Aust 2015;202:470–1.
- Reid IR, Bolland MJ, Grey A. Effects of vitamin D supplements on bone mineral density: a systematic review and meta-analysis.
Lancet 2014;383:146–55 http://dx.doi.org/10.1016/S0140-6736(13)61647-5
- New Zealand Formulary (NZF). NZF v48. 2016. Available from: www.nzf.org.nz (Accessed
Jul, 2016)
- Bhan A, Rao AD, Rao DS. Osteomalacia as a result of vitamin D deficiency. Endocrinol Metab Clin North Am 2010;39:321–331,
table of contents. http://dx.doi.org/10.1016/j.ecl.2010.02.001
- Ministry of Health (MoH). Companion statement on vitamin D and sun exposure in pregnancy and infancy in New Zealand.
Wellington: Ministry of Health. 2013. Available from: www.health.govt.nz/publication/companion-statement-vitamin-d-and-sun-exposure-pregnancy-and-infancy-new-zealand (Accessed
May, 2016).
- Ferrari R, Prosser C. Testing vitamin d levels and choosing wisely. JAMA Intern Med 2016; [Epub ahead of print]. http://dx.doi.org/10.1001/jamainternmed.2016.1929
- MEDSAFE. Safety information: Vit.D3 - important information for patients with a peanut or soya allergy. 2016. Available
from: www.medsafe.govt.nz/safety/EWS/2016/AlertVitaminD.asp
- Tai V, Leung W, Grey A, et al. Calcium intake and bone mineral density: systematic review and meta-analysis. BMJ
2015;351:h4183 http://dx.doi.org/10.1136/bmj.h4183
- New Zealand Nutrition Foundation. Calcium. 2014. Available from: http://www.nutritionfoundation.org.nz/nutrition-facts/minerals/calcium (Accessed
May, 2016).
- Bolland MJ, Leung W, Tai V, et al. Calcium intake and risk of fracture: systematic review. BMJ 2015;351:h4580 http://dx.doi.org/10.1136/bmj.h4580