Asthma is “chronically common” amongst New Zealand children
Symptoms of wheeze or asthma most commonly develop in early childhood. However, in 50-75% of children, these symptoms
resolve by adulthood.2 Accurate diagnosis and management will allow children with asthma to have a quality
of life no different from children without asthma. Poor management, incorrect diagnosis, under or over-prescription of
medicine can lead to lower quality of life and adverse effects later in life.4
In New Zealand, the prevalence of current asthma symptoms is greater in Māori (28.5%) and Pacific children (25.2%)
than European children (20.7%).5 This disparity appears to be growing and continues among adults.6 Māori
and Pacific children have a greater frequency of severe asthma than European children and are more likely to be admitted
to hospital and have days off school for asthma-related illness.7 There are also disparities in clinical care
with caregivers of Māori and Pacific children reporting lower rates of receiving “easy to understand” education
about asthma and action plans than caregivers of European children.8 Māori and Pacific children also
appear less likely to receive inhaled corticosteroids for their asthma than European children.8
While the reasons for this disparity are difficult to pinpoint it is likely that the differences are influenced by
environmental factors, health literacy, housing standards/crowding and the prevalence of smoking among household members.
Difficulty in accessing primary healthcare is also likely to play a large role. The challenge is for primary healthcare
to assist in addressing these disparities, to detect asthma early and to manage it effectively, while minimising unnecessary
treatment caused by inaccurate diagnosis.
Diagnosing asthma in children
The diagnosis of asthma in children is clinical and based on history, examination and assessing the response to treatment.
While investigations such as respiratory function testing may be helpful in pointing to a diagnosis, there is no single
diagnostic test for asthma in children. The likelihood of a child having asthma is determined by how well the symptoms
fit the typical pattern of recurrent episodic symptoms, including wheeze, and whether features to suggest an alternative
diagnosis are present.3
Shortness of breath mimicking asthma
While exercise is a common trigger of asthma, exercise-induced dyspnoea and laryngeal dysfunction both produce breathlessness
and are commonly misinterpreted as asthma. These conditions may be differentiated from asthma by exercise testing.
Children with asthma will develop increased airway obstruction on spirometry if they are symptomatic with exercise.
Children with laryngeal dysfunction present with stridor which is difficult to separate from wheeze. It is usually
only present during vigorous exercise and is difficult to reproduce in a laboratory setting. Older children who are
involved in sports to a high or elite level may present with exercise-induced dyspnoea as they reach the physiologic
limits of their performance. This can be identified by observing no reduction in lung function with exercise testing.9
Children with hyperventilation syndrome may also present with symptoms similar to asthma. This syndrome can be identified
through observing the patient breathe by moving their upper chest and shoulders rather than their abdomen, particularly
when discussing symptoms, and asking about symptoms of tingling around the lips and mouth, palpitations and faintness.
A non-judgmental description of the problem and demonstration of normal abdominal breathing is usually successful in
resolving mild cases. However, referral to a physiotherapist specialised in the disorder may be required to correct
the breathing pattern. Laryngeal dysfunction and hyperventilation-syndrome may co-exist with asthma, complicating diagnosis
and management.
Symptoms of asthma
The typical clinical pattern of asthma in children is recurrent and episodic symptoms of:
- Wheezing
- Cough
- Difficulty breathing
- Chest tightness
Other factors which can help indicate asthma are:
- A personal history of atopy
- Family history of asthma or atopy
- Widespread wheeze on auscultation
- An improvement in symptoms or lung function with treatment (bronchodilators or inhaled corticosteroids)
Wheezing
Wheezing is the most familiar and useful sign for the diagnosis of asthma but is just one of a large number of respiratory
noises children make. Parents may use the term “wheezing” non-specifically to describe any respiratory noise
such as stridor or rattly breathing. Therefore, it is essential to confirm that they are describing: “a high-pitched
musical or whistling sound coming from the chest”.3 Acute, severe episodes of wheeze are most often
triggered by viral illnesses. Symptoms between severe episodes (interval symptoms) may occur in response to a trigger
such as exercise, cold or damp air and exposure to pets or with emotion and laughter. Symptoms may be worse at night
or in the early morning.
Wheeze alone is not necessarily indicative of asthma.3,9-11 Wheezing may be seen in other disorders, which
should be considered in the differential diagnosis, including: inhaled foreign body, laryngeal abnormalities, congenital
airway narrowing, chronic aspiration of feeds/gastro-oesophageal reflux, bronchiectasis, cystic fibrosis and primary
or acquired immune deficiency syndromes. Signs suggesting a disorder other than asthma include very sudden onset of
symptoms, abnormal voice or cry, continuous daily wheeze, wheeze that has been persistent since infancy, failure to
thrive, digital clubbing, a chronic moist or wet-sounding cough, persistent diarrhoea and recurrent skin or other infections.
Further investigations and treatment may be discussed with a paediatrician where necessary.
Wheeze in children aged under five years
Wheeze in response to a viral illness is common in children aged under five years. Children aged under one year with
symptoms of wheeze should generally be regarded as having bronchiolitis, or another disorder causing wheeze, and not
asthma.
Many children with episodes of wheeze commencing under age five years will have transient wheeze and resolution of
their symptoms by mid-childhood.12 However, a proportion of children will have persistent wheeze and have
asthma when they reach school-age. Unfortunately, at the time of presentation it is not possible to clinically separate
those with transient wheeze and those who will have persistent wheeze and asthma. In addition, children aged under five
years are not reliably able to perform lung function testing. Assessment in pre-school children should be directed at
eliminating other causes (by history and examination), assessing bronchodilator response to see if this is a useful
symptomatic treatment and determining whether interval symptoms are present. Symptoms that are persistent from infancy,
especially if continuous, should suggest an alternate diagnosis and discussion with a paediatrician is recommended.
The asthma cough
Cough is a common symptom of asthma, however, it is very unlikely that a cough in the absence of wheezing is due to
asthma.13 The diagnosis of “cough-variant asthma” should no longer be used. Asthma cough is often
dry and occurs in response to a trigger. During exacerbations the cough may be wet or moist-sounding due to increased
mucous production.
A chronic or frequent, wet or moist-sounding cough, particularly on waking or with exercise, is suggestive of chronic
suppurative lung disease such as bronchiectasis or cystic fibrosis rather than asthma. Children with a chronic cough
lasting longer than six weeks (other than pertussis) should be referred for a chest x-ray and further investigation.
Unlike adults, trials of treatment for asthma, reflux or hay fever in children with chronic cough, prior to performing
investigations, are not appropriate unless there are specific features suggesting an underlying cause.14
Personal and family history of atopy
A diagnosis of asthma is more likely if the child has a history of associated eczema or hay fever.9 A history
of asthma or atopy in a close relative also increases the likelihood of a diagnosis of asthma in the child. Positive
skin prick tests for aeroallergens (e.g. house dust mite, cat dander) or a raised eosinophil count may be helpful in
confirming an atopic tendency although aeroallergens are difficult to avoid except in the case of sensitisation to a
household pet.
Lung function testing and other investigations for asthma
Lung function testing in children is time-consuming and needs active participation both for the patient and the person
performing the test. Therefore, it may not be easy to perform reproducibly in primary care. In secondary care spirometry
may be used in children aged over five years to aid in diagnosing asthma, assessing treatment response and monitoring.
Children aged under five years are unlikely to produce consistent or reliable results on a spirometry test. Normal results
do not exclude asthma and many other respiratory diseases will lead to abnormal results.3
A measure of clinical responsiveness to a bronchodilator can support a diagnosis of asthma.3 This can be
assessed in primary care by observing an improvement in symptoms, work of breathing or a >12% improvement in peak expiratory
flow rate (PEFR) 20 minutes after inhaling six puffs of salbutamol administered via a spacer. Regular PEFR monitoring
is generally considered inaccurate in children. Forced expiratory volume in one second (FEV1) is a more reproducible
measure and hand-held electronic meters are now available which can measure this.
Assessing the probability of asthma
After a clinical assessment of the child’s symptoms, history and other factors, the probability of a diagnosis
of asthma can be determined.
High likelihood of asthma
Children with typical history and examination findings for asthma and without features to suggest an alternate diagnosis
have a high likelihood of asthma. Further investigations, such as chest x-ray or spirometry, are unnecessary prior to
commencing treatment. Initial treatment should be based on the severity and frequency of the asthma symptoms using the
step-wise treatment plan (see below).
The response to treatment should be assessed within two to three months. If the child has responded, then continue
treatment, titrating up and down steps as appropriate for the severity of symptoms. If the child has not responded,
discussion with a paediatrician is recommended for consideration of other diagnoses.
An intermediate likelihood of asthma
In children with wheeze, who do not fit the clinical pattern for asthma but do not have signs to suggest an alternate
diagnosis, the most practical first step may be to wait and review in one month. Alternatively, a trial of asthma treatment
may be commenced and the response assessed. Symptoms may resolve with time, therefore the return of symptoms following
the withdrawal of asthma treatment is particularly helpful in establishing a diagnosis. A positive response to bronchodilator
testing (if the child is old enough) increases the likelihood of asthma. If there is no response after one month of
treatment, discussion with a paediatrician about other diagnoses should be considered.
Low likelihood of asthma
Children who have features that suggest an alternate diagnosis and whose clinical pattern on history and examination
are not consistent with asthma have a low likelihood of asthma. Further investigation should be carried out as appropriate
and discussion with a paediatrician is recommended. Diagnostic trialling with asthma medication is unlikely to be beneficial
in this group.
Long-term management of asthma
Most guidelines recommend a step-wise approach to management in order to titrate treatment to achieve symptom control
and minimise adverse effects.
| Step 1: |
SABA alone |
| Step 2: |
A: Add ICS at low dose |
| B: Increase ICS to moderate dose |
| Step 3: |
Add LABA |
| Step 4: |
High dose ICS+LABA and/or add oral medication - consider referral to paediatrician |
| Step 5: |
Frequent or continuous oral steroids - definite referral to paediatrician |
In children assessed as likely to have asthma, treatment can be commenced with consideration of the following practice
points:
- Treatment should be commenced at the lowest step consistent with the frequency of symptoms
- Children with only intermittent symptoms can be commenced on Step One
- Children with frequent interval symptoms should be commenced on Step Two
- Assessment of severity will change with response to treatment and the level of ongoing treatment is determined by
the level of control achieved
- Children should be assessed after two to three months (or sooner if clinically indicated or on Step 4 or 5) and
treatment titrated up or down on the step-wise treatment plan according to the level of control achieved
- Treatment should be titrated to the lowest step that achieves control of symptoms
Treatment in children aged one to five years
Most children aged one to five years with wheeze will only have symptoms when acutely unwell with a viral illness.
Treatment should be symptomatic with bronchodilators during these periods. Children without interval symptoms will not
benefit from inhaled corticosteroids (ICS) and maintenance treatment is not indicated. Montelukast (a leukotriene receptor
antagonist) can be effective for these children to prevent and treat exacerbations but is not currently funded in New
Zealand.15
A proportion of children aged one to five years will have persistent or interval symptoms between viral illnesses.
These children can be managed similarly to older children with asthma but with ICS maintenance treatment directed at
control of the interval symptoms rather than preventing exacerbations.15 Treatment should be for three month
periods and, unlike in older children, should be trialled off (after tapering) rather than titrated down if interval
symptoms resolve.
Step One - short-acting beta-2 agonists
All children with symptomatic asthma should be prescribed a short-acting beta-2 agonist (SABA) such as salbutamol
or terbutaline. This is for symptomatic relief and is taken as required. Regular SABA use is not more effective than “as
needed” use. Good asthma control is associated with little or no SABA use and children with increasing or high
frequency of SABA use should have their asthma management reviewed.
Children with mild intermittent asthma should be treated with SABA only, as needed. Children with more persistent
symptoms should start on Step Two. Children who commence on Step One but are poorly controlled should progress to Step
Two.
Using two or more canisters of beta-2 agonists per month or >10-12 puffs per day is a marker of poorly controlled
asthma that puts children at risk of potentially life-threatening asthma.
Step Two - Regular preventer treatment
The addition of inhaled corticosteroids (ICS) may be beneficial for children whose symptoms are uncontrolled on Step
One or whose asthma symptoms are more severe.
There are a variety of types and strengths of ICS. As a rough guide; 200 mcg beclomethasone = 200 mcg budesonide =
100 mcg fluticasone.3 An ICS should be administered via the same inhaler device as the child’s SABA.
Children should be advised to clean their teeth or rinse their mouth after using their ICS inhaler to remove any steroid
from the oral cavity.
Initial treatment is one puff, twice daily of fluticasone 50 mcg
or beclomethasone/budesonide 100 mcg.
Initiate treatment at a low dose if the asthma symptoms are mild yet not controlled with a SABA. The lower dose inhalers
should be prescribed initially (50 mcg fluticasone or 100 mcg of beclomethasone or budesonide). The initial starting
treatment for mild symptoms should be one puff, twice daily of the lowest dose inhaler. If control is not achieved,
or symptoms are moderate or severe, the dose should be doubled to two puffs, twice daily (i.e. total daily dose 200
mcg fluticasone or 400 mcg of beclomethasone or budesonide). Adverse effects on growth and adrenal function are unlikely
at these levels. Higher doses should not be used in children aged under 12 years without trialling the addition of a
long-acting beta-2 agonist (LABA).
Inhaled chromones (e.g. sodium chromoglycate or nedocromil sodium) may be used as an alternative initial preventer
treatment in children aged over five years, but require frequent dosing which makes them second-line treatment. An oral
leukotriene antagonist (e.g. montelukast) may also be used as initial preventer treatment, particularly in children
aged under five years, but these are currently not funded.
 Best Practice tip: Ensure that patients and their caregivers understand
that they should continue to use their “preventer” until instructed otherwise, even if they experience asthma
symptoms (i.e. no longer “preventing” symptoms).
Best Practice tip: Ensure that patients and their caregivers understand
that they should continue to use their “preventer” until instructed otherwise, even if they experience asthma
symptoms (i.e. no longer “preventing” symptoms).
Step Three - Initial add-on treatment
If control is not achieved with a SABA and an ICS preventer, then additional treatment will be needed. It is recommended
that children aged under five years are referred to a paediatrician at this point. For children aged 5-12 years adding
a long-acting beta-2 agonist (LABA) should be considered. The maximum dose for a LABA in children is 50 mcg salmeterol,
twice daily or 12 mcg eformoterol, twice daily.
It is unsafe for a LABA to be used without an inhaled corticosteroid
A LABA should only be used if the child is receiving an ICS, therefore to increase compliance and safety it is recommended
that a combination LABA/ICS inhaler is prescribed (fluticasone with salmeterol or budesonide with eformoterol) where
possible. Recent changes to Special Authority restrictions now means that there is no requirement for a three month
trial period on separate LABA and ICS inhalers before prescribing a combination inhaler. Patients must, however, have
previously been treated with an ICS - at least 400 mcg/day beclomethasone or budesonide, or 200 mcg/day fluticasone
in a child aged under 12 years and at least 800 mcg/day beclomethasone or budesonide, or 500 mcg/day fluticasone in
those aged over 12 years.
 For further information see: “Schedule
changes for asthma inhalers”
For further information see: “Schedule
changes for asthma inhalers”
The response to the LABA should be assessed two to four weeks after the treatment begins. Continue treatment if there
is a positive response. However, if there is no response or a negative response proceed to Step Four and consider stopping
the LABA.
Step Four - Poor control on moderate ICS and LABA
The principle causes of persistent poor control of asthma in children are non-adherence or poor technique with inhalers,
environmental tobacco smoke exposure and psychosocial stressors.16 These issues need to be identified and
addressed before medication is increased. A home visit by the local Asthma Society or district nurse may be helpful.
Allergy testing for aeroallergens and dust-mite avoidance measures may also be useful at this stage. Although allergen
reduction and avoidance is hard to implement and is unlikely to improve asthma control, it may avoid the necessity for
further medication in some cases.
Children with persistent poor symptom control despite appropriate use of ICS and LABA require investigation for alternate
causes such as cystic fibrosis or for additional disorders which may be worsening asthma control such as hay fever and
gastro-oesophageal reflux (“asthma plus”).16 This usually involves discussion with, or referral
to, a paediatrician.
Children who are confirmed to have asthma require add-on treatment with either oral medication or an increase in their
ICS to a high dose.3 Children aged under 12 years may be given up to 200 mcg fluticasone, twice daily (i.e.
total daily dose 400 mcg) or 400 mcg of beclomethasone, twice daily (i.e. total daily dose 800 mcg) in a primary care
setting. At this dose a spacer must always be used regardless of proficiency to ensure optimal drug deposition in the
lungs and minimise oro-pharyngeal deposition. Children on doses higher than this are at risk of adrenal suppression
and adrenal crises in the event of surgery or infection and should be under the care of a paediatrician.3
Alternatives to high dose ICS are oral add-on treatment with an antihistamine, montelukast or theophylline. However,
antihistamines may only be effective for the rhinitis component, montelukast is not currently funded and theophylline
may be toxic so these medicines would usually be initiated after discussion with a paediatrician.
Step Five - Frequent or continuous oral steroid treatment
The need for frequent or continuous oral steroid treatment, such as prednisolone, in children for persistent asthma
symptoms despite maximal inhaler treatment is very unusual and has a high rate of adverse events such as poor growth,
adrenal suppression and osteoporosis. These children should be referred for assessment and ongoing monitoring by a paediatrician.
Healthy homes, healthy lungs
There are many environmental factors that can cause or exacerbate asthma in children. Tobacco smoke, damp homes,
dust mites, pets, diet and air pollution have all been associated with asthma.
Smoking in particular has been shown to exacerbate asthma. Maternal smoking during pregnancy is strongly associated
with wheezing and decreased lung function in the infant.3 Several studies have shown that when parents
stop smoking there is a decrease in asthma symptoms in children.3 Smoking cessation advice and help should
be offered to parents and other household members if there are young children in the home. The smoking status of
the household members should be recorded at all asthma check-ups.
Other potential asthma triggers should be removed where possible to create a healthy home environment. Pets should
be excluded from the house only if the child is sensitised. House dust mite allergen exposure reduction is difficult
to achieve and maintain and results from trials have shown inconsistent results on asthma control. Nonetheless, this
may be attempted if the child has persistent symptoms despite appropriate preventive treatment. |
Asthma in children with food allergy
Children with food allergy are at an increased risk of life-threatening anaphylaxis if they also have asthma.
Good control of asthma is essential in this group. These children should have an allergy action plan and carry an
adrenaline pen if needed.
 |
Choice of inhaler
Children aged four years or younger will generally require a metered dose inhaler (MDI) via a spacer with a mask. Children
should progress to using a spacer and mouthpiece without mask as soon as they are able. Some older children may wish
to use an MDI without a spacer, however, drug deposition in the lungs is poor without a spacer so this should be discouraged
where possible.
Children aged over seven years may prefer a dry powder inhaler, such as a Turbuhaler or Accuhaler, as they are less
conspicuous than a MDI with a spacer, which may increase compliance. Inhaler technique with dry powder inhalers is difficult
and the child’s ability to use the device should be observed with a placebo device or sample prior to issuing a
prescription.
Good inhaler technique is important to maximise lung deposition of medications. All health professionals caring for
children with asthma should ensure they are familiar with ideal inhaler technique so they can train and monitor their
patients correctly.
 The Asthma Foundation website has useful information for patients and
parents/caregivers on correct inhaler technique: www.asthmafoundation.org.nz/understanding_your_inhalers.php
The Asthma Foundation website has useful information for patients and
parents/caregivers on correct inhaler technique: www.asthmafoundation.org.nz/understanding_your_inhalers.php
Regular consultation and review
Children with asthma should be monitored on a regular basis, at least annually. Asthma symptom control should be checked
opportunistically at every health encounter. Inhaler technique should be checked until technique is good and then reviewed
at each asthma consultation, especially before increasing medicine doses. Practitioners should monitor and record:3
- Symptom control or symptom score, e.g. Childhood Asthma Control Test (see “Assessing symptom control”)
- Exacerbations, oral corticosteroid use and time off school due to asthma
- Inhaler technique
- Adherence to treatment (including prescription filling)
- Existence and use of self-management and personal action plans
- Growth (height and weight centile)
- Scheduled vaccinations plus annual influenza vaccine in moderate and severe cases
- Smoking status of household members
- Psychosocial stresses/caregiver/parental support
As part of the assessment, review treatment and if there is good control, step down the treatment to the lowest dose
at which effective control is maintained, which may mean reducing to Step One (i.e. SABA alone). Some children with
mild asthma only require maintenance ICS treatment during their worst time of the year. The ICS dose should be reduced
slowly by 25-50% at three month intervals. Caregivers should be given clear instructions to step back up to the previous
dose if control worsens.
Assessing symptom control
The aim of asthma treatment is to achieve complete control while minimising treatment adverse effects. Complete control
of asthma is defined as:3,9
- Few symptoms, day or night
- Minimal use of reliever medication
- No exacerbations
- No limitation of activity or play
- Normal lung function (FEV1 and PEFR >80% predicted)
- Minimal adverse effects from medication
Patients and caregivers may under-report symptoms when asked in an open/general manner, therefore it is important
to also enquire about specific symptoms. The Childhood Asthma Control Test17 can be used or Table 1 lists
suggested questions to ask parents. Peak flow diaries and symptom diaries are often unreliable and do not add to management.
Complete control of exacerbations may not be possible in children due to their frequent viral illnesses. In children
aged one to five years, aim to control the interval symptoms rather than the frequency of exacerbations.
| Table 1: Assessment of interval symptoms and asthma control. *Interval symptoms |
| Control Questions |
Indicator of good control (good control is defined as all of the following) |
| In a usual or “good” week how often does your child wake at night with cough or wheeze?* |
No waking |
| In a usual or “good” week how often does your child have wheezing?* |
Less than three times per week |
In a usual or “good” week how often does your child use their reliever (“blue inhaler”)
except before sport?*
|
Less than three times per week |
| When they are well how much can your child run around or play compared to other children the same age?* |
Same or better than other children |
| How often has your child needed oral steroids in the past 12 months? |
No more than one course in last 12 months |
| How many times has your child been admitted overnight to hospital for their asthma in the past 12 months? |
No admissions in last 12 months |
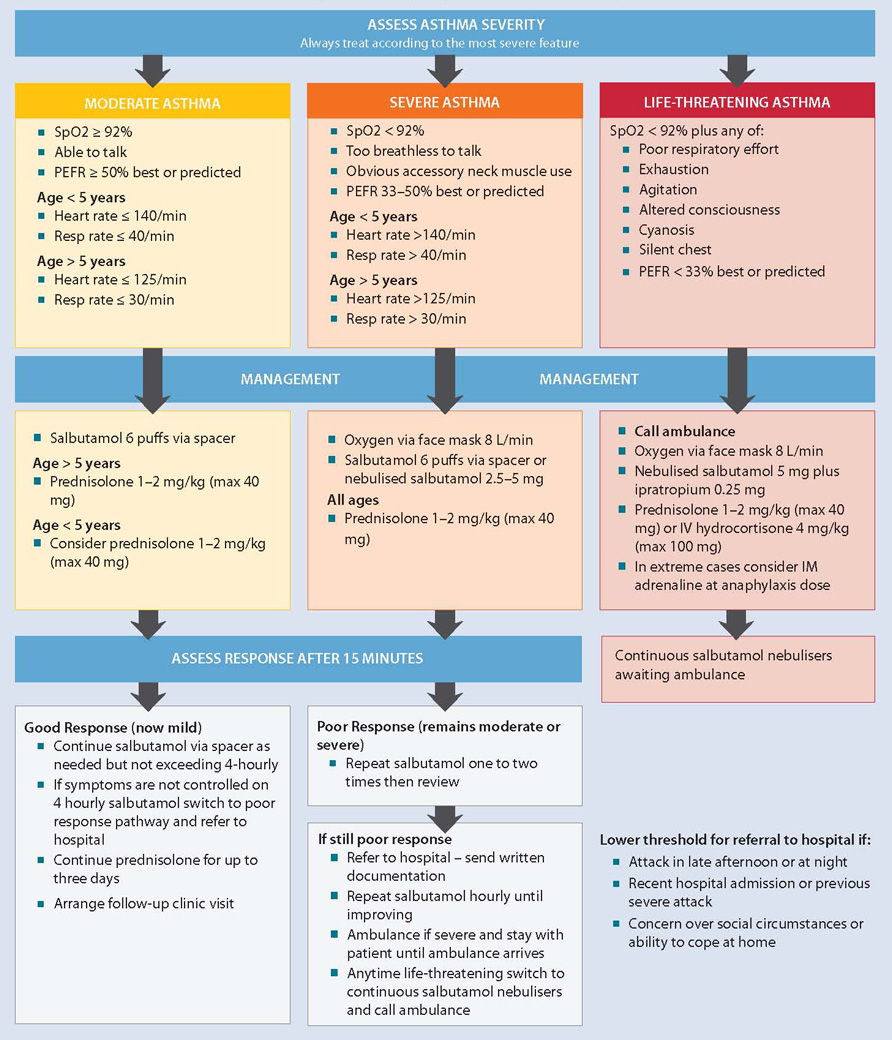
Management of acute asthma in children in primary care (Adapted from BTS/SIGN, 2011)3
ACKNOWLEDGEMENT Thank you to Dr David McNamara, Paediatric Respiratory Specialist,
Starship Hospital, Auckland for expert guidance in developing this article.