Hazardous substances disease and injury notifications
A new electronic notification system has been designed for general practices to report incidents related to exposures
to hazardous substances. The system has been developed by bestpractice Decision Support (BPAC Inc) and the Centre for
Public Health Research, and is funded by the Ministry of Health.
General Practitioners in the Capital and Coast, Hutt Valley and Wairarapa regions are the first in New Zealand to use
the system to electronically notify cases of hazardous substance disease and injury, and lead poisoning, seen in primary
care. The notification system will be introduced throughout New Zealand in 2013; practices will be notified by their local
Medical Officer of Health when the module is available in their area.
What is defined as a hazardous substance injury or disease?
A hazardous substance is anything that can explode, catch fire, oxidise, corrode or be toxic to humans, as defined in
the Hazardous Substances and New Organisms Act 1996. The Act requires medical practitioners to notify cases of injury
or disease caused by exposure to a hazardous substance to the Medical Officer of Health.
There are a multitude of possibilities of exposure to hazardous substances, such as: ingestion of cleaning products
or cosmetics by children, overdose with agrichemicals, carbon monoxide poisoning, illness caused by exposure to solvents
or chlorine, contact dermatitis due to chemicals, a fireworks burn or eye injury and “huffing” (inhaling) of butane.
How should a case be notified?
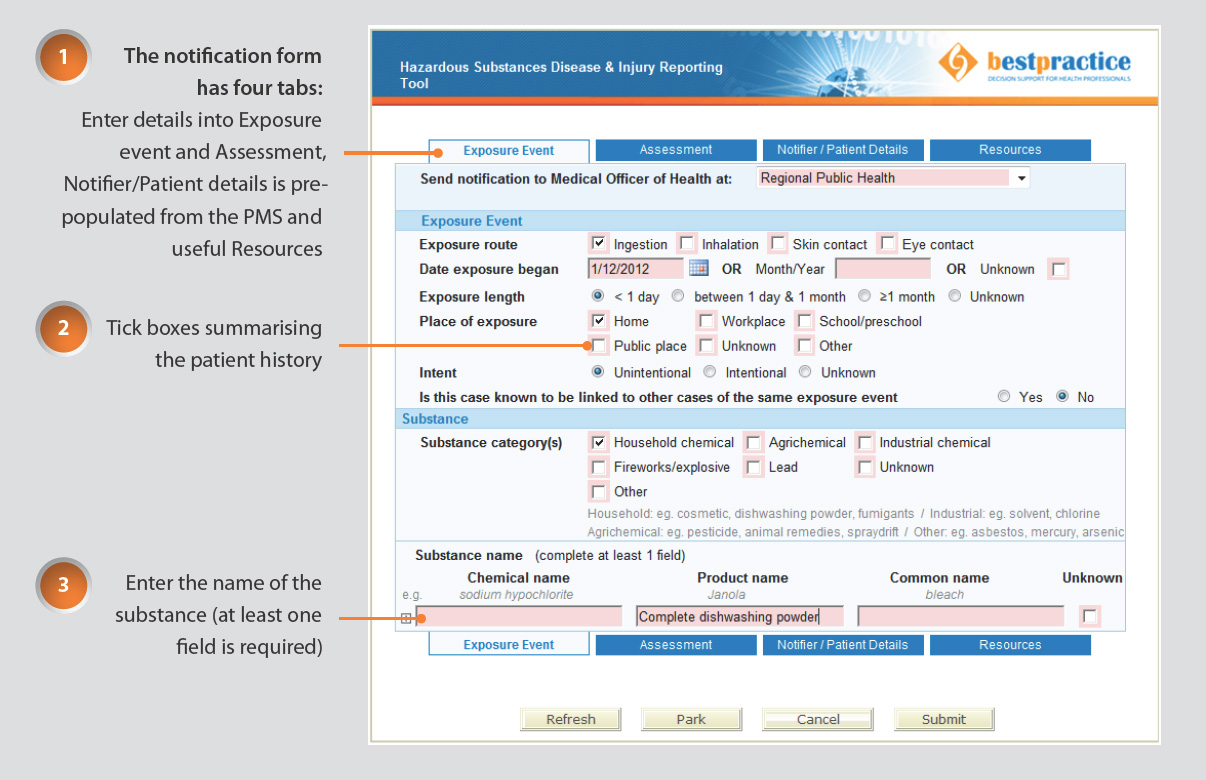
If you are in the Wellington, Hutt Valley or Wairarapa regions look for the “Hazardous Substances and Lead notifications”
module on the bestpractice Decision Support dashboard (see Figure 1 for an example). Submitting the form will send it
to your local Medical Officer of Health via a secure system.
If your practice does not currently have access to this electronic form, contact your local Public Health Unit to notify
them of a case.
Lead notifications
Cases of non-occupational lead exposure, in which a patient has a blood lead level ≥0.48 µmol/L, are required
to be notified under the Health Act 1956. The electronic form can be used for these notifications.
Chemical contamination of the environment
Cases of poisoning arising from chemical contamination of the environment (including from agrichemical spray
drift) are also required to be notified under the Health Act 1956, and this can be done via the electronic form.
Why notify?
The Medical Officer of Health and Public Health Unit staff will assess the information about the exposure and determine
if further follow-up with the patient is required.
Primary care notifications allow identification of substances which are causing harm, and can lead to controls being
put in place to prevent disease or injury. For example, exposure to lead from deteriorating lead-based paint can be reduced
through a range of remedial actions. In another example, regulatory changes have been made to the pH of dishwasher powder
following reports of injuries to children (see over page).
For further information about reporting exposures to hazardous substances, contact your local Public Health Unit, or
for more information about the new e-notification tool, contact:
Figure 1: Example of the Exposure Event tab of the notification form – ingestion of dishwashing powder (Click
image to enlarge)
Reporting of poisonings in children ingesting dishwasher powders resulted in changes to legislation
In 2005 caustic dishwasher powders were recognised as an area of public health concern due to considerable numbers
of reports of children ingesting them and requiring medical attention. Between January, 2003 and January, 2005 there
were 610 calls to the National Poisons Centre and 11 admissions to Starship Hospital. Five children required intensive
care, including intubation and multiple procedures for upper airway and oesophageal injuries.1
The reports from the National Poisons Centre and Starship Hospital were used to inform public health action (at the
time, data on dishwasher powder ingestions managed in primary care were not available). A Safekids awareness campaign
was initiated, and in 2007 the Environmental Risk Management Authority (ERMA) made changes to the group standard prohibiting
the sale in New Zealand of dishwasher powders with a pH of greater than 12.5.2 As a result of these actions
the number of children referred for medical attention following a call to the National Poisons Centre for dishwasher
powder ingestion has decreased considerably.3
The notification of hazardous substances injuries and diseases seen in primary care as part of the overall Hazardous
Substances Surveillance System, aims to identify strategies that will reduce future morbidity and mortality resulting
from exposure to hazardous substances.
References
- Bertinelli A, Hamill J, Mahadevan M, Miles F. Serious injuries from dishwasher powder ingestions in small children.
J Paed Child Health 2006;42(3):129-33.
- Safekids New Zealand. Children ingesting dishwashing powder: Update 2007. Safekids NZ; 2007. Available from: www.safekids.org.nz (Accessed
Apr, 2013).
- Environmental Risk Management Authority New Zealand (ERMA NZ). Monitoring Report 2011. Report to the Minister for
the Environment: Monitoring the effectiveness of the Hazardous Substances and New Organisms Act 1996. ERMA NZ: Wellington;
2012. Available from: www.epa.govt.nz (Accessed Apr, 2013).