In this article 
View / Download pdf version of this article

Your Practice Management System (PMS) is a powerful tool. When used well, consistently and linked to decision support software,
it can enhance understanding of a practice population’s health and help to improve patient outcomes.
Once a practice has quality information about its population, targeted care and monitoring can help improve the services
offered by the practice, increase quality of care and reduce health disparities. Your PMS is also the best tool you have
to help you meet the goals of the current PHO Performance Programme (PPP).
These goals are to:
- Improve the health of people enrolled in general practices
- Reduce inequalities in health outcomes for high need populations
Achieving PPP targets and having an information plan for the practice supports clinical governance, assists patients
at an individual level and can be financially rewarding to primary care when targets are met across the PHO as a whole.
A good example of what the PPP has achieved is illustrated in the cardiovascular disease (CVD) risk assessment indicator.
Since the CVD risk assessment indicator was introduced to the programme in 2008, assessment rates for the high need and
total population have risen from under 20% to over 67% as of June, 2013.1 From a population perspective we now have a
very good understanding of cardiovascular risk within our practices and how this relates to New Zealand as a whole.
So what are the top five things you need to make sure you and your practice team are doing to get the most out of your
PMS?
1. Make sure your demographics are correct
Ensure that the information you have about your practice population is accurate. Check that all of your patients are
identified correctly if they are part of the high need population, which comprises Māori and Pacific peoples and people
living in the lowest (NZDep deciles 9 and 10 or quintile 5) socioeconomic areas. To capture this information your PMS
needs to have recognised ethnicity codes linked to patient demographic information. To ensure your population has the
appropriate deprivation index the geo-coding functionality needs to be up to date and working correctly (see: Best
Practice Tip). This is important as the high need population accounts for a large part of the funding that your PHO receives.
Ask patients what ethnicity they identify with when they present for a consultation. Some patients may be reluctant
to indicate a preference but explaining the implications may help, i.e. that ethnicity is an important piece of health
information that impacts on clinical decisions and helps to address specific health needs.
 Best Practice Tip: To confirm your demographic coding is operating, create a new patient record and then check if dwelling
location and ethnicity coding options are automatically displayed.
Best Practice Tip: To confirm your demographic coding is operating, create a new patient record and then check if dwelling
location and ethnicity coding options are automatically displayed.
 Recognised ethnicity codes are available from:
www.dhbsharedservices.health.nz/Site/SIG/pho/Technical-Documents.aspx
Recognised ethnicity codes are available from:
www.dhbsharedservices.health.nz/Site/SIG/pho/Technical-Documents.aspx
2. Know the targets and what data is required to meet them
The correct data needs to be exported from your PMS to your PHO in order to assess performance against PPP targets.
Therefore it is important that you know what the PPP targets are and what data the targets require. There should be a
staff member within the practice who is responsible for ensuring that the correct data is being entered into the PMS.
This helps to guarantee that the effort and clinical expertise of the team is reflected in your PPP performance. It also
means that the practice receives all the funding that it’s entitled to. The PPP targets, and the data that your PHO requires
to meet them, is outlined in the document “Indicator definitions for PHOs”. An article in support of the PPP is also published
in each edition of Best Practice Journal (indicated by the PPP logo).
 To access the latest version of the indicator definitions for PHOs, see:
www.dhbsharedservices.health.nz/Site/SIG/pho/Operational-Documents.aspx
To access the latest version of the indicator definitions for PHOs, see:
www.dhbsharedservices.health.nz/Site/SIG/pho/Operational-Documents.aspx
3. Right data, right format, right place...
The coding of clinical information, using diagnostic Read codes, ensures that the recording of health information is
the same across the health care system, and that this information can be used for improving funding decisions and research.
It is also important to be aware of the codes that are used for the PPP. Recording patient outcomes and co-morbidities
is an important factor for the diabetes and ischaemic heart disease indicators. When the wrong codes are used or misused
your practice’s performance will be inaccurate and you can miss out on achieving the targets.
All practices should develop a set of commonly used, recognised codes for their PMS from the PPP data format standard
document (see below). These should be used by all clinicians within your practice.
 Best Practice Tip: Run a query in your PMS to check that the
codes you use in your PMS are approved for the purposes of PPP. If there are unapproved codes being used some systems
allow mapping of local codes to approved codes for PPP purposes.
Best Practice Tip: Run a query in your PMS to check that the
codes you use in your PMS are approved for the purposes of PPP. If there are unapproved codes being used some systems
allow mapping of local codes to approved codes for PPP purposes.
 Recognised Read codes for the purposes of PPP can be obtained from the document
“Code mappings for data transfer specification and clinical performance indicator data format standard document” available
from:
www.dhbsharedservices.health.nz/Site/SIG/pho/Technical-Documents.aspx
Recognised Read codes for the purposes of PPP can be obtained from the document
“Code mappings for data transfer specification and clinical performance indicator data format standard document” available
from:
www.dhbsharedservices.health.nz/Site/SIG/pho/Technical-Documents.aspx
The data required for the PPP indicators is stored in a number of different areas within the PMS. The PPP collects practice-based
data via an extraction process. To ensure that all the data the practice records contributes to the PPP target, it is
important that the data extractor is mapped to all sources of the information. For example, in MedTech smoking status
can be incorrectly linked to cardiovascular risk assessment, i.e. a screening code linked to an incorrect PPP code, potentially
leading to an incorrect assessment of your practice’s performance. It is important to check that the extractor mechanism
has been mapped correctly to extract all the information stored within your system.
 To ensure that your PMS’s data extractor is set-up correctly contact your local
PHO.
To ensure that your PMS’s data extractor is set-up correctly contact your local
PHO.
4. Implement practice-wide processes
To get the most out of your PMS it is important that everyone in the practice is using it the same way. Good practice-wide
processes help to structure tasks across the practice. Identify key team members who have the responsibility for ensuring
that patients are registered properly and have an identified geocode, and that the practice is receiving funding for the
patients. A process should also be put in place to ensure that patients who have not been seen in the last three years,
and are about to be removed from the practice register, are contacted and offered an assessment. Patients who are due
for an intervention, e.g. a CVD risk assessment or cervical smear, should be recalled and followed up if they do not respond
initially. Investigation results, such as mammography reports, should be captured in the system so that recalls are automatically
generated for follow-up. Together, such processes should increase the PPP achievement rate for the practice.
As an example of a good practice-wide process, set a policy for clinicians to ask everyone who comes to the practice
about their smoking status and record the information so that it can be captured by the PPP. This can dramatically improve
the “smoking status recorded” indicator. This could be introduced as a team goal. For example, review the number of times
each staff member records a smoking status or a CVD Risk assessment. The clinician who has achieved the most can then
be rewarded at the end of each month. This approach creates a healthy competition within the team to achieve better recording
of information.
5. Make use of electronic support tools
Support tools are usually “add-on” applications that are integrated into the PMS. Their main purpose is to ensure best
practice is followed and any missing data is collected. These tools help practices to maximise the benefits of their PMS.
Support tools have three main functions:
- Dashboard or patient prompt tools
- Electronic decision support tools
- Reporting applications
When all of these support tools are set-up to work together, consistency occurs with coding and the storing of information
within primary care systems. The data contained in the PMS then has greater meaning and ensures more accurate population
information. Clinicians can then focus on clinical issues and not be concerned about how to record and check that the
information for the PPP is accurate and retrievable.
When PHOs implement these integrated tools across their regions a greater understanding of population health and practice
performance is captured. Practices implementing good processes can be identified and their methods can be shared with
other practices to adopt the successful approaches.
Dashboard or patient prompt tools
When the patient’s file is opened on the PMS the prompting tools assess the information within the systems and look
for missing information, such as smoking status, or whether previously collected information is now out of date, such
as looking for a cardiovascular risk within the last five years or a cervical smear in the last three years. These tools
are becoming increasingly more sophisticated and can now highlight progressive chronic kidney disease and integrate with
electronic decision support tools and enable the use of electronic health pathways and smart referrals.
Electronic decision support
Decision support tools are integrated into your PMS to help facilitate cardiovascular risk and diabetes assessments.
They have evolved from simple data collection tools for administrative purposes into key solutions for providing best
practice guidance on managing cardiovascular disease, diabetes, chronic kidney disease and many other long-term conditions.
Decision support applications are enhancing the role of primary care.
Reporting applications
Population reporting applications give practices and PHOs an understanding of disease prevalence and associated co-morbidities.
They provide information on how practices are performing in relation to the PPP and to other practices. The ability of
the reporting applications to receive data on a daily basis helps practices to reflect more accurately on their achievements
and to visualise their improvement when they change or introduce new processes into their practice.
Practices can clearly identify patients who have not received an intervention or require review. Using the information
within these reports allows practices to schedule appointments for patient with long-term conditions and target care for
those at greatest risk.

Common coding conundrums
Coding of health information is a bit like marmite; you either love it or hate it! Coding systems can be complex, and
poor understanding of how coding systems are structured can lead to errors. Conversely, improved coding leads to more
accurate reporting of health information, more efficient practice systems and, in the case of the PPP, improves your performance
and funding.
Coding of information allows for the standardisation of clinical terms, e.g. the terms “heart attack” and “acute myocardial
infarction” are linked by the mapping of these two terms to a single code root: in the Read thesaurus this is G30. The
different terms, heart attack and acute myocardial infarction, are extensions of the code G30. Extensions or synonyms
are defined by the numbers after the period as illustrated below:
G30.14Heart Attack
G30.00Acute Myocardial Infarction
The linking of these medical terms provides uniformity through the G30 Read code. Uniformity then allows for data to
be collated and used for evaluation of care, reporting, statistics, funding, planning and clinical research.
However, problems can arise when coding is not well understood. Common issues that occur in practice include:
1. Codes are used that are not recognised by the PPP
For example, the smoking code 137.00 – Tobacco consumption is not part of the code used to identify smoking status.
The synonym of the code 137, 137.11, is called “Smoker – amount smoked”. This is frequently recorded in practice as follows:
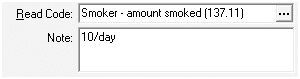
This code is not extracted for the PPP so will not be recognised. The other mistake is the use of the note section to change the meaning or
reference of the code being used. A more appropriate code would be to use:
1374.00 Moderate smoker – 10–19 cigarettes/day
2. Changing the meaning of the code by adding text to the note section
If the note section is used in an attempt to change the meaning of the code, the addition is lost when the code is interpreted
and aggregated by a computer. This will lead to unreliable reports and performance.
For example:
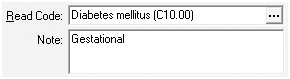
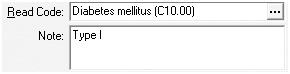
Or
In the first example the patient will be included in the PPP reports, but should not be as people with gestational diabetes
are excluded from the PPP.
In the second example there will be no affect on the PPP reports, but there would be no ability to differentiate between
two different types of diabetes with two different pathophysiologies if all patients with diabetes were coded with the
C10 code and only identified by type within the note section.
A more precise approach which would lead to an improved understanding of population health and more accurate PPP reports
would be to use the following codes:
L1809 Gestational diabetes
C108 Type I diabetes mellitus
C109 Type II diabetes mellitus
3. The over-use of local codes
Some practices have devised their own codes when the current coding system does not match their needs. In the example
below, at first glance everything looks fine, the term clearly refers to an individual with type I diabetes, but the code
linked to the term is a made up local code and will not be recognised by the PPP.
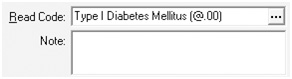
Local codes are best avoided unless they have been adopted nationally as in the case of the new ‘ZP’ smoking codes.
Acknowledgement
Thank you to Glen Knol, Facilitator, bestpractice Decision Support, Dunedin for contributing
to the development of this article.
Reference
- PHO Performance Programme. National Summary of PHO Performance: 1 April 2013 - 30 June 2013. 2013.
Available from: www.dhbsharedservices.health.nz (Accessed Oct, 2013)