In this article 
View / Download
pdf version of this article
| Key Messages |
- Depression is common in primary care and is a major cause of disability
- Routine psychosocial assessment is the key to improving the recognition of depression. The use of simple, verbal
2 – 3 question screening tools is recommended when targeting adults at high risk for depression
- Assessment should include identification of key stresses contributing to the presentation so that these can be
addressed in the management plan
- A high index of suspicion is needed for substance use disorder as it is often harder to recognise than other mental
disorders
- K10 and PHQ-9 are useful assessment and monitoring tools
|
- Most people can be managed within primary care using a stepped care approach
- Use of self-management strategies, including e-therapy, should be encouraged and supported by practitioners
- Psychological and pharmacological therapies are equally effective for treating adults with moderate depression
- Where antidepressant therapy is planned, SSRIs are first-line treatment, with few exceptions
- Planned treatment for depression should reflect the individual’s values and preferences and the risks and benefits
of different treatment options
|
Mental disorders are extremely common with over one third of adults who attend primary care likely to have met the criteria
for a DSM-IV diagnosis within the past year.1
It is probable that a significant number of people with mental disorders are not identified. This can be due to time
and resource constraints and relatively low priority placed on patients with minimal functional impairment, especially
if they have more urgent medical problems. On the other hand, many people with a diagnosis of depression will be prescribed
antidepressants when psychological therapy alone would have been effective treatment. Adjunctive psychological therapy
with antidepressants is often neglected due to lack of available services, cost or time constraints.
Epidemiology of Mental Disorders in New Zealand.1
Mental disorders are very common in the New Zealand population. A survey conducted between 2003 and 2004, in 13,000
people aged 16 years and over, identified a 40% self-reported lifetime prevalence of a mental disorder. Overall, anxiety
disorders were the most frequently reported (lifetime prevalence rate of 25%), followed by depression and other mood disorders
(20%) and substance use disorders -predominantly alcohol (12%).
Other New Zealand studies have shown that half or more of all people who develop a serious mental disorder had experienced
the disorder by age 18 years. However, a first episode of depression can occur at any time of life with about a quarter
of first episodes reported in people aged 50 years and older. Women have a higher lifetime prevalence rate of disorder
than men, particularly major depressive disorder.
New Zealand research has also shown that people with mental disorders do use primary care services although they may
not present with these as their main problem. Primary care is well placed to provide effective management of these treatable
disorders.
Cultural Issues
There is an inextricable link between health and culture. Cultural identity is an essential component of good health
and effective services must reflect all dimensions of wellness. Central to this is recognition of whānau ora, building
on the strengths of whānau and encouraging their involvement in the process of recovery. Services will improve when
models of practice incorporate a better understanding of the importance of whānau, and the interface between culture
and clinical practices.7
Traditional Māori and Pacific perspectives challenge some commonly held assumptions, such as the focus on developing
individuality and self advocacy. There is speculation that therapies that focus on the individual may be less relevant
and less acceptable for Māori and Pacific patients, who place more emphasis on relationships beyond the individual.
1
Key cultural issues that need to be addressed in the care of all patients include: 1
- acknowledgement of environmental factors such as the role of the wider whānau
- awareness of different belief systems and lifestyles
- knowledge of existing support systems such as kaiatawhai (Māori health workers), whānau, kaumatua (elders),
ministers, consumer advisers and other specialist service providers
Kaupapa Māori Mental Health Services have wide networks and diverse expertise including the assessment of patients
with culturally specific syndromes. Similarly for Pacific peoples input from cultural advisors, leaders, healers or ministers
of religion may be needed.1
 see BPJ 14 – “Māori Mental Health” for
more information on culturally specific syndromes
see BPJ 14 – “Māori Mental Health” for
more information on culturally specific syndromes
The primary care sector is the logical place for the delivery of mental health care to Māori, Pacific Peoples and
other ethnic groups. It offers better prospects for early intervention and the management of comorbidities.
Depression in Māori and other ethnicities
Tangata Whenua
Māori have higher prevalence rates of mental health disorders overall than the rest of the population and experience
greater severity, burden and impact.2–7 Te Rau Hinengaro, the New Zealand Mental Health
Survey, reported that 3 in 5 Māori are predicted to experience a mental illness sometime in their lifetime.
6 Major
depression was the most common mood disorder among Māori with almost 1 in 3 experiencing major depression at some
point in their lives.3
Poorer access to services
There is significant unmet need among Māori with mental illness. Research has shown that less than a third of
Māori with a mental health need had any contact with mental health services and most Maori with serious or moderate
disorders had no contact with any services. For those Māori with mental health needs that did have contact, general
practice services were the services most often used. Māori tend to access mental health services at a later stage
of illness, with more severe symptoms and get less health care than others for their mental health issues relative to
need (Table 1).2
When Māori access services they tend to use mainstream providers. Therefore, it is important to ensure mainstream
services are responsive and effective in working.5 Primary health care and early intervention
can reduce the impact and severity of mental illness and addiction-related issues among Māori.2
| Table 1: Severity of mental health disorder, ethnicity, access to services for mental
health needs.2 |
| Severity |
Māori |
Non-Māori |
| |
Prevalence |
Access |
Prevalence |
Access |
| Serious |
9% |
48% |
4% |
64% |
Moderate
|
13% |
25% |
9% |
39% |
Mild
|
8% |
16% |
6% |
19% |
Rangatahi
Rangatahi (youth) are likely to be experiencing higher rates of mental illness than previous generations. Alcohol and
other substance-use disorders have contributed to this increase.6 A higher proportion
of Māori are in the age groups where mental disorders are likely to first occur, therefore the impact of unmet mental
health need among rangatahi will have a significant impact on Māori as a population.2
Pasifika
Pacific peoples have a high prevalence of mental disorders and suicidal behaviour, compounded by significant underutilisation
of health services. Pacific peoples frequently present late to services, and report difficulty accessing culturally appropriate
care and information.1
Asian
Although diverse as a group, the New Zealand Asian population shares a range of risk factors for mental disorders,
such as social isolation, language barriers and unemployment. There is a strong stigma associated with mental disorders
which may delay presentation and treatment. Somatisation (the physical manifestation of mental distress) is more common
in this population than in Western societies.1
The Mental Health Commission report on Asian mental health highlighted, in particular, the high mental health needs
of women and refugees within smaller migrant communities (e.g. Vietnamese, Indonesian), and of older migrants and refugees
suffering from pre-migration trauma, combined with the stress of adapting to a new culture. There is general recognition
of the need for general practitioners to develop skills in interacting with Asian patients and to increase their awareness
of how cultural factors influence the presentation and treatment of mental disorders in this population.1
Etiology of depression and risk factors.1
The cause of depression is multifactorial and complex. It involves the interaction of individual vulnerability with
exposure to stressors. Genetic, developmental, nutritional, endocrine, psychosocial and life stress factors can all contribute.
This complexity may explain the wide variation in clinical presentation and response to treatment.
A number of risk factors (vulnerability) and resilience factors (protective) have been described (Table 2). For example,
a history of depression in one or both parents puts their children at a three-fold increased risk of depression, whereas
good parenting (emotional warmth, cognitive stimulation) is viewed as protective in the presence of risk factors.
Table 2: Risk factors and resilience factors for depression
Common risk factors
(which could lead to vulnerability)
|
Resilience factors
(protective in the presence of risk factors) |
| Parental history of depression |
Good parenting |
| Difficult temperament as a child |
Easy temperament as a child |
| Attachment difficulties/parental neglect |
Good peer relationships |
| Family discord |
Stability in love relationships |
| Previous depression/anxiety in adulthood |
Has coped with past difficulties well |
| Ruminating over negative circumstances |
|
These concepts fit well in to the “stress vulnerability model” whereby stressful situations may trigger depression in
susceptible (vulnerable) people, but not in others who display protective traits or resilience. The concept of resilience
was once considered to be a personal trait but is now viewed as more of dynamic development process which can be used
as part of intervention and prevention programs.
Although depression can present spontaneously, there is usually an underlying factor such as work stress, job loss,
grief or relationship breakdown that can precipitate depression, especially if the person is vulnerable and has low resilience.
Alcohol, cannabis and other recreational drug use are all associated with depression. Although low socioeconomic status
alone does not appear to be predictive for development of depression, people in low socio-economic groups may be less
likely to access services and receive effective treatment.
Analysis of antidepressant use in New Zealand
Antidepressants are a mainstay of the treatment of moderate to severe depression (see Pharmacological
Management of Depression in Adults).
In this analysis of prescribing data (Figure 1) we have looked at the SSRIs (Selective Serotonin Reuptake Inhibitors)
and venlafaxine but not TCAs (Tricyclic Antidepressants) as data for the latter are confounded by their significant use
for other indications such as pain.
Fig1: New Zealanders receiving an SSRI or an SNRI (August 06 - July 07 and August 07 - July 08)
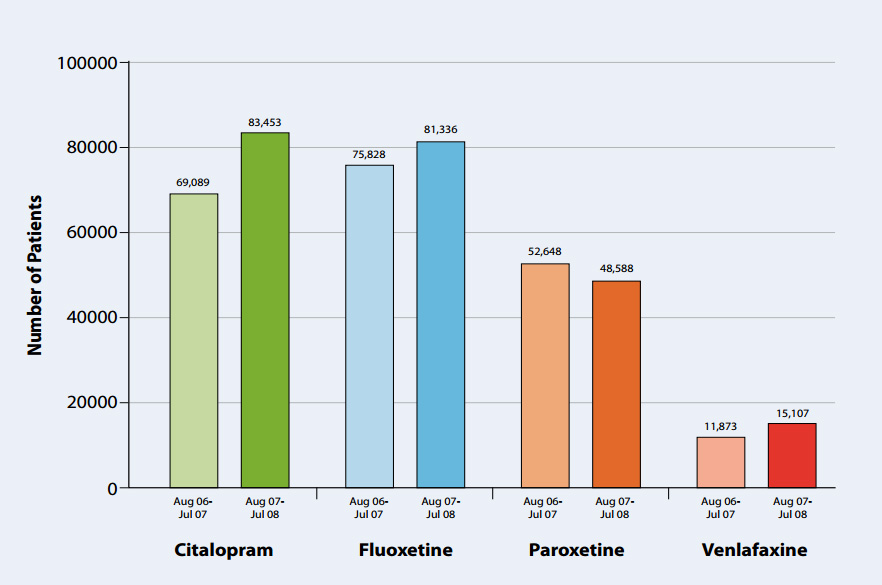
This analysis estimates the number of patients using one of the available SSRIs or venlafaxine. Two consecutive 12 month
periods have been considered (August 2006 to July 2007 and August 2007 to July 2008). The volume of venlafaxine prescribing
is influenced by its special authority status and the current restrictions on its use. However, venlafaxine use has been
steadily increasing over the last two years since vocationally trained general practitioners were given authority to prescribe
it.
Notes:
- The data are not exclusive for the treatment of depression.
- The number of patients has been estimated over the two consecutive twelve month periods analysed.
At a national level citalopram and fluoxetine are the most commonly used SSRIs whilst paroxetine appears to be the least
favoured SSRI.
Although all SSRIs are generally accepted to be similar in effectiveness, certain SSRIs may be preferred in specific
patient groups. Paroxetine has not been shown to be effective in adolescents and is linked with a higher rate of suicidal
ideation. Fluoxetine is the preferred SSRI for adolescents although this is not a licensed indication in New Zealand.
In the elderly, citalopram may be preferred due to its lower potential for interactions. Paroxetine should be avoided
in pregnancy because of reported higher rates of congenital malformations.
 References and Appendices
References and Appendices