Coeliac disease is a common but often unrecognised disorder, affecting about 1 in 100 people. Symptoms of coeliac disease are often vague and non-specific and may or may not include gastrointestinal symptoms. A low gluten diet in adults and a zero gluten diet in children often result in complete remission. However, untreated coeliac disease may be associated with long term health problems.
In this article 
View / Download pdf
version of this article
Expert Reviewers
Dr John Wyeth, Gastroenterologist and Clinical Director of Medicine, Capital & Coast DHB.
Dr Richard Steele, Clinical Immunologist and Immunopathologist, Wellington Hospital and Aotea Pathology.
Dr Simon Chin, Paediatric Gastroenterologist, Starship Hospital
Summary Points
- Coeliac disease is a common but often unrecognised disorder, affecting about 1 in 100 of the general population. Prevalence
in those with a first-degree relative with coeliac disease is about 1 in 10
- Many people presenting with coeliac disease have vague or non-specific symptoms and gastrointestinal symptoms may
even be absent
- Coeliac disease causes inflammation of the small intestine which may affect absorption of important nutrients including
iron, folic acid, calcium and fat soluble vitamins
- The diagnosis of coeliac disease should be considered in a wide range of clinical situations
- Appropriate initial tests for coeliac disease are anti-tTG and a total IgA level. The gold standard for diagnosis
is duodenal biopsy
- A zero gluten diet in children usually results in complete remission. In adults, the amount of gluten that can be
tolerated is variable. Symptomatically some adults are sensitive to extremely small amounts of gluten, while others can
tolerate low levels
- Untreated coeliac disease can be associated with the development of long term health problems although some patients
remain completely asymptomatic
Coeliac disease In adults
Coeliac disease is a chronic inflammatory condition of the small intestine in genetically susceptible individuals. It
typically presents with gastrointestinal symptoms but may also present with a wide range of non-specific symptoms.
Many studies report a prevalence of coeliac disease in adult populations as 1 in 100 but this varies with the ethnic
composition of the population being studied. A study in Canterbury, NZ gives a prevalence of 1 in 82.
1 This
is one of the highest rates reported in the literature. A 30-year review of coeliac disease in Canterbury reports that
prevalence is increasing2 but cautions that this may be due to increased
awareness, specific serological tests and availability of endoscopic duodenal biopsies, rather than a true increase.
Diagnosis can be made at any age but the majority of people present for the first time as adults.
3,4 Both
sexes can be affected by coeliac disease, although most studies indicate a higher proportion of females, particularly
during the reproductive years. The Canterbury study showed a female to male ratio of about two to one.
2
Coeliac disease occurs in almost all ethnic groups, but appears to be rare in black Africans and people of Chinese or
Japanese origin. There is little information on prevalence rates in Māori but it is generally considered to be lower than
in Europeans.
Samuel Gee, a physician at St Bartholomew's Hospital, London gave the first detailed description of coeliac disease
in 1887 although the physician, Aretaeus of Cappadocia described a malabsorptive syndrome, with persistent diarrhoea,
during the 2nd century AD.5 As the years went by, some researchers suspected
that carbohydrates were involved in the development of coeliac disease, but the specific link with wheat was not confirmed
until the 1940s, with work done by a Dutch paediatrician, Professor Willem-Karel Dicke.
6 In
1950 he published a classic thesis on the deleterious effects of wheat on the gut. Biopsies of the upper bowel have been
performed since 1956, although the use of fibre-optic endoscopy over the last 25 years has made this much easier. During
the 1970s genetic markers were identified and the haplotypes HLA-DQ2 and DQ8 which are seen in more than 99% of patients
have now been well characterised. Serological tests have made recognition of coeliac disease much easier over the last
20 years.
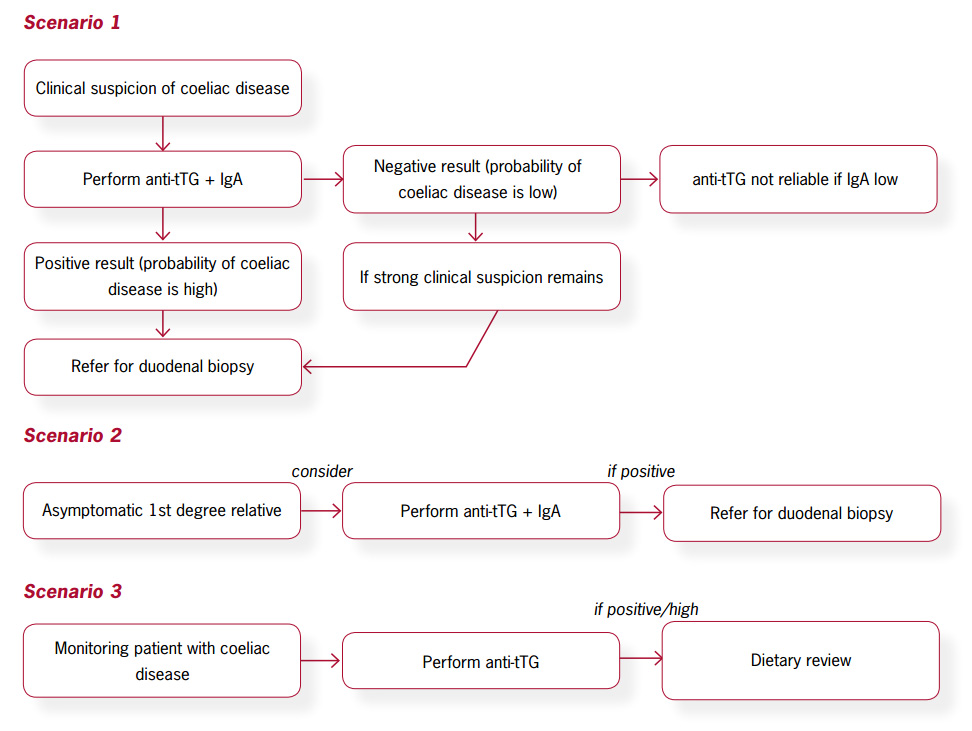
Summary of primary care investigations in coeliac disease
Coeliac disease is a chronic inflammatory condition of the small intestine in genetically susceptible
individuals
Active consideration of the diagnosis of coeliac disease in general practice will help identify those with non specific
symptoms
Coeliac disease remains under-recognised because of the non-specific way in which people with coeliac disease present
to their GP. The 'classical' presentation of coeliac disease reflects its effect on the small bowel with resulting malabsorption
producing steatorrhoea, abdominal cramps, bloating and weight loss. In practice however, people with coeliac disease
often present with diarrhoea and can be overweight. Symptoms may be similar to those attributed to irritable bowel syndrome
and some gastroenterologists routinely test people with suspected irritable bowel for coeliac disease.
4
For those diagnosed with coeliac disease as adults, it is presumed that the disease has been silent or unrecognised
during childhood. The proportion of people with latent or early symptomatic coeliac disease who go on to develop more
classical coeliac symptoms is still not known.7 Unless coeliac disease
is considered, it will remain undiagnosed.
As well as presentations caused by malabsorption, a wide range of symptoms are associated with dysmotility, autoimmunity
or the systemic effects of nutritional deficiency. Some people with coeliac disease may have temporary secondary lactose
intolerance due to the intestinal damage, which then resolves as the gut heals.
Some common presentations of coeliac disease are;
- Iron or folate deficiency anaemia3,8
- Tired all the time ('TATT') or chronic fatigue9
- Unexplained diarrhoea3,8
- Dental enamel defects10,11
- Recurrent mouth ulcers9,10
Coeliac disease is more prevalent in those with;
- First degree relative with coeliac disease (risk 1 in 10)4,8
- Type I diabetes (risk 1 in 20)4,9
- Auto-immune thyroid disease4,9
- Osteoporosis8,9
- Infertility/recurrent miscarriage4,7
- Unexplained neurological disease (particularly peripheral neuropathy, ataxia and epilepsy)
8,9
- Unexplained liver disease4,9
- Addison's disease3,9
- Sjogren's syndrome3,8
- Dermatitis herpertiformis3,9
- Down and Turner syndromes3,10
- Primary Biliary cirrhosis3,8
Appropriate initial tests
An appropriate initial test for coeliac disease is anti-tissue transglutaminase antibodies (anti-tTG) plus a total IgA
level.9,12 The patient should still be taking a gluten containing diet,
as a negative result does not exclude coeliac disease if the person has had a gluten free diet prior to testing.
13 Testing
the total IgA level is necessary because the likelihood of IgA deficiency is up to ten times higher for people with coeliac
disease than in the general population14 and this may give a misleadingly
low result to the anti-tTG level. There should be a lower threshold for performing duodenal biopsy in people with IgA
deficiency.
Some centres follow a positive anti-tTG result with a request for endomysial antibodies and some use endomysial antibodies
as the initial test. A recent review published in the BMJ found that the use of anti-tTG was adequate and cost effective.
12
Anti-gliadin antibodies are no longer routinely used for initial testing.
Serological tests are most useful as a preliminary step in testing symptomatic people and those with increased risk,
or to monitor the condition. There is some controversy in the literature as to whether asymptomatic people should be screened.
HLA typing is available but it is expensive and can be difficult to interpret. It can be useful to rule out coeliac
disease when the diagnosis is uncertain or endoscopy cannot be performed. HLA typing leads to a high false positive rate
in those identified as having the gene, resulting in unnecessary further testing and possibly gluten free diets.
If serology is equivocal and/or there is a high suspicion of coeliac disease, then upper GI endoscopy and duodenal biopsy
should be considered.
Biopsy remains the gold standard for diagnosing coeliac disease
If serology is positive, the patient should be referred to a gastroenterologist for a duodenal biopsy to confirm the
diagnosis.9 This is still considered to be the gold standard despite
the availability of the highly specific blood tests.
There are three major reasons for seeking a secure diagnosis.
- A life-long dietary change usually has a significant effect on the quality of life of people with coeliac disease
and also financial implications.
- Baseline histology can be useful for later comparison, particularly if there is no response to the change in diet,
or if the initial histology is not diagnostic of coeliac disease.
- PHARMAC currently requires a biopsy proven diagnosis to approve a special authority for gluten free products.
Other Investigations
A number of routine blood tests are required at diagnosis, during symptomatic relapse, and during pregnancy to identify
nutritional deficiencies. Tests include haemoglobin, vitamin B12, folate, iron studies, LFT's, vitamin D and
calcium. They may also be done at annual follow-up if dietary adherence needs checked or the response to the dietary change
has been poor. There is no clear agreement on when bone densitometry should be requested but a recent article suggests
symptomatic patients be referred at the time of diagnosis.15
Management of coeliac disease
Treatment is based on permanent removal of gluten from the diet
Adherence to a gluten free diet remains the key step in the management of coeliac disease. This means the exclusion
of all foods containing wheat, rye and barley. Avoiding these cereals can be difficult as they are found in bread, biscuits,
cakes, pastries, breakfast cereals, pasta, beer, and most soups, sauces and puddings.
16 Gluten
is often present as an additive or contaminant in foods.7
Prescription gluten free products include gluten free flour, bread, biscuits, and pasta. Most patients with coeliac
disease tolerate these products well. Gluten free products are now available in most supermarkets.
A low gluten diet may be tolerated by some adults with coeliac disease. Low gluten foods must have less than 20 mg of
gluten per 100 g of the food (or <2.5-5 g per day). For this category there is no prohibition on oats and malts. Children,
however, should have a zero gluten diet.
Therapeutic trials of a gluten free diet are generally not indicated without confirmation of the diagnosis, if coeliac
disease is suspected.
Removal of gluten from the diet improves symptoms and long term health for people with coeliac disease
Most adults respond promptly to a gluten free diet, showing improvement of symptoms within days or weeks. Histological
improvement usually takes many months. Once established on a gluten free diet, eating gluten-containing food can cause
an almost immediate return of symptoms and histological changes within a few weeks. There may however be no direct relationship
between the amount of gluten in the diet, the extent of the small bowel damage and the severity of the symptoms.
Referral to a dietician is important to ensure a balanced, varied gluten free diet through assessment and education.
Dieticians can also provide advice on food labelling, product availability, tips for eating out and travelling and unusual
sources of gluten (medication, sweets etc).
For most people strict adherence to a gluten free diet not only resolves the majority of presenting symptoms but also
improves the long-term health outcome. Untreated coeliac disease can lead to a number of other health problems including
poor growth in childhood, osteopenia, osteoporosis, anaemia and possibly autoimmune disorders. It has been linked to the
development of malignancy but there is still debate regarding the strength of these associations.
17,18 Experts
generally believe that adherence to a gluten free diet reduces this risk of malignancy.
Check of coeliac disease status after diagnosis
- BMI
- Symptoms, including gastrointestinal symptoms, rashes, lethargy.
- Blood tests for haemoglobin, folate, iron studies, vitamin D, calcium, vitamin B12, LFT's.
- Consider an annual check of anti-tTG to assess poor adherence to diet or relapse.
- Consider bone densitometry scan after one year of gluten free diet, during the perimenopausal period for women, age
55 for men and at any age if fracture occurs.15
- Consider testing first-degree relatives, who have a 1 in 10 chance of developing coeliac disease.
People with coeliac disease benefit from regular follow-up
After diagnosis, patients are initially seen at three and six months. If the patient is well, it is recommended that
they be reviewed annually. People with coeliac disease should be reviewed during pregnancy.
Vaccination against pneumococcus and haemophilus influenzae type b and meningococcus should be offered to the minority
of people with coeliac disease who develop hyposplenism.3,9,19 Hyposplenism
is suggested by abnormalities on the blood count and blood film.
Effective management requires a team approach
Information and support is vital to help people make the change to a gluten free diet. Adherence to a gluten free diet
is not easy, even in ideal circumstances. For individual patients this task can be complicated by family and professional
commitments, as well as peer pressure. People may find they manage well at home and when they have control over their
food choices but have difficulties while socialising and travelling. Adolescence can be a particularly difficult time.
As with any chronic condition, careful explanation, the provision of written information and ongoing encouragement are
very important. Supervision by a dietician may be essential, at least initially. People with coeliac disease are encouraged
to join the Coeliac Society of New Zealand (www.coeliac.co.nz).
Booklets listing gluten free products specific to New Zealand are available.
When to refer to a Specialist
- For duodenal biopsy and confirmation of the diagnosis
- If serology is negative but suspicion of coeliac disease remains
- Failure of a patient with coeliac disease to respond to a gluten free diet
- New symptoms arising in a patient with coeliac disease, already on a gluten free diet
Some conditions associated with coeliac disease
Osteoporosis - Most people with coeliac disease have bone mineral loss due to inadequate absorption
of calcium. Bone densitometry scan should be considered at the time of diagnosis, especially in patients with symptoms
of malabsorption.15 Adequate intake of calcium and vitamin D should be
encouraged. Patients should be advised to stop smoking, avoid excessive alcohol and take regular weight bearing exercise.
Bone densitometry is also recommended for people with coeliac disease at 55 years for men and at menopause for women.
Other causes of osteoporosis should always be considered.
Dermatitis Herpetiformis - This is a disorder characterised by an itchy blistering skin eruption
that frequently affects the knees, elbows, buttocks and back. It is found in 2-5% of people with coeliac disease.
19 Treatment
with a gluten free diet may control the dermatitis over six to twelve months, although dapsone may be needed in some cases.
Malignancy - Several types of malignancy may be increased in adults with coeliac disease.
3,20 The
strongest links are with T cell lymphomas and gastrointestinal malignancies20 specifically
small intestinal carcinoma, oesophageal and pharyngeal carcinoma.21 Interestingly
there has been recent evidence of a reduced risk of breast cancer in coeliac patients.20,22
Ulcerative Jejuno-ileitis: This is an unusual complication in which unresponsive coeliac disease
is associated with ulceration and stricture formation. This change can signify the development of T cell lymphoma.
Coeliac disease in children
The symptoms of coeliac disease vary widely depending on the age at presentation.
Classically there is a gradual failure to gain weight or a loss of weight after the introduction of cereals in a previously
well child aged 9-24 months, accompanied by anorexia, irritability, alteration in stools, abdominal distension, muscle
wasting and hypotonia. This 'text book' presentation is not the norm and in practice coeliac disease presents more frequently
in children between 5 to 9 years of age or older. A retrospective review of children diagnosed at Starship Hospital showed
a median age of 6.9 years.23
These older children present with a range of symptoms such as recurrent non specific abdominal pain, constipation, intermittent
loose stools, tiredness, mouth ulcers, vomiting and poor appetite. Significant poor growth may not be seen although sometimes
children present with short stature alone.
Coeliac disease can also present in infants younger than nine months although rarely. In this age group, vomiting, diarrhoea
and abdominal distension are more marked.
Which children require testing?
Testing is recommended for all symptomatic children.
Testing in asymptomatic children includes siblings of an index case (although because the tests may be unreliable, avoiding
this until the child is 2-3 years of age, may be preferable, unless there are symptoms), those with Type I diabetes, and
children with Down's syndrome.
How to test for coeliac disease in children
The basic approach to testing is the same as in adults. However, in young children, antibody tests are less reliable
for excluding coeliac disease. It may be appropriate to do a duodenal biopsy for every child where there is a clinical
suspicion of coeliac disease despite negative serology.
Before any testing is done, parents or caregivers need to be aware of the risks of biopsy and of untreated coeliac disease,
and the need for a lifelong gluten free diet if the tests are positive.
Children should not be started on a gluten free diet on the basis of an antibody test unless there are reasons why an
endoscopy cannot be performed.
Management in children requires a zero gluten diet
A zero gluten diet is usually recommended for children as opposed to the low gluten diet tolerated by most adults (Chin
S. personal communication, September 2007).
Oats are not recommended because their safety is still unproven and there is a risk of cross contamination from gluten
containing products. Adherence to a gluten free diet can be enhanced by involvement of caregivers and teachers in playgroup
and school environments. This will help prevent 'cheating' or experimentation with the diet, contamination (e.g. eating
play dough) or accidental exposure to gluten.11 Compliance in the teenage
years can be particularly troublesome.
Symptoms and signs found in coeliac disease in children (both GI & non GI)
10
- Persistent diarrhoea
- Abdominal pain, vomiting, constipation, abdominal distension
- Unexplained anaemia or iron deficiency
- Lassitude/weakness
- Dermatitis herpetiformis
- Dental enamel defects
- Faltering growth, idiopathic short stature
- Osteoporosis, rickets, pathological fractures
- Delayed menarche
- Recurrent aphthous ulcers
- Unexplained raised transaminases
Associated conditions (estimated lifetime prevalence)10
- Type I diabetes (≥8%)
- Selective IgA deficiency (1.7-7.7%)
- Down's, (5-12%) Williams' (8.2%) and Turner's (4.1-8.1%) syndrome
- Autoimmune thyroiditis (5-15%)
- Relatives of coeliac patient. First degree relative (10%), HLA matched sibling (30-40%), monozygotic twin (70%)
Children should be followed up regularly (12 monthly) to ensure they are growing normally and complying
with the diet and that there are no persistent symptoms. Formal dietary advice about a gluten free diet should be sought
from a paediatric dietician.
References
- Cook H, Burt M, Collett J, et al. Adult coeliac disease: Prevalence and clinical significance. J Gastroenterol Hepatol.
2000;15:1032-1036
- Cook B, Oxner R, Chapman B, et al. A thirty year (1970-1999) study of coeliac disease in the Canterbury region of
New Zealand. N Z Med J 117;1189:2004
- Clinical Resource Efficiency Support Team (Northern Ireland). Guidelines for the diagnosis and management of coeliac
disease in adults. 2006. Available from www.crestni.org.uk.
Accessed September 2007.
- Mulder C, Cellier C. Coeliac disease: changing views. Best Pract Res Clin Gastroenterol. 2005;19(3): 313-21
- Dowd B, Walker-Smith J. Gee S. Aretaeus and the coeliac affection. BMJ 1974;2:45-7
- van Berge-Henegouwen G, Mulder C. Pioneer in the gluten free diet: Willem-Karel Dicke 1905-1962, over 50 years of
gluten free diet. Gut 1993;34:1473-1475
- Mearin M, Ivarsson A, Dickey W. Coeliac disease: is it time for mass screening? Best Pract Res Clin Gastroenterol.
2005;19(3):441-52
- Green P, Rostami K, Marsh M. Diagnosis of coeliac disease. Best Pract Res Clin Gastroenterol. 2005;19(3):389-400
- Hopper A, Hadjivassiliou M, Butt S, Sanders D. Adult coeliac disease. BMJ 2007;335:558-62
- BSPGHAN Coeliac Working Group. Guideline for the Diagnosis and Management of coeliac disease in Children. 2005. Available
from
http://bspghan.org.uk/working_groups/coeliac.shtml accessed
September 2007
- Sharrett M, Cureton P. Kids and the Gluten-Free Diet. Pract Gastroenterol 2007;2:49-65
- Hopper A, Cross S, Hurlstone D et al. Pre-endoscopy serological testing for coeliac disease: evaluation of a clinical
decision tool. BMJ 2007;334(7596):729
- Primary Care Society for Gastroenterology. The management of adults with coeliac disease in primary care. 2006. Available
from www.pcsg.org.uk accessed September 2007
- Lochman I, Martis P, Burlingame R, Lochmanova A. Multiplex assays to diagnose celiac disease. Ann NY Acad Sci. 2007;1109:330-7.
- Corazza G, Stefano M, Maurino E, Bai J. Bones in coeliac disease: diagnosis and treatment. Best Pract Res Clin Gastroenterol.
2005;19(3):453-65
- Walker-Smith J, Guandaline S, Schmitz J, et al. Revised criteria for diagnosis of coeliac disease. Arch Dis Child.
1990;77:891-4
- Goddard C, Gillett H. Complications of coeliac disease: are all patients at risk? Postgrad Med J 2006;82:705-712
- Brousse N, Meijer J. Malignant complications of coeliac disease. Best Pract Res Clin Gastroenterol. 2005;19(3):401-12
- British Society of Gastroenterology. Guidelines for the management of patients with coeliac disease. 2002. Available
from www.bsg.org.uk accessed September 2007
- West J, Logan R, Smith C, et al. Malignancy and mortality in people with coeliac disease: population based cohort
study. BMJ 2004;329:716-719
- Cook, B. Coeliac Disease. Curr Ther 2001/2;42:49-53
- Anderson L, McMillan S, Monaghan P, et al. Malignancy and mortality in a population-based cohort of patients with
coeliac disease or “gluten sensitivity”. World J Gastroenterol. 2007;13(1):146-51
- Westerbeek E, Mouat S, Wesley A, Chin S. Coeliac disease diagnosed at Starship Children's Hospital: 1999-2002. N
Z Med J 2005;118(1220):U1613