In this article 
View / Download
pdf version of this article
| Key concepts: |
- Māori and Pacific women have lower rates of breast screening and as a result have a higher mortality rate from
breast cancer
- General practice can play a key role in addressing this inequality by ensuring all eligible women are assisted to
enrol and participate in the breast screening programme
- Practices that have made a commitment to increasing breast screening rates for Māori and Pacific women are
finding they can make significant improvements in screening rates
|
Breast cancer is the most commonly diagnosed cancer in women and is a leading cause of cancer death in New Zealand women.
A woman’s chance of developing breast cancer increases with age. Approximately 70% of women diagnosed with breast
cancer are aged over 50 years and of those who die from breast cancer, 80% are aged 50 years and over.1
The incidence of breast cancer is similar for all women. However Māori and Pacific women are over 1.5 times more
likely to die as a result of breast cancer compared to other women in New Zealand (Figure 1).2 Māori and
Pacific women are diagnosed later than other ethnic groups with larger, higher grade tumours with more lymph nodes involved.3
The national target for breast screening is for 70% of all eligible women to have been screened within a two year screening
interval. This target has not been met for any ethnic group, and there are significant differences in screening rates
between Māori and Pacific women, and other women (Figure 2).
General practice has a key role in improving breast screening rates in Māori and Pacific women
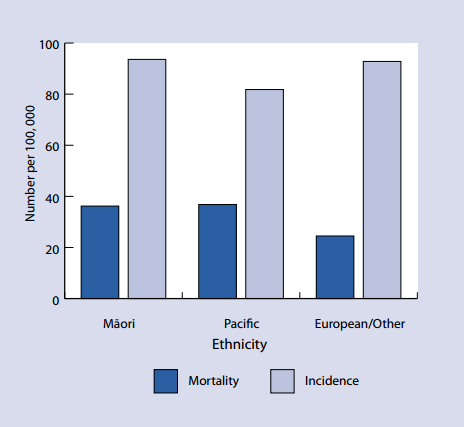
Figure 1: Breast cancer incidence and mortality2
|
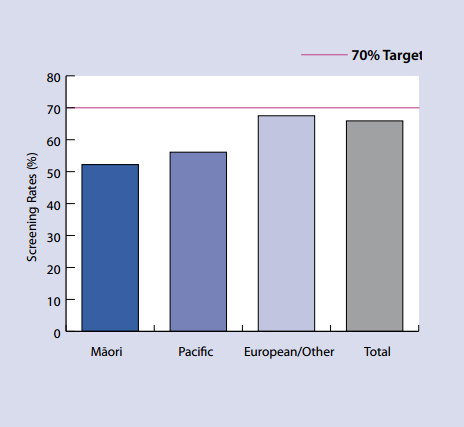
Figure 2: Breast screening coverage by ethnicity (women aged 50 to 69 years, June 2007–09)
|
The aim of breast screening is to identify breast cancers at an early stage, allowing treatment to commence sooner,
leading to reduced morbidity and mortality. Many women miss out on breast screening because there is no national system
available which identifies and enrols them for screening as they become eligible.
The challenge, in the absence of a national system is for individual general practices to commit to ensuring all eligible
women in their practice population are encouraged and assisted to enrol in the breast screening programme.
What can your practice do?
Be able to identify and contact eligible women in your practice:
- Use your practice management system to identify and flag eligible women
- Send invitations that encourage women to enrol for breast screening
- Ask women about their breast screening status and record it in their notes in a way that is accessible/searchable
Reflect on barriers that may prevent women accessing screening. Strategies to overcome some of the common barriers include:
- Encourage all practice staff to have an understanding of the barriers to breast screening and be aware of the practice’s
strategies to overcome these barriers
- Actively assist women to enrol with BreastScreen Aotearoa and to make an appointment for a mammogram
- Ensure eligible women know that breast screening is free
- Provide women with appropriate information about breast screening
- Allow enough time to talk through a woman’s concerns
- Support women who are shy or apprehensive
- Ensure women know they can bring a support person
Ensure your practice is aware of breast screening services in your area:
- Do you know when the next mobile breast screening vehicle is in your area? This information is available from
www.nsu.govt.nz/
Click on your region, then select “mobile screening unit schedule” to bring up a list of times, dates and
locations of mobile screening. Consider printing this out and ensuring all practice staff are aware when the mobile screening
unit is in your community.
Consider coordinating with other practices as it is important to ensure the potential of the mobile breast screening
unit is maximised when it is in your community.
Ensure practice staff are aware of transport options in your area. Your PHO may have a financial assistance programme
which could be used to help cover the cost of transport, if this is a barrier.
To enrol women with BreastScreen Aotearoa:
- Telephone BreastScreen Aotearoa on 0800 270 200
- Complete the online form at
www.nsu.govt.nz/Current-NSU-Programmes/1528.asp
- Post or fax an enrolment form to the BreastScreen Aotearoa lead provider in your area
Who is eligible for breast screening in New Zealand?
As part of the New Zealand breast screening programme, a mammogram is performed every two years. This is provided
throughout the country by BreastScreen Aotearoa and is free of charge. To be eligible women must:4
- Be aged 45 to 69 years of age
- Have no symptoms of breast cancer
- Have not had a mammogram in the previous 12 months
- Not be pregnant
- Be eligible for public health services in New Zealand
(www.moh.govt.nz/eligibility)
Women who have had breast cancer in the past, but now meet the above requirements can enter or re-enter the BreastScreen
Aotearoa programme, five years from when their breast cancer was first diagnosed.
Raising the profile of breast screening in a practice
Practice Nurse, Waitemata DHB
We have had huge success, working in partnership with BreastScreen Aotearoa. Before the mobile caravan
is due to come to our area, we have regular meetings and brainstorms with other health providers on how to reach eligible
women. Together with BreastScreen Aotearoa we do an audit of our 45-69 year old female patients that are not enrolled
with BreastScreen Aotearoa each year. We then rule out the patients who have gone privately, declined, or have other health
issues preventing them from having a mammogram through breast screening.
BreastScreen Aotearoa gives us appointment times and we then phone these woman and enrol then over the
phone and book them an appointment on the spot. We target the high needs Māori and Pacific women first. This method
has been very successful as it means the patients do not have to phone BreastScreen Aotearoa and arrange it themselves.
We also ask if there are any transport issues and can arrange transport for them through our local Māori Health provider
or other community initiatives. The initial phone contact is useful to allay some women’s fears and to answer questions
about mammograms. BreastScreen Aotearoa reimbursed the practice for the time and phone call costs to do this.
Through this initiative we have improved our screening rates dramatically and it continues to improve
each year. BreastScreen Aotearoa provided all the staff in the practice with shirts and fleeces with BreastScreen Aotearoa
and the age limits written on them. It was surprising how many patients saw the shirts and were prompted to ask questions
and subsequently go for a mammogram. Raising the profile of breast screening and working closely together with BreastScreen
Aotearoa and other community groups seems to be the key.
PATIENT INFORMATION supporting the breast screening programme, in a variety of languages, and free
of charge and can be ordered online at: www.healthed.govt.nz
Increasing the uptake of breast screening in Māori women5
A general practitioner led initiative at the Te Whānau ā Apanui Community Health Service (TWAACH) in the Eastern
Bay of Plenty, has been successful in increasing the uptake of breast cancer screening in a predominantly Māori community
(approximately 90% Māori). Screening rates have increased from 45% of eligible Māori women in 2003 to about
98% in both 2005 and 2007.
The starting point was agreement from the general practice team to set a goal and a clear focus on improving breast
cancer screening participation rates for their predominantly Māori population. Changes were achieved using the current
staff and resources, but with local input, flexibility and collaboration between existing services.
The strategy had two broad aims – to increase local involvement and to reduce barriers to participation and included
the following:
- The PMS system was used to create a master list of eligible women who were sent letters inviting them to enrol for
breast screening
- TWAACH received agreement from Breast Screening Aotearoa to coordinate registration and make appointments. Staff were
encouraged to be flexible and resourceful to ensure no one was turned away and all available appointments were filled.
Staff were able to arrange group bookings for women who lived in the same household, whānau (family) group or area
- Two weeks prior to screening, telephone or face-to-face contact was made with all women who had not enrolled, breast
screening discussed and enrollment encouraged
- The day before their appointment women were contacted to confirm the appointment time and assistance was offered if
there were going to be difficulties in attending
- Women who “dropped in” were not turned away. Instead there was flexibility to allow them to be enrolled
and screened
- Women who did not arrive were contacted and offered further assistance and a rescheduled appointment at another mobile
unit or fixed site
Issues that were predicted to affect participation in the screening programme were identified through discussions with
practice staff and patients. These included transport difficulties, travel time, inconvenience, concern, fear and the
influence of negative reports from other women. A number of strategies were used by TWAACH to help overcome these barriers
to participation. They found:
- Booking directly with women helped overcome issues with an unreliable rural mail delivery, literacy, and competing
priorities
- Arranging group bookings for women who lived in the same household, whānau (family) group or area, helped with
travel difficulties as well as providing support
- Providing a cup of tea afterwards allowed the opportunity for women to share and debrief with each other, resulting
in positive feedback and encouragement of other whānau to attend.
TWAACH also followed up abnormal results.
Breast screening was strongly advocated in the community. The staff of TWAACH were encouraged to promote breast screening
at any opportunity. The dates of the mobile unit visits were advertised repeatedly in the TWAACH newsletter, marae and
local businesses.
Breast screening was promoted and information provided at a number of community events. Two well known women who had
previously been diagnosed with breast cancer shared their stories and support of the breast screening programme. Registration
forms were available at these events.

PHO performance programme and breast screening
Breast cancer screening coverage is included as one of the clinical indicators for the PHO performance programme. The
overall goal is to achieve a breast screening rate of greater than 70% for all high needs women aged 50 to 64 years.
A high needs woman is defined as an enrolee who is Māori, Pacific or living in a New Zealand deprivation decile
area 9 or 10.
Make it count
Calculation of breast screening rates is made using data extracted from the PHO enrolment data base and the
National Screening Unit breast screening data base. It is important all demographic information collected is as complete
and accurate as possible.
Ethnicity
The key points of effective ethnicity data collection are:
- Patients must identify their own ethnicity
- Patients may choose multiple ethnicities
- Patients may choose not to answer the question
- Ethnicity data can be collected in person, by telephone, by post or by proxy
- The standard ethnicity question helps to maintain consistency of responses and quality of data
See BPJ 9, October 2007 “Making Ethnicity Data count”.
NHI number: Ensure the NHI number is included. A valid NHI means the data can be matched with the
NSU and PHO enrolment databases, to ensure it is counted.
Gender: Ensure gender is recorded, as an “unknown” gender is converted to “male”,
and will not be counted.
Declines: Women who decline to be screened are not counted. This should not affect achievement of
targets, as they are based on improvement rather than absolute numbers.
Age band extension: The BreastScreen Aotearoa programme was extended to include women aged 45-49 and
65-69 from 1 July 2005. At this point in time there is insufficient data for measurement of these age bands. As a result,
women aged 50 to 64 are only measured for this indicator.
Acknowledgement
Thank you to Dr Nina Scott, Māori Strategic Advisor, National Screening Unit, Wellington for
expert guidance in developing this article.
References
- New Zealand Health Information Service. Cancer: New registrations and deaths 2004. Ministry of Health, Wellington,
2007.
- Dachs G, Currie M, McKenzie F, et al. Cancer disparities in indigenous Polynesian populations: Māori, Native
Hawaiians and Pacific people. Lancet Oncol 2008; 9:473-84.
- Weston M, Moss D, Stewart J, Hill A. Differences in breast cancer biological characteristics between ethnic groups
in New Zealand. Breast Cancer Res Treat 2008 Oct;111(3):555-8.
- National Screening Unit. BreastScreen Aotearoa. Available from: www.nsu.govt.nz/ (Accessed
September 2009)
- Thomson R, Crengle S, Lawrenson R. Improving participation in breast screening in a rural general practice with a
predominately Māori population. N Z Med J 2009; 122:1291.