In this article 
View / Download pdf
version of this article
| Key concepts: |
- Stroke needs to be dealt with immediately – “time is brain”
- Patients with sudden onset of neurological symptoms should be screened with the FAST tool
- Patients with symptoms suggestive of stroke should be referred to secondary care management immediately
- Do not give aspirin or attempt to reduce blood pressure in the acute setting
|
Stroke can be thought of as a “brain attack”, which like a heart attack, needs to be dealt with immediately
– “time is brain”. Rapid access to secondary care management can improve patient outcomes.
Stroke is the third most common cause of death in New Zealand
Approximately 22 strokes occur each day in New Zealand. Although the incidence of stroke increases with age a quarter
of people who have a stroke will be under 65 years. The average age of onset of stroke is around ten years lower for Māori
and Pacific peoples compared to European people.
Stroke is the third most common cause of death in New Zealand. Approximately 11% of people with ischaemic stroke and
30% of those with haemorrhagic stroke will die within the first month. Compared to other OECD countries New Zealand has
below average stroke survival rates.1
Stroke is a significant cause of disability and institutionalisation. Approximately two-thirds of stroke survivors will
have some level of disability one year after a stroke. Half of all stroke survivors remain permanently disabled.2
Common causes of stroke:
- Thrombosis and atheroma within an artery
- Athero-thromboembolism (e.g. from carotid arteries)
- Heart emboli (atrial fibrillation, infective endocarditis, myocardial infarct)
- Central nervous system bleed (hypertension, head injury, aneurysm rupture)
- Systemic hypotension and shock
- Vasculitis e.g. giant cell arteritis
- Arterial dissection, most commonly vertebral and carotid arteries
- Venous-sinus thrombosis
Recognising a stroke
The predominant symptom of stroke is sudden loss of neurological function e.g. paralysis or numbness. However other
neurological conditions may also mimic these symptoms, such as migraine, head trauma, brain tumour and post-ictal paralysis
(Todd’s Palsy). Hypo- or hyperglycaemia, renal or hepatic failure, infection and drug intoxication may also present
with some of the same symptoms as stroke.
Symptoms of a stroke typically:
- Start suddenly - the patient, or witness, is certain when the event began
- Have maximal neurological deficit at the onset - progressive symptoms imply another diagnosis
- Are focal - representative of loss of blood supply to one part of the brain
- Involve loss of neurological function e.g. paralysis or numbness
Transient ischaemic attack (TIA) is classically defined as stroke signs and symptoms that resolve within 24 hours. However,
most transient symptoms that last for more than one hour are in fact small strokes.
The exact pattern of neurological deficit in stroke depends on which artery is involved.
Use the FAST tool to screen for stroke
Patients with sudden onset of neurological symptoms suggestive of a stroke should be screened with a validated tool
such as FAST (see below). It is recommended that hypoglycaemia is excluded first.
The limitation of FAST is that it may not detect less common presentations of acute stroke or TIA, such as people with
visual field defects, disorders of perception, balance, or coordination or unilateral weakness confined to the leg.
FAST |
FACIAL WEAKNESS – Can the patient smile?
Ask patient to smile or show teeth.
- Look for new asymmetry – is there unequal smile or grimace, or obvious facial asymmetry?
ARM WEAKNESS – Can the person raise both arms?
Lift the patient’s arms together at 90 degrees if sitting, or 45 degrees if supine, and ask them to hold in
position for five seconds. Then let go.
- Does one arm drift down or fall down rapidly?
SPEECH PROBLEMS – Can the person speak clearly?
If the patient attempts conversation.
- Look for new disturbance of speech (check with witness)
- Look for slurred speech
- Look for word-finding difficulties. This can be confirmed by asking the patient to name commonplace objects that
may be nearby, such as a cup, chair, table, keys, pen
- If there is a severe visual disturbance, place an object in the patient’s hand and ask him/her to name it.
TIME TO REFER
If there is any neurological deficit, consistent with stroke or TIA, do not delay: Arrange to transfer the patient
immediately to secondary care.
(Adapted from NICE 20083) |
Acute stroke treatment
Patients with symptoms suggestive of stroke should be referred to secondary care management immediately.
- Arrange urgent admission to the nearest hospital with facilities for brain imaging
- Do NOT give aspirin. In contrast to a resolved TIA (or MI), aspirin should not be given to individuals with ongoing
symptoms until brain imaging excludes haemorrhage
- Do NOT attempt to reduce blood pressure in the acute setting
Immediate referral may not be appropriate for some individuals with severe co-morbidities or a terminal illness.
The main aim of acute stroke management is to preserve life, reverse or limit brain damage and prevent complications.
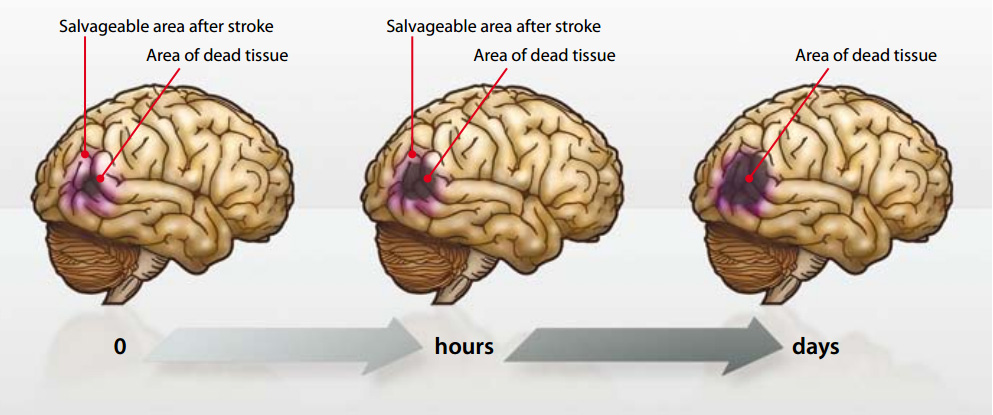
“Time is brain”
Urgent brain imaging, such as CT or MRI scan, is required to rule out haemorrhage before thrombolysis or for those whose
clinical condition is poor e.g. severe headache, progressive symptoms, reduced level of consciousness. All other people
with stroke should ideally be imaged within 24 hours and certainly within 48 hours.
Thrombolysis is recommended as first-line treatment for ischaemic stroke for people who meet specific criteria (see
below), however it is currently only available in a limited number of locations around New Zealand. Similar to acute
MI there is a small window where thrombolysis is of benefit for ischaemic stroke – up to 4.5 hours, but ideally within
three hours.4
“Time” is quite literally “brain” and the sooner the treatment is given, the greater the chance
of a successful outcome.
Acute stroke treatment in secondary care
Stroke units improve outcomes
Clinical trials have demonstrated clear benefits of rapid access to dedicated stroke units (similar to cardiac care
units). Stroke units achieve approximately 20% better survival rates than usual care.5 The positive impact
of aspirin and early thrombolysis for ischaemic stroke has improved survival and reduced disability.6,7 The
message is clear: organised stroke care saves lives and reduces disability. Currently there are stroke units in most major
centres in New Zealand and other areas are in the process of establishing units.
Acute thrombolysis with alteplase
Alteplase (recombinant tissue plasminogen activator - tPA) is recommended as first-line treatment for ischaemic stroke,
for people who meet specific inclusion criteria (see below), by most national and international
guidelines. Treatment within 4.5 hours of stroke onset has been shown to be safe and effective.8
Patients treated with alteplase are at least 30% more likely to have little or no disability at three months than those
who did not receive this treatment.9 If treated within one hour the estimated number of patients needed-to-treat
(NNT) to see benefit is only three. By 4.5 hours the NNT to prevent one death or disability has risen to 14.10
Acute antiplatelet therapy with aspirin for ischaemic stroke
After exclusion of haemorrhagic stroke, aspirin (150–300 mg) is given as early as possible, although delayed one or
two days if thrombolysis is given. Aspirin reduces the risk of death and recurrent stroke.11 It is recommended
that aspirin is continued as part of a long-term antithrombotic treatment regimen.
Decompressive hemicraniectomy
In rare occurrences, a patient with a large middle cerebral artery infarct may progressively deteriorate in their level
of consciousness, and have reduced ventilatory drive during the first 24–48 hours. In this instance, prognosis is very
poor without intervention and these patients require decompressive hemicraniectomy, which relieves intracranial pressure
from swelling of brain tissue.
Removal of a substantial area of skull and dura allows the brain to expand without compressing other brain structures.
At six weeks to six months after removal, the stored bone flap, or an artificial replacement, is used for reconstituting
cranioplasty.12
| Eligibility for thrombolysis in New Zealand |
Inclusion criteria:
- Age 18 – 85 years
- Clinical diagnosis of ischaemic stroke causing measurable neurological deficits
- Clearly defined onset of symptoms within three hours of treatment initiation (a patient must not have woken from
sleep with symptoms)
- Patient able to undergo CT before tPA administration
|
Exclusion criteria are numerous, some examples are:
- Coma
- Minor or non-disabling stroke symptoms
- History of stroke in previous 12 weeks
- Myocardial infarction within the past 30 days
- Conditions involving increased risk of bleeding e.g. recent trauma, ulcerative wounds, thrombocytopenia
|
 See “New Zealand protocols for the management of stroke
and TIA” for a full list of inclusion and exclusion criteria. Available from:
www.stroke.org.nz/pdfs/SUNNZguidelines.pdf See “New Zealand protocols for the management of stroke
and TIA” for a full list of inclusion and exclusion criteria. Available from:
www.stroke.org.nz/pdfs/SUNNZguidelines.pdf |
Acknowledgement
Thank you to Dr Gerry McGonigal, Clinical Leader, Capital & Coast DHB Rehabilitation Service, Wellington,
for expert guidance in developing this article.
References
- Organisation for economic co-operation and development (OECD). Health at a glance 2009: OECD indicators. OECD, 2009.
Available from:
http://www.oecd.org/document/11/0,3343,en_2649_33929_16502667_1_1_1_37407,00.html (accessed
January, 2010).
- Warlow C, Sudlow C, Dennis M, et al. Stroke. Lancet 2003;362(9391):1211-24.
- National Institute for Health and Clinical Excellence (NICE). Diagnosis and initial management of acute stroke and
transient ischaemic attack (TIA). NICE, 2008. Available from:
www.nice.org.uk/cg068 (Accessed January, 2010).
- Hacke W, Kaste M, Bluhmki E. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med
2008;359(13):1317-29.
- Seenan P, Long M, Langhorne P. Stroke units in their natural habitat: systematic review of observational studies.
Stroke 2007;38(6):1886-92.
- Sandercock PAG, Counsell C, Gubitz GJ, Tseng MC. Antiplatelet therapy for acute ischaemic stroke. Cochrane Database
Syst Rev 2008;3:CD000029.
- Wardlaw JM, Murray V, Berge E, del Zoppo GJ. Thrombolysis for acute ischaemic stroke. Cochrane Database Syst Rev
2009;4:CD000213.
- Hacke W, Donnan G, Fieschi C, et al. Association of outcome with early stroke treatment: pooled analysis of ATLANTIS,
ECASS, and NINDS rt-PA stroke trials. Lancet 2004;363:768–74.
- The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. Tissue plasminogen activator
for acute ischemic stroke. N Engl J Med 1995;333:1581–87.
- Saver JL. Number needed to treat estimates incorporating effects over the whole range of clinical outcomes: novel
derivation method and application to thrombolytic therapy for acute stroke. Arch Neurol 2004; 61: 1066–70.
- Chen ZM, Sandercock P, Pan HC, et al. Indications for early aspirin use in acute ischemic stroke : A combined analysis
of 40 000 randomized patients from the Chinese acute stroke trial and the international stroke trial. On behalf of the
CAST and IST collaborative groups. Stroke 2000;31(6):1240-9.
- Kohrmann M, Schwab S. Hemicraniectomy for malignant middle cerebral artery infarction. Curr Opin Crit Care 2009;15(2):125-30.